The Pathophysiology And Therapeutic Intervention Of Migraine
The Pathophysiology and Therapeutic Intervention of Migraine

Introduction
Migraine, a prevalent neurological disorder characterized by recurrent headaches, sensory disturbances, and autonomic dysregulation, poses a significant global health burden. We are going to provide a comprehensive review citing out the unique pathophysiological mechanisms underlying migraine and discuss the evolving landscape of therapeutic interventions.
Understanding Migraine Pathophysiology

1. Genetic Predisposition
Migraine exhibits a strong familial aggregation, suggesting a genetic component in its etiology. Genome-wide association studies have identified numerous susceptibility loci implicated in migraine susceptibility, including genes involved in neuronal excitability, neurotransmitter release, and vascular regulation.
2.Environmental Factors
Environmental triggers such as stress, sleep disturbances, hormonal fluctuations, dietary factors, and sensory stimuli play a crucial role in migraine onset and exacerbation. These triggers interact with genetic predispositions to precipitate migraine attacks, underscoring the threshold nature of the disorder.
Sensory Processing Abnormalities
Migraine pathophysiology revolves around the concept of a cyclic sensory threshold model, wherein aberrant processing of sensory inputs leads to hypersensitivity and pain amplification. Dysregulation of cortical excitability, thalamocortical networks, and descending pain modulatory pathways contribute to the sensory manifestations of migraine.
Phases of Migraine

Migraine progression is characterized by distinct phases, including premonitory, aura, pain, and postdrome phase, each associated with specific neurophysiological changes. The premonitory phase, marked by various symptoms preceding the headache, reflects hypothalamic and brainstem activation. Aura, a transient neurological phenomenon, involves cortical spreading depression and cortical spreading depolarization, leading to visual, sensory, or motor disturbances. The pain phase, mediated by trigeminal vascular activation and central sensitization, culminates into headache and associated symptoms. The postdrome phase, characterized by residual symptoms following headache resolution, implicates persistent alterations in cortical and brainstem function.
a) Trigeminal vascular System

Central to migraine pathophysiology is the trigeminal vascular system, comprising peripheral trigeminal afferents and central brain nuclei involved in pain processing. Activation of trigeminal vascular pathways, mediated by neuropeptides like Calcitonin gene-related peptide, substance P, and neurokinin A, initiates neurogenic inflammation and sensitization of meningeal nociceptors, contributing to headache generation.
b) Brainstem Nuclei
Brainstem regions, including the dorsolateral pons, periaqueductal gray, and locus coeruleus, serve as crucial modulators of trigeminal vascular transmission. Dysregulation of brainstem nuclei leads to unbearable pain processing and autonomic dysfunction, characteristic of migraine attacks.
c) Hypothalamic Involvement
The hypothalamus plays an important role in migraine initiation and progression, integrating nociceptive, autonomic, and circadian inputs. Dysregulation of hypothalamic neurotransmitters, including orexin, serotonin, and dopamine, contributes to migraine susceptibility and triggers stress-induced attacks.
d) Thalamic Dysfunction
The thalamus, a key relay station in sensory processing, exhibits structural and functional abnormalities in migraine. Altered thalamocortical connectivity, thalamic excitability, and neurotransmitter imbalance contribute to central sensitization, photophobia, and allodynia, hallmark features of migraine.
e) Cortical Alterations
Beyond aura generation, the cerebral cortex demonstrates widespread abnormalities in migraineurs, including changes in cortical thickness, gray matter volume, and functional connectivity. Genetic variants associated with glutamatergic neurotransmission and cortical excitability further implicate cortical dysfunction in migraine pathophysiology.
Therapeutic Approaches

a) Acute Treatments
Triptans, serotonin receptor agonists, have long been the mainstay of acute migraine therapy. However, emerging classes of medications, including ditans and gepants, offer alternative treatment options with improved tolerability and efficacy. Lasmiditan, a selective 5-HT1F receptor agonist, provides rapid relief without vasoconstrictive effects, making it suitable for patients with contraindications to triptans. Gepants, small-molecule CGRP receptor antagonists, block CGRP-mediated vasodilation and neurogenic inflammation, offering effective pain relief without cardiovascular risks.
b) Preventive Treatments
Monoclonal antibodies targeting CGRP or its receptors represent a breakthrough in migraine prevention, providing sustained efficacy with monthly or quarterly dosing regimens. Erenumab, fremanezumab, and galcanezumab have demonstrated superior efficacy compared to placebo in reducing migraine frequency and severity, with favorable safety profiles. Gepants such as atogepant and Rimegepant offer additional options for migraine prophylaxis, particularly in patients intolerant to traditional preventive therapies.
c) Neuromodulation Techniques
Non-invasive neuromodulation modalities, including transcranial magnetic stimulation and transcutaneous supraorbital nerve stimulation, offer adjunctive therapeutic options for acute migraine management. TMS delivers magnetic pulses to cortical regions implicated in migraine pathophysiology, modulating cortical excitability and pain perception. tSNS targets the supraorbital nerve, inhibiting nociceptive transmission and providing rapid pain relief without systemic side effects. Additionally, vagus nerve stimulation (VNS) offers a promising approach for both acute and preventive migraine treatment, modulating autonomic function and central pain processing.
Conclusion
In conclusion, migraine represents a complex neurological disorder with a diverse clinical manifestations. Advances in our understanding of migraine pathophysiology have paved the way for the development of novel therapeutic agents targeting key molecular and neural pathways. By understanding the interplay between genetic predisposition, sensory processing abnormalities, and central pain modulation, clinicians can tailor treatment strategies to individual patient needs, optimizing therapeutic outcomes and improving quality of life for migraine patients worldwide. Continued research efforts and clinical innovations hold the promise of further advancements in migraine management, underscoring the collective commitment to alleviating the global burden of this devastating condition.
Understanding the pathophysiology of migraine is crucial for effective management, and this comprehensive analysis sheds light on the complex mechanisms underlying this neurological disorder. For medical students facing challenges in studying migraine or any other medical topic, seeking professional help from Expert Academic Assignment Help can provide valuable guidance and support. With our expert assistance, students can overcome obstacles and excel in their academic endeavors. Contact us at expertassignment46@gmail.com to elevate your understanding and mastery of medical concepts.
More Posts from Expertacademicassignmenthelp and Others
The 12 Most Interesting Facts about Nursing

The nursing profession is a cornerstone of the healthcare system, rich in history, filled with unique facts, and bolstered by surprising statistics that highlight its evolution and impact. Whether you’re a registered nurse, nurse practitioner, nurse’s assistant, or involved in nurse staffing, there is always more to learn about this vital field. Here, we indulge into 12 intriguing facts about nursing that might surprise even those within the industry.
1. Nursing’s Ancient Origins

The earliest records of nursing date back to 300 A.D. in the Roman Empire, where nurses operated in what were considered hospitals at the time. These early healthcare institutions, known as valetudinaria, provided care primarily to soldiers and slaves. Nursing during this period was rudimentary and primarily focused on basic care and comfort.
The practice of nursing evolved significantly during the Middle Ages. Monastic orders, particularly in Europe, took on the role of caregivers. Monks and nuns provided care in hospices and infirmaries, laying the groundwork for modern nursing. The evolution continued with the establishment of more structured medical and nursing practices in response to the Black Death in the 14th century. These historical roots underscore the longstanding tradition of compassion and care in nursing.
2. Florence Nightingale’s Pioneering Influence

Florence Nightingale, often referred to as the founder of modern nursing, played a major role in transforming the profession. Born into a wealthy British family, Nightingale defied societal expectations to pursue a career in nursing. Her work during the Crimean War (1853–1856) brought her international acclaim. She was appalled by the unsanitary conditions and high mortality rates in military hospitals and implemented rigorous hygiene practices, significantly reducing the death rate.
Nightingale’s contributions extended beyond the battlefield. She established the Nightingale Training School for Nurses in 1860 at St. Thomas’ Hospital in London, emphasizing the importance of formal education and training for nurses. Her book, “Notes on Nursing: What It Is and What It Is Not,” became a seminal text in nursing education. Nightingale’s legacy includes her pioneering use of statistical analysis to advocate for healthcare reform, showcasing the impact of evidence-based practice.
3. The First Nursing School
The establishment of the Bellevue Hospital School of Nursing in New York City in 1873 marked a significant milestone in American nursing history. Inspired by Florence Nightingale’s principles, the school offered a one-year program that combined theoretical instruction with practical experience. This model set the standard for future nursing education.
Bellevue’s success prompted the establishment of other nursing schools, such as the New England Hospital for Women and Children (now part of the Boston Medical Center) and Massachusetts General Hospital’s nursing school. These institutions played a crucial role in professionalizing nursing and raising the standards of patient care. The emphasis on rigorous training and education helped transform nursing into a respected and essential profession.
4. The Physical Demands of Nursing
Nurses are known for their dedication and hard work, but the physical demands of the profession are often underestimated. On average, nurses walk four to five miles during a typical 12-hour shift, which is double the daily walking distance of most people. This constant movement is necessary to provide timely and effective care to patients, but it also highlights the physical challenges nurses face.
The demanding nature of nursing underscores the importance of proper footwear and ergonomics in the workplace. Comfortable, supportive shoes can help prevent injuries and reduce fatigue, enabling nurses to perform their duties effectively. Additionally, the physical activity associated with nursing contributes to overall health, but it also necessitates a focus on self-care and occupational health strategies to mitigate the risk of long-term musculoskeletal issues.
5. Dominance in Healthcare Education
Nursing is a dominant field within healthcare education, with approximately 50% of students in healthcare-related programs pursuing nursing degrees. This significant representation reflects the critical role nurses play in the healthcare system. The demand for nursing education has led to the development of numerous undergraduate and graduate programs, offering specialized training in various areas such as pediatric nursing, geriatric nursing, and critical care.
The strong support network among nursing students and professionals fosters a collaborative learning environment. Nursing programs emphasize not only clinical skills but also the development of critical thinking, communication, and leadership abilities. This comprehensive approach ensures that nursing graduates are well-prepared to meet the diverse and complex needs of patients.
6. Top Nursing Jobs
Nursing offers a wide range of career opportunities, and several nursing roles are consistently ranked among the top jobs in the United States. According to U.S. News & World Report, three nursing roles were among the top 40 jobs in 2021: registered nurses (ranked 37th), nurse anesthetists (ranked 39th), and nurse practitioners (ranked 3rd).
These rankings highlight the diverse and lucrative opportunities within the nursing profession. Registered nurses (RNs) are the backbone of healthcare, providing essential care and coordination in various settings. Nurse anesthetists, who administer anesthesia and monitor patients during surgical procedures, are highly specialized and command competitive salaries. Nurse practitioners (NPs) have advanced training that allows them to diagnose and treat medical conditions, often serving as primary care providers. The high ranking of NPs reflects the growing recognition of their critical role in expanding access to healthcare.
7. Mary Eliza Mahoney’s Legacy
Mary Eliza Mahoney, the first African American registered nurse in the United States, broke significant barriers in the field of nursing. Born in 1845 in Boston, Mahoney worked at the New England Hospital for Women and Children for 15 years before enrolling in its nursing program. She graduated in 1879, becoming one of only three graduates out of a class of 42.
Mahoney’s accomplishments extend beyond her personal achievements. She co-founded the National Association of Colored Graduate Nurses (NACGN) in 1908, advocating for the inclusion and recognition of African American nurses. The NACGN played a crucial role in supporting black nurses and promoting racial equality in the profession. Mahoney’s legacy is a testament to her resilience, dedication, and pioneering spirit, which continue to inspire nurses today.
8. The U.S. Nursing Workforce
As of 2020, there were approximately three million nurses in the United States, comparable to the population of Jamaica. This vast workforce is essential to the functioning of the healthcare system. Nurses work in a variety of settings, including hospitals, clinics, long-term care facilities, schools, and community health centers.
Globally, there are over 28 million nurses, accounting for 59% of healthcare professionals worldwide. This significant presence underscores the critical role nurses play in delivering healthcare services. However, the global nursing workforce faces challenges such as shortages, particularly in low- and middle-income countries. Efforts to address these shortages include increasing educational opportunities, improving working conditions, and supporting international collaboration.
9. Projected Growth in Nursing
The nursing field is not only large but also poised for continued growth. According to the U.S. Bureau of Labor Statistics, the employment of registered nurses is projected to increase by 7% from 2019 to 2029. This growth is driven by several factors, including an aging population, increased prevalence of chronic diseases, and expanded access to healthcare services.
The projected growth in nursing offers substantial opportunities for those entering the profession. It also underscores the importance of supporting nursing education and training programs to meet the demand for skilled nurses. Healthcare organizations and policymakers must invest in initiatives that attract and retain nurses, ensuring a robust workforce to provide high-quality care.
10. Diverse Work Environments
While hospitals remain the largest employer of nurses, the nursing profession offers diverse work environments. According to data from the U.S. Bureau of Labor Statistics, the distribution of nurses across various settings is as follows:
Hospitals: 60%
Ambulatory healthcare services: 18%
Nursing and residential care facilities: 7%
Government: 5%
Educational services: 3%
This diversity allows nurses to work in a range of settings, each with its unique challenges and opportunities. Ambulatory healthcare services include outpatient clinics, surgical centers, and primary care practices, where nurses play a vital role in patient care and health promotion. Nursing and residential care facilities provide long-term care for individuals with chronic illnesses or disabilities, emphasizing the importance of compassionate, ongoing support. Government and educational services offer roles in public health, policy, research, and academia, contributing to the advancement of the profession and the improvement of public health.
11. National Nurses Week
National Nurses Week, celebrated annually from May 6 to May 12, honors the challenging work and dedication of nurses. Established over 40 years ago, this week-long celebration culminates on May 12, the birthday of Florence Nightingale. The week recognizes the significant contributions of nurses to healthcare and society.
National Nurses Week includes various events and activities to celebrate and appreciate nurses. These may include educational seminars, award ceremonies, community outreach programs, and public awareness campaigns. The celebration provides an opportunity to highlight the vital role of nurses, advocate for their needs, and inspire the next generation of nursing professionals.
12. Staffing Agencies and Nursing Employment
Nurse staffing agencies play a crucial role in addressing the fluctuating demand for nursing services. Many nurses find employment through staffing agencies, which help them secure jobs and new opportunities. These agencies match nurses with healthcare facilities that need additional staff, ensuring that patient care remains uninterrupted.
For staffing agencies, keeping pace with the rising demand for nurses is crucial. Solutions like invoice factoring can provide the necessary funding to grow and support their operations effectively. Invoice factoring allows agencies to sell their accounts receivable at a discount in exchange for immediate cash, helping them manage cash flow and invest in recruiting and retaining qualified nurses.
Conclusion
These facts not only highlight the rich history and essential role of nursing but also underscore the profession’s ongoing evolution and the increasing opportunities within the field. Whether you’re a nurse or involved in nursing services, staying informed about these developments is key to advancing in this vital industry. The nursing profession continues to grow and adapt, driven by a commitment to providing high-quality care and improving patient outcomes.
For those involved in nurse staffing, understanding the dynamics of the nursing workforce and exploring financial solutions like invoice factoring can help meet the rising demand and ensure continued success. By recognizing the historical significance, current trends, and future prospects of nursing, we can better support and celebrate this indispensable profession.
For medical students and nurses of all categories, navigating assignments, homework, case studies, research, online classes, and challenging medical units can be daunting. Seeking professional guidance and assistance can make a significant difference in your academic and professional journey. For expert help with these challenges, consider reaching out to Expert Academic Assignment Help at expertassignment46@gmail.com Our professional support can help you excel in your studies and career.
How to Write a Compelling Blog Post

Crafting captivating headlines is an art that can make or break a blog post. Your headline serves as the gateway to your content, enticing readers indulging deeper into your article. In this comprehensive guide, we’ll involve into the ways and methods of crafting irresistible headlines that not only grab attention but also keep readers engaged from start to finish.
Craft a Great Headline That Readers Can’t Resist

The headline sets the stage for your entire post, acting as a beacon to guide readers towards the valuable insights and information you have to offer. To create a headline that truly resonates with your audience, consider the following strategies:
1.Promise a Solution: Your headline should address a specific problem or need that your target audience has. By promising a solution or benefit, you immediately capture their interest and encourage them to keep reading.
2.Know Your Audience: Conduct thorough research to understand the pain points and interests of your target audience. Tailor your headline to speak directly to their needs and desires, ensuring maximum relevance and engagement.
3.Utilize Proven Templates: Tried-and-tested headline formulas like “How to” and list posts are effective for grabbing attention and driving clicks. Experiment with different templates to see what resonates best with your audience.
4.Engage the Senses: Use sensory words and vivid language to evoke emotions and create a tangible experience for your readers. Engaging multiple senses can make your headline more compelling and memorable.
5.Avoid Over-Promising: While it’s important to make your headline enticing, avoid exaggeration or over-promising. Be truthful and transparent in your messaging to maintain trust and credibility with your audience.
Write an Introduction That Grabs and Seduces

Once you’ve crafted a compelling headline, the introduction serves as the gateway to your content. It should build upon the promise made in the headline and draw readers in with captivating storytelling, thought-provoking questions, or intriguing facts. Consider the following tips for writing an irresistible introduction:
1.Hook Your Readers: Capture readers’ attention from the very first sentence with a compelling hook that intrigues and entices.
2.Set the Tone: Establish the tone and style of your post in the introduction, giving readers a glimpse of what to expect.
3.Preview the Content: Provide a brief overview of what readers can expect to learn or gain from reading your post. This sets clear expectations and encourages readers to continue reading.
Deliver Advice That’s Easy to Consume and Impossible to Ignore
The main body of your post is where you deliver on the promise made in the headline and introduction. Here’s how to ensure your content is both valuable and engaging:
1.Provide Valuable Insights: Offer practical advice, valuable insights, or informative content that fulfills the promise made in your headline.
2. Organize Your Content: Break down complex ideas into digestible chunks and use subheadings to guide readers through your content. This makes it easier for readers to consume and retain information.
3.Incorporate Visuals: Use visuals such as images, infographics, or videos to enhance comprehension and engagement. Visual elements can break up text-heavy content and make your post more visually appealing.
4.Keep it Engaging: Maintain a conversational tone and engage readers with relatable examples, or case studies. Encourage interaction by asking questions or prompting readers to share their experiences.
Close with a Motivational B
The conclusion of your post is your final opportunity to leave a lasting impression on your readers. Here’s how to end your post on a high note:
Summarize Key Points: Recap the main points or takeaways from your post to reinforce the message you’ve conveyed
Provide a Call to Action: Encourage readers to take the next step, whether it’s sharing the post, leaving a comment, or implementing the advice you’ve provided. A clear call to action motivates readers to engage with your content beyond the initial reading.
3.Leave a Memorable Impression: End your post with a memorable closing statement or thought-provoking question that leaves readers thinking long after they’ve finished reading.
Polish Your Post So It’s Smoother Than a Slip ‘n Slide
Before you hit publish, it’s essential to thoroughly edit and polish your post to ensure it’s error-free and polished to perfection. Consider the following tips for polishing your post:
1.Edit for Clarity and Coherence: Review your content for clarity, coherence, and logical flow. Ensure that your ideas are presented in a clear and organized manner.
2.Check for Grammar and Spelling Errors: Proofread your post carefully to catch any grammatical errors, spelling mistakes, or typos. Use grammar-checking tools or enlist the help of a peer to ensure your writing is error-free.
3.Format for Readability: Pay attention to formatting elements such as headings, paragraphs, and bullet points to enhance readability. Break up long blocks of text and use formatting techniques to make your post visually appealing.
4.Seek Feedback: Consider seeking feedback from peers or beta readers to get an outside perspective on your post. Fresh eyes can help identify areas for improvement and ensure your content resonates with your target audience.
By following these steps, you can create blog posts that captivate readers, provide valuable insights, and leave a lasting impression. Crafting compelling headlines is just the first step in creating engaging content that resonates with your audience, but by mastering the art of headline writing, you can set your posts up for success from the very beginning.
In conclusion, mastering the art of blog writing is crucial for creating engaging content that resonates with your audience. If you’re looking to enhance your blogging skills and ensure your posts are set up for success, consider seeking assistance from Expert Academic Assignment. Get in touch via email at expertassignment46@gmail.com to discover how our expertise can elevate your writing game. Remember, it’s okay to seek help when you need it, especially when it comes to crafting compelling content.
Digestive System

The digestive system is a marvel of biological engineering, orchestrating the journey of food through the body, from the moment it enters the mouth to its exit through the anus. This complex process involves a network of organs, each playing a crucial role in breaking down food, absorbing nutrients, and eliminating waste. In this detailed exploration, we delve into the anatomy, functions, common conditions, care practices, and the importance of seeking medical attention for digestive system issues.
Anatomy of the Digestive System
Gastrointestinal (GI) Tract:
1.Mouth:
Initiating Digestion: Salivary glands activate as the sight and scent of food trigger the digestive process.
Chewing and Mixing: Food is chewed into digestible pieces, mixed with saliva to facilitate breakdown.
Swallowing: The tongue propels the food into the throat and esophagus.
2. Esophagus:
Transportation: A muscular tube conducting food to the stomach through peristalsis.
Sphincter Function: The lower esophageal sphincter relaxes to allow food entry and contracts to prevent stomach content reflux.
3.Stomach:
Container and Mixer: A hollow organ holding and mixing food with stomach enzymes for further breakdown.
Acid Secretion: Cells in the stomach lining secrete powerful acids and enzymes crucial for digestion.
Release to Small Intestine: Processed stomach contents move to the small intestine for further digestion.
4.Small Intestine:
Segments and Functions: Comprising the duodenum, jejunum, and ileum, each segment has distinct roles in digestion and nutrient absorption.
Enzymatic Breakdown: Pancreatic enzymes and bile from the liver aid in breaking down food.
Nutrient Absorption: The jejunum and ileum absorb nutrients into the bloodstream.
Consistency Changes: Contents transition from semi-solid to liquid as water, bile, enzymes, and mucus contribute to the process.
Biliary System:
a. pancreas:
Enzyme Secretion: Releases digestive enzymes into the duodenum to break down proteins, fats, and carbohydrates.
Insulin Production: The pancreas produces insulin, a key hormone for sugar metabolism.
b. Liver:
Nutrient Processing: Processes nutrients absorbed by the small intestine.
Bile Production: Secretes bile into the small intestine, aiding in fat digestion and vitamin absorption.
Detoxification: Acts as the body’s chemical “factory,” detoxifying harmful substances.
c. Gallbladder:
Bile Storage: Stores and concentrates bile from the liver.
Release into Duodenum: Releases bile into the duodenum to assist in fat absorption.
Large Intestine (Colon):
Colon:
Waste Processing: Responsible for transforming waste into a convenient form for bowel movements.
Peristalsis: Propels stool through the colon, removing water and transitioning it from a liquid to a solid state.
Storage and Elimination: Stool is stored in the sigmoid colon until mass movements propel it into the rectum for elimination.
Rectum:
Chamber Function: A straight chamber connecting the colon to the anus.
Signaling and Holding: Signals the brain about stool presence and holds stool until evacuation.
Anus:
Final Elimination: The last part of the digestive tract, consisting of pelvic floor muscles and sphincters.
Sphincter Control: Surrounding sphincter muscles control stool release, preventing involuntary bowel movements.
Conditions and Disorders
Digestive system health can be affected by a spectrum of conditions, ranging from temporary issues to chronic diseases:
Temporary Conditions:
Constipation:
Frequency and Characteristics: Reduced bowel movements with dry and hard stool.
Difficulty and Pain: Straining during bowel movements, leading to discomfort.
2.Diarrhea:
Loose and Watery Stool: Abnormal stool consistency often caused by various factors.
Potential Causes: Bacterial infections, dietary issues, or unknown triggers.
3.Heartburn:
Misleading Name: Despite the name, heartburn is a digestive issue.
Acidic Backflow: Occurs when stomach acids move up the esophagus, causing discomfort in the chest.
4.Hemorrhoids:
Swollen Veins: Enlarged veins inside and outside the anus and rectum.
Symptoms: Pain, discomfort, and rectal bleeding.
5.Stomach Flu (Gastroenteritis):
Viral Infection: Infection of the stomach and upper part of the small intestine.
Duration: Typically lasts less than a week.
6.Ulcers:
Sore Development: Sores on the lining of the esophagus, stomach, or small intestine.
Causes: Helicobacter pylori infection and prolonged use of anti-inflammatory drugs.
7.Gallstones:
Solid Material Formation: Small pieces formed from digestive fluid in the gallbladder.
Chronic Diseases:
GERD (Chronic Acid Reflux):
Frequent Acid Backflow: Acid-containing contents in the stomach frequently leak into the esophagus.
Symptoms: Persistent heartburn and regurgitation.
2,Irritable Bowel Syndrome (IBS):
Colon Muscle Dysfunction: Irregular contractions leading to excessive gas, abdominal pain, and cramps.
Chronic Nature: A long-term condition affecting bowel function.
3.Lactose Intolerance:
Inability to Digest Lactose: Results in digestive discomfort after consuming milk and dairy products.
Common Symptoms: Bloating, gas, and diarrhea.
4.Diverticulosis and Diverticulitis:
Colon Pockets Formation: Diverticula (pockets) in the wall of the colon.
Complications: Inflammation (diverticulitis) can occur, causing pain and infection.
5.Gastrointestinal (GI) Cancers:
Tissue and Organ Affliction: Cancers affecting the digestive system, including esophageal, gastric, colorectal, pancreatic, and liver cancers.
6.Crohn’s Disease:
Inflammatory Bowel Disease (IBD): A lifelong condition causing inflammation in the digestive tract.
7.Celiac Disease:
Autoimmune Disorder: Gluten consumption damages the small intestine.
Trigger: Found in wheat, barley, and rye.
Care Practices for Digestive Health
Maintaining a healthy digestive system involves adopting proactive lifestyle and dietary habits:
1.Hydration:
Importance of Water: Drinking water facilitates smooth food flow, preventing dehydration-related constipation.
Dehydration Consequences: Insufficient water intake can lead to dry and hard stool.
2.Fiber-Rich Diet:
Benefits of Fiber: Supports digestion and regular bowel movements.
Soluble and Insoluble Fiber: Both types contribute to digestive health.
3.Balanced Nutrition:
Fruits and Vegetables: Multiple servings daily for essential vitamins and minerals.
Whole Grains: Choosing whole grains over processed grains.
Limiting Processed Foods: Reducing intake of processed and sugary foods.
4.Probiotics:
Role of Probiotics: Supporting a healthy gut microbiome.
Post-Antibiotic Use: Especially beneficial after antibiotic treatments.
5.Mindful Eating:
Chewing and Digestion: Thorough chewing aids in proper digestion.
Eating Pace: Slower eating allows the body to signal fullness.
6.Physical Activity:
Exercise and Digestion: Physical activity and gravity aid in moving food through the digestive system.
Post-Meal Walks: Taking a walk after meals can enhance digestion.
7.Avoiding Harmful Habits:
Alcohol and Smoking: Limiting alcohol intake to prevent acid-related issues.
Smoking Cessation: Quitting smoking improves digestive symptoms.
8.Stress Management:
Stress and Digestive Issues: Association between stress and conditions like constipation, diarrhea, and IBS.
Stress Reduction Techniques: Incorporating stress-relief practices into daily life.
Seeking Medical Attention
While occasional digestive issues are common, persistent symptoms warrant attention:
When to Contact a Healthcare Provider:
Frequent Symptoms: Constipation, diarrhea, vomiting, stomach pain, excessive gas, or heartburn.
Potential Underlying Issues: Frequent occurrences may indicate a more serious digestive system problem.
2.Importance of Medical Evaluation:
Diagnostic Assessment: Identifying the cause of persistent symptoms.
Early Intervention: Timely treatment prevents potential complications.
3.Collaborative Approach:
Healthcare Professional Guidance: Seeking advice on managing and preventing digestive issues.
Individualized Care: Tailoring interventions based on the individual’s health status and conditions.
Conclusion
In conclusion, understanding the details of the digestive system provides a foundation for promoting digestive health. The collaboration of organs in the GI tract and the biliary system highlights the complexity of the digestive process. Awareness of common conditions, care practices, and the significance of seeking medical attention empowers individuals to prioritize their digestive well-being. Adopting a holistic approach that combines a healthy lifestyle, balanced nutrition, and regular medical check-ups ensures a resilient and well-functioning digestive system, contributing to overall health and vitality.
For Health Sciences Assignment Help;
Email us on;
williamsliason@outlook.com
Digestive System

The digestive system is a marvel of biological engineering, orchestrating the journey of food through the body, from the moment it enters the mouth to its exit through the anus. This complex process involves a network of organs, each playing a crucial role in breaking down food, absorbing nutrients, and eliminating waste. In this detailed exploration, we delve into the anatomy, functions, common conditions, care practices, and the importance of seeking medical attention for digestive system issues.
Anatomy of the Digestive System

Gastrointestinal (GI) Tract:
1.Mouth:
Initiating Digestion: Salivary glands activate as the sight and scent of food trigger the digestive process.
Chewing and Mixing: Food is chewed into digestible pieces, mixed with saliva to facilitate breakdown.
Swallowing: The tongue propels the food into the throat and esophagus.
2. Esophagus:
Transportation: A muscular tube conducting food to the stomach through peristalsis.
Sphincter Function: The lower esophageal sphincter relaxes to allow food entry and contracts to prevent stomach content reflux.
3.Stomach:
Container and Mixer: A hollow organ holding and mixing food with stomach enzymes for further breakdown.
Acid Secretion: Cells in the stomach lining secrete powerful acids and enzymes crucial for digestion.
Release to Small Intestine: Processed stomach contents move to the small intestine for further digestion.
4.Small Intestine:
Segments and Functions: Comprising the duodenum, jejunum, and ileum, each segment has distinct roles in digestion and nutrient absorption.
Enzymatic Breakdown: Pancreatic enzymes and bile from the liver aid in breaking down food.
Nutrient Absorption: The jejunum and ileum absorb nutrients into the bloodstream.
Consistency Changes: Contents transition from semi-solid to liquid as water, bile, enzymes, and mucus contribute to the process.
Biliary System

a. pancreas:
Enzyme Secretion: Releases digestive enzymes into the duodenum to break down proteins, fats, and carbohydrates.
Insulin Production: The pancreas produces insulin, a key hormone for sugar metabolism.
b. Liver:
Nutrient Processing: Processes nutrients absorbed by the small intestine.
Bile Production: Secretes bile into the small intestine, aiding in fat digestion and vitamin absorption.
Detoxification: Acts as the body’s chemical “factory,” detoxifying harmful substances.
c. Gallbladder:
Bile Storage: Stores and concentrates bile from the liver.
Release into Duodenum: Releases bile into the duodenum to assist in fat absorption.
Large Intestine (Colon):
Colon:
Waste Processing: Responsible for transforming waste into a convenient form for bowel movements.
Peristalsis: Propels stool through the colon, removing water and transitioning it from a liquid to a solid state.
Storage and Elimination: Stool is stored in the sigmoid colon until mass movements propel it into the rectum for elimination.
Rectum:
Chamber Function: A straight chamber connecting the colon to the anus.
Signaling and Holding: Signals the brain about stool presence and holds stool until evacuation.
Anus:
Final Elimination: The last part of the digestive tract, consisting of pelvic floor muscles and sphincters.
Sphincter Control: Surrounding sphincter muscles control stool release, preventing involuntary bowel movements.
Conditions and Disorders
Digestive system health can be affected by a spectrum of conditions, ranging from temporary issues to chronic diseases:
Temporary Conditions:
Constipation:
Frequency and Characteristics: Reduced bowel movements with dry and hard stool.
Difficulty and Pain: Straining during bowel movements, leading to discomfort.
2.Diarrhea:
Loose and Watery Stool: Abnormal stool consistency often caused by various factors.
Potential Causes: Bacterial infections, dietary issues, or unknown triggers.
3.Heartburn:
Misleading Name: Despite the name, heartburn is a digestive issue.
Acidic Backflow: Occurs when stomach acids move up the esophagus, causing discomfort in the chest.
4.Hemorrhoids:
Swollen Veins: Enlarged veins inside and outside the anus and rectum.
Symptoms: Pain, discomfort, and rectal bleeding.
5.Stomach Flu (Gastroenteritis):
Viral Infection: Infection of the stomach and upper part of the small intestine.
Duration: Typically lasts less than a week.
6.Ulcers:
Sore Development: Sores on the lining of the esophagus, stomach, or small intestine.
Causes: Helicobacter pylori infection and prolonged use of anti-inflammatory drugs.
7.Gallstones:
Solid Material Formation: Small pieces formed from digestive fluid in the gallbladder.
Chronic Diseases:
GERD (Chronic Acid Reflux):
Frequent Acid Backflow: Acid-containing contents in the stomach frequently leak into the esophagus.
Symptoms: Persistent heartburn and regurgitation.
2,Irritable Bowel Syndrome (IBS):
Colon Muscle Dysfunction: Irregular contractions leading to excessive gas, abdominal pain, and cramps.
Chronic Nature: A long-term condition affecting bowel function.
3.Lactose Intolerance:
Inability to Digest Lactose: Results in digestive discomfort after consuming milk and dairy products.
Common Symptoms: Bloating, gas, and diarrhea.
4.Diverticulosis and Diverticulitis:
Colon Pockets Formation: Diverticula (pockets) in the wall of the colon.
Complications: Inflammation (diverticulitis) can occur, causing pain and infection.
5.Gastrointestinal (GI) Cancers:
Tissue and Organ Affliction: Cancers affecting the digestive system, including esophageal, gastric, colorectal, pancreatic, and liver cancers.
6.Crohn’s Disease:
Inflammatory Bowel Disease (IBD): A lifelong condition causing inflammation in the digestive tract.
7.Celiac Disease:
Autoimmune Disorder: Gluten consumption damages the small intestine.
Trigger: Found in wheat, barley, and rye.
Care Practices for Digestive Health

Maintaining a healthy digestive system involves adopting proactive lifestyle and dietary habits:
1.Hydration:
Importance of Water: Drinking water facilitates smooth food flow, preventing dehydration-related constipation.
Dehydration Consequences: Insufficient water intake can lead to dry and hard stool.
2.Fiber-Rich Diet:
Benefits of Fiber: Supports digestion and regular bowel movements.
Soluble and Insoluble Fiber: Both types contribute to digestive health.
3.Balanced Nutrition:
Fruits and Vegetables: Multiple servings daily for essential vitamins and minerals.
Whole Grains: Choosing whole grains over processed grains.
Limiting Processed Foods: Reducing intake of processed and sugary foods.
4.Probiotics:
Role of Probiotics: Supporting a healthy gut microbiome.
Post-Antibiotic Use: Especially beneficial after antibiotic treatments.
5.Mindful Eating:
Chewing and Digestion: Thorough chewing aids in proper digestion.
Eating Pace: Slower eating allows the body to signal fullness.
6.Physical Activity:
Exercise and Digestion: Physical activity and gravity aid in moving food through the digestive system.
Post-Meal Walks: Taking a walk after meals can enhance digestion.
7.Avoiding Harmful Habits:
Alcohol and Smoking: Limiting alcohol intake to prevent acid-related issues.
Smoking Cessation: Quitting smoking improves digestive symptoms.
8.Stress Management:
Stress and Digestive Issues: Association between stress and conditions like constipation, diarrhea, and IBS.
Stress Reduction Techniques: Incorporating stress-relief practices into daily life.
Seeking Medical Attention
While occasional digestive issues are common, persistent symptoms warrant attention:
When to Contact a Healthcare Provider:
Frequent Symptoms: Constipation, diarrhea, vomiting, stomach pain, excessive gas, or heartburn.
Potential Underlying Issues: Frequent occurrences may indicate a more serious digestive system problem.
2.Importance of Medical Evaluation:
Diagnostic Assessment: Identifying the cause of persistent symptoms.
Early Intervention: Timely treatment prevents potential complications.
3.Collaborative Approach:
Healthcare Professional Guidance: Seeking advice on managing and preventing digestive issues.
Individualized Care: Tailoring interventions based on the individual’s health status and conditions.
Conclusion
In conclusion, understanding the details of the digestive system provides a foundation for promoting digestive health. The collaboration of organs in the GI tract and the biliary system highlights the complexity of the digestive process. Awareness of common conditions, care practices, and the significance of seeking medical attention empowers individuals to prioritize their digestive well-being. Adopting a holistic approach that combines a healthy lifestyle, balanced nutrition, and regular medical check-ups ensures a resilient and well-functioning digestive system, contributing to overall health and vitality.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for professional assistance.
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science

The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work

Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader

A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.

Thank you @kitteena and everyone who got me to 5 reblogs!
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com
What Makes a PhD Dissertation Different from a Masters Thesis?

Introduction
In the realm of academia, pursuing advanced degrees such as a Master’s or a PhD involves rigorous research and scholarly endeavors. Central to this academic journey are the culminating projects — the Master’s thesis and the PhD dissertation. While often used interchangeably, these two academic works possess distinct characteristics that set them apart. In this comprehensive discussion, we will major into the differences between a PhD dissertation and a Master’s thesis, exploring various aspects including the depth of research, original contribution to knowledge, duration and intensity of study, evaluation and defense process, as well as career implications and academic prestige.
Depth of Research

One of the fundamental disparities between a PhD dissertation and a Master’s thesis lies in the depth of research. A Master’s thesis typically explores a specific topic within a field of study, offering a comprehensive analysis but within a more confined framework. In contrast, a PhD dissertation delves into original research, contributing novel insights or advancing existing knowledge within the chosen discipline. The depth of investigation required for a dissertation is considerably greater, often involving extensive data collection, analysis, and interpretation.
Original Contribution to Knowledge

Building upon the notion of originality, a PhD dissertation is expected to make a significant contribution to the body of knowledge within the respective field. It must demonstrate a unique perspective, innovative methodology, or novel findings that add value to the academic discourse. On the other hand, while a Master’s thesis also involves original research, its contribution may be more incremental or focused on synthesizing existing literature rather than forging new paths of inquiry.
Duration and Intensity of Study

Another factor that distinguishes a PhD dissertation from a Master’s thesis is the duration and intensity of study involved. Pursuing a PhD typically entails a more prolonged and immersive engagement with the research topic, spanning several years of dedicated study and inquiry. The process of conducting original research, analyzing data, and drafting a dissertation demands a substantial commitment of time and effort. In contrast, a Master’s thesis can often be completed within a shorter timeframe, typically ranging from one to two years, depending on the program’s requirements.
Evaluation and Defense Process
The evaluation and defense process also differ between a PhD dissertation and a Master’s thesis. For a PhD dissertation, the candidate must present their research findings to a committee of faculty members or experts in the field. This oral defense involves a rigorous examination of the dissertation’s methodology, results, and conclusions, as well as the candidate’s ability to articulate and defend their research. In contrast, while some Master’s programs may require a thesis defense, the level of scrutiny and formality is often less intense compared to a PhD dissertation defense.
Career Implications and Academic Prestige

Furthermore, the completion of a PhD dissertation carries significant career implications and academic prestige. Attaining a PhD is often regarded as the highest level of academic achievement, opening doors to advanced research positions, teaching opportunities, and leadership roles within academia and industry. A PhD dissertation serves as a hallmark of expertise and scholarly rigor, signaling to the academic community and potential employers the candidate’s ability to conduct independent research at a high level. On the other hand, while a Master’s thesis is a commendable accomplishment in its own right, it may not carry the same weight in terms of career advancement or academic recognition as a PhD dissertation.
Conclusion
In conclusion, the comparison between a PhD dissertation and a Master’s thesis reveals the intricate differences that exist between these two academic endeavors. While both represent significant milestones in academic scholarship, they embody distinct attributes that reflect the depth of research, originality of contribution, and level of academic achievement. Whether seeking thesis vs. dissertation writing help or PhD dissertation assistance, students embarking on these scholarly endeavors can benefit from the guidance and support offered by dissertation writing services. With expert assistance, aspiring scholars can navigate the complexities of research, writing, and presentation, ensuring their academic work meets the highest standards of excellence and scholarly rigor
Understanding the differences between a PhD dissertation and a Master’s thesis is crucial for students embarking on academic research. Expert Academic Assignment Help offers personalized support at every stage of the process, ensuring academic excellence. Reach out at expertassignment46@gmail.com to benefit from expertise and guidance in navigating the complexities of research, writing, and presentation.
Atherosclerosis

Introduction
Atherosclerosis is a chronic and progressive condition characterized by the accumulation of plaque within the walls of arteries, leading to their hardening and narrowing. Despite being often asymptomatic in its early stages, atherosclerosis poses significant risks to cardiovascular health and can result in severe complications such as heart attacks, strokes, and peripheral artery disease (PAD). Therefore, comprehensive knowledge of its symptoms, causes, prevention strategies, diagnosis methods, and treatment options is imperative for effectively managing its impact on individuals’ well-being.
Symptoms of Atherosclerosis

Atherosclerosis typically advances silently, with symptoms only becoming apparent as arteries become significantly obstructed or when a cardiovascular event occurs. The manifestation of symptoms varies depending on the affected arteries, each presenting distinct clinical presentations:
Coronary Arteries: The narrowing of coronary arteries due to atherosclerosis can lead to symptoms such as arrhythmia (irregular heartbeat), angina (chest pain or pressure), and shortness of breath, especially during physical exertion.
Cerebral Arteries: Atherosclerosis affecting cerebral arteries may manifest as numbness or weakness in the limbs, difficulty speaking or understanding speech, drooping facial muscles, paralysis, severe headache, or vision problems, indicating a heightened risk of stroke.
3. Peripheral Arteries: Individuals with atherosclerosis in peripheral arteries may experience symptoms such as leg pain when walking (intermittent claudication), numbness, cold extremities, aching or burning sensations in the feet, and slow-healing wounds or infections, reflecting compromised blood flow to the extremities
4. Renal Arteries: Atherosclerosis affecting renal arteries can result in elevated blood pressure (hypertension) and eventual kidney failure, highlighting the systemic impact of arterial narrowing on vital organ function.
Causes and Stages of Atherosclerosis

The development and progression of atherosclerosis involve a series of intricate biological processes initiated by damage to the endothelium, the delicate inner lining of arteries. As plaque composed of cholesterol, fat, calcium, and inflammatory substances accumulates within arterial walls, the disease progresses through distinct stages:
Damage to the Endothelium: The initial stage of atherosclerosis is characterized by injury to the endothelial cells lining the arteries, often attributed to risk factors such as high cholesterol, hypertension, inflammation, obesity, diabetes, and smoking.
2. Formation of Fatty Streaks: Following endothelial damage, the infiltration of low-density lipoprotein (LDL) cholesterol into the arterial wall triggers an inflammatory response, leading to the formation of fatty streaks — the earliest visible signs of atherosclerosis.
3 . Development of Fibrous Plaques: Over time, the accumulation of cholesterol-laden foam cells and the proliferation of smooth muscle cells contribute to the formation of fibrous plaques, which protrude into the arterial lumen and impede blood flow.
4 . Formation of Complicated Lesions: Advanced atherosclerosis is characterized by the formation of complicated lesions, where unstable plaques prone to rupture expose thrombogenic components, leading to the formation of blood clots and subsequent cardiovascular events such as myocardial infarction or ischemic stroke.
Risk Factors for Atherosclerosis
Numerous modifiable and non-modifiable risk factors influence the development and progression of atherosclerosis, underscoring the multifactorial nature of the disease. These risk factors include:
High Cholesterol: Elevated levels of LDL cholesterol, commonly referred to as “bad” cholesterol, promote the deposition of cholesterol within arterial walls, contributing to plaque formation and atherosclerosis progression.
2. High Blood Pressure: Hypertension exerts mechanical stress on arterial walls, accelerating endothelial damage and promoting atherosclerosis development
3. Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis or systemic lupus erythematosus, exacerbate endothelial dysfunction and foster plaque formation within arteries.
4. Obesity: Excess adiposity predisposes individuals to metabolic abnormalities, including dyslipidemia and insulin resistance, which fuel atherosclerosis progression.
5. Diabetes: Both type 1 and type 2 diabetes mellitus increase the risk of atherosclerosis by inducing endothelial dysfunction, promoting inflammation, and accelerating the formation of advanced glycation end-products (AGEs) implicated in vascular
6. Smoking: Tobacco smoke contains toxic compounds that promote endothelial injury, oxidative stress, and inflammation, exacerbating the progression of atherosclerosis and increasing the risk of cardiovascular events.
7.Sedentary Lifestyle: Physical inactivity contributes to metabolic derangements, including obesity, dyslipidemia, and insulin resistance, fostering atherosclerosis development and cardiovascular risk.
8. Family History of Heart Disease: Genetic predisposition plays a significant role in atherosclerosis susceptibility, with familial clustering of cardiovascular risk factors amplifying the likelihood of disease manifestation.
9. Poor Diet: Diets rich in saturated fats, trans fats, refined carbohydrates, and excess sodium promote dyslipidemia, hypertension, and endothelial dysfunction, fueling atherosclerosis progression.
9 .Stress: Chronic stress triggers sympathetic nervous system activation and cortisol release, contributing to hypertension, inflammation, and atherosclerosis development
10. Sleep Apnea: Obstructive sleep apnea, characterized by recurrent episodes of upper airway obstruction during sleep, disrupts normal cardiovascular function and exacerbates atherosclerosis progression.
Identifying and addressing these risk factors through targeted interventions and lifestyle modifications are essential for mitigating the burden of atherosclerosis and reducing the risk of cardiovascular events.
Diagnosis and Treatment of Atherosclerosis

Accurate diagnosis and effective management of atherosclerosis require a multidisciplinary approach involving clinical evaluation, imaging studies, and laboratory testing. Diagnostic modalities utilized in the assessment of atherosclerosis include:
Physical Examination: Healthcare providers perform a comprehensive physical examination, assessing vital signs, auscultating for abnormal heart sounds or bruits, and palpating for peripheral pulses to evaluate cardiovascular health.
Imaging Tests: Various imaging modalities are employed to visualize arterial anatomy, assess plaque burden, and identify areas of stenosis or occlusion. These includes;
Angiography: Intravascular contrast dye is utilized to visualize arterial lumens and detect areas of stenosis or occlusion via X-ray imaging.
Ultrasound: Non-invasive ultrasound techniques, such as carotid ultrasound or abdominal ultrasound, enable the assessment of arterial wall thickness, plaque morphology, and blood flow characteristics.
Computed Tomography (CT) Angiography: CT angiography provides detailed anatomical imaging of arterial structures, facilitating the identification of atherosclerotic lesions and assessing their severity.
Magnetic Resonance Angiography (MRA): MRA employs magnetic resonance imaging (MRI) techniques to generate high-resolution images of blood vessels, aiding in the evaluation of arterial stenosis, plaque composition, and hemodynamic parameters.
3. Laboratory Evaluations: Blood tests are conducted to assess lipid profiles, inflammatory markers, and other biochemical parameters associated with cardiovascular risk. These include
Lipid Profile: Measurement of serum lipid levels, including total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides, provides insight into atherosclerosis risk and treatment efficacy.
Inflammatory Markers: Assessment of inflammatory biomarkers, such as C-reactive protein (CRP) or interleukin-6 (IL-6), aids in risk stratification and monitoring disease activity in individuals with atherosclerosis.
Blood Glucose: Screening for abnormal glucose metabolism, including fasting blood glucose and hemoglobin A1c (HbA1c) levels, helps identify individuals at risk of diabetes-associated atherosclerosis complications
4. Functional Tests: Functional assessments, such as stress testing or ankle-brachial index (ABI) measurement, are performed to evaluate cardiovascular function and assess the impact of atherosclerosis on tissue perfusion.
Once diagnosed, the management of atherosclerosis encompasses various approach targeting risk factor modification, pharmacological intervention, and, when indicated, invasive procedures to alleviate arterial obstruction and prevent cardiovascular events.
Treatment strategies for atherosclerosis include:
Lifestyle Modifications: Lifestyle interventions form the cornerstone of atherosclerosis management, emphasizing dietary modifications, regular physical activity, smoking cessation, stress reduction, and weight management to optimize cardiovascular health and mitigate disease progression.
Medication Management: Pharmacological therapy plays a pivotal role in atherosclerosis treatment, targeting modifiable risk factors such as dyslipidemia, hypertension, and inflammation. Commonly prescribed medications include
Statins: HMG-CoA reductase inhibitors, such as atorvastatin or simvastatin, reduce LDL cholesterol levels and stabilize atherosclerotic plaques, lowering the risk of cardiovascular events.
Antihypertensive Agents: Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and calcium channel blockers are utilized to control blood pressure and mitigate endothelial dysfunction in individuals with hypertension-associated atherosclerosis.
Antiplatelet Therapy: Aspirin and other antiplatelet agents, such as clopidogrel or ticagrelor, inhibit platelet aggregation and reduce the risk of thrombotic events in individuals with established atherosclerosis or high cardiovascular risk.
Antidiabetic Medications: Oral hypoglycemic agents, insulin, or glucagon-like peptide-1 (GLP-1) receptor agonists are prescribed to achieve glycemic control and minimize the risk of diabetes-related atherosclerosis complications.
3. Invasive Procedures: In cases of severe arterial stenosis or symptomatic atherosclerotic disease refractory to medical therapy, invasive interventions may be warranted to restore arterial patency and alleviate ischemic symptoms. These include:
Percutaneous Coronary Intervention (PCI): Angioplasty with or without stent placement is performed to widen narrowed coronary arteries and improve myocardial perfusion in individuals with coronary artery disease (CAD).
Coronary Artery Bypass Grafting (CABG): Surgical revascularization using autologous or synthetic conduits bypasses obstructed coronary vessels, restoring blood flow to ischemic myocardial territories in patients with multivessel CAD or left main coronary artery disease.
Carotid Endarterectomy: Surgical removal of atherosclerotic plaque from carotid arteries reduces the risk of stroke in individuals with significant carotid stenosis and a history of transient ischemic attacks (TIAs) or cerebrovascular events.
Peripheral Arterial Interventions: Endovascular procedures, such as angioplasty, stenting, or atherectomy, are performed to treat lower extremity arterial disease and alleviate claudication symptoms in patients with peripheral artery disease (PAD).
Secondary Prevention Strategies: Beyond acute management, secondary prevention measures aim to prevent recurrent cardiovascular events and minimize disease progression through comprehensive risk factor modification, medication adherence, and ongoing surveillance of disease activity
Prevention of Atherosclerosis

Preventive strategies for atherosclerosis focus on addressing modifiable risk factors and promoting cardiovascular health through lifestyle modifications, health education, and targeted interventions. Key components of atherosclerosis prevention include:
Healthy Lifestyle: Encouraging individuals to adopt a healthy lifestyle characterized by balanced nutrition, regular physical activity, adequate sleep, stress management, and avoidance of harmful habits such as smoking or excessive alcohol consumption is paramount for reducing atherosclerosis risk
2. Dietary Modifications: Emphasizing a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and unsaturated fats while limiting intake of saturated fats, trans fats, cholesterol, sodium, and added sugars helps optimize lipid profiles, blood pressure, and overall cardiovascular health.
3. Physical Activity: Promoting regular exercise and physical activity is essential for maintaining cardiovascular fitness, weight management, insulin sensitivity, and endothelial function, thereby reducing the risk of atherosclerosis and its complications.
4. Tobacco Cessation: Implementing tobacco cessation programs and providing support for smoking cessation initiatives are critical for reducing atherosclerosis risk and improving overall cardiovascular outcomes.
5. Stress Management: Teaching stress reduction techniques such as mindfulness meditation, yoga, deep breathing exercises, or cognitive-behavioral therapy empowers individuals to cope with stressors effectively and mitigate their detrimental effects on cardiovascular health.
5 . Health Education: Educating individuals about the risks associated with atherosclerosis, the importance of early detection, and the benefits of preventive measures fosters informed decision-making and empowers individuals to take proactive steps towards cardiovascular wellness.
6. Regular Screening: Encouraging regular medical checkups and health screenings enables early detection of cardiovascular risk factors, facilitating timely intervention and personalized risk stratification for individuals at heightened risk of atherosclerosis.
Conclusion
In conclusion, atherosclerosis represents a significant public health challenge with far-reaching implications for cardiovascular morbidity and mortality. By majoring on the pathophysiology of atherosclerosis, identifying modifiable risk factors, and implementing evidence-based preventive strategies, healthcare providers can effectively mitigate the burden of atherosclerotic disease and promote cardiovascular health across diverse populations. Empowering individuals with knowledge, facilitating lifestyle modifications, and fostering a collaborative approach to atherosclerosis prevention and management are essential steps towards achieving optimal cardiovascular outcomes and enhancing quality of life for individuals affected by this pervasive condition.
As you navigate the complexities of cardiovascular health, remember that support and guidance are always available. Seek assistance from Expert Academic Assignment Help whenever needed.
Your journey in medicine is about more than just acquiring knowledge — it’s about embodying compassion, empathy, and continuous learning. Together, let’s strive for optimal cardiovascular health for all.
Email us at expertassignment46@gmail.com
Wishing you success and fulfillment in your medical journey.
Blood Physiology

Introduction:
Embarking on the intricate exploration of blood physiology and disorders is akin to embarking on a profound journey through the very essence of human existence. This comprehensive journey traverses the diverse components that collectively compose this vital fluid, unraveling the nuanced orchestration of physiological processes that sustain life. From the dynamic realms of blood plasma to the vigilant guardianship of red and white blood cells, this expedition seeks to illuminate the complexities of blood’s role in transporting essential nutrients, facilitating immune defenses, and maintaining the delicate equilibrium of the human body’s internal milieu.
Within the intricate tapestry of the circulatory system, blood stands as the lifeblood, a multifaceted composition of plasma, platelets, leukocytes, and erythrocytes. The adult human body, a vessel coursing with 4 to 5 liters of this life-sustaining elixir, serves as a testament to the elaborate harmony orchestrated within. Plasma, constituting 55% of the total blood volume, emerges as a luminous yellowish liquid, a reservoir of water, coagulants, plasma proteins, electrolytes, and immunoglobulins.
The embryonic stage marks the genesis of blood plasma, a symphony conducted by mesenchymal cells. The progression from albumin to globulin and other plasma proteins in adults is guided by reticuloendothelial cells in the liver, with collaborative assistance from bone marrow and spleen. The multifaceted functions of blood plasma underscore its indispensability, from coagulation and immune defense to maintaining osmotic pressure and regulating acid-base balance. It serves as the conduit for the transportation of nutrients, respiratory gases, hormones, and the excretion of waste products.
Temperature regulation, a finely tuned aspect of blood physiology, finds expression in the erythrocyte sedimentation rate (ESR). This diagnostic tool becomes pivotal in unraveling the intricate dance of fibrinogen during acute inflammatory conditions. Transitioning to the realm of erythrocytes, these biconcave discoidal cells, lacking a nucleus, become protagonists in the vital tasks of oxygen delivery and carbon dioxide collection. The narrative of erythropoiesis unfolds in the red bone marrow, a meticulously choreographed process ensuring the constant renewal of these cellular warriors.
Leucocytes, the vigilant defenders of the immune system, come to the forefront with their diverse cast of Neutrophils, Monocytes, Eosinophils, Basophils, and Lymphocytes. As the guardians of immune function, each type plays a unique role, orchestrating a symphony that responds to infections, cleanses dead cells, and regulates various immune responses.
The intricate process of hematopoiesis, transpiring in the red bone marrow, sets the stage for the production of red and white blood cells and platelets. Hormones stimulate this process, emanating from haemocystoblasts that give rise to lymphoid and myeloid stem cells. The formation of red blood cells unfolds in a meticulously orchestrated developmental journey, culminating in mature erythrocytes that ensure oxygen transport.
Yet, within this symphony of life, disorders cast shadows. Conditions like sickle cell anemia, leukemia, and hemochromatosis underscore the vulnerability of the hematologic system. Pediatrics, with its unique challenges, introduces a nuanced perspective, classifying disorders based on affected blood components and involving platelets, erythrocytes, and leucocytes.
In conclusion,
This journey through the intricacies of blood physiology and disorders reveals the marvels and vulnerabilities coursing through our veins. Blood, the fluid that sustains life, demands reverence for its complexities and resilience. From the transient lifespan of red blood cells to the vigilant defense mounted by white blood cells, the symphony of blood orchestrates the dance of life within us. As we navigate the river of existence, let us cherish the vital fluid that carries within it the essence of our being.
The journey into the depths of blood physiology takes us through a complex network of interconnected components, each playing a crucial role in maintaining the delicate balance of life. Blood plasma, the predominant liquid component, emerges as a multifaceted entity composed of water, coagulants, plasma proteins, electrolytes, and immunoglobulins. Its origins, traced back to the embryonic stage and guided by the intricate dance of reticuloendothelial cells, highlight the dynamic nature of plasma production in the adult human body.
The functions of blood plasma, akin to a maestro conducting a symphony, encompass coagulation, immune defense, maintenance of osmotic pressure, acid-base balance regulation, and the intricate task of transporting nutrients, respiratory gases, and hormones. The excretion of waste products from cellular metabolism is another crucial responsibility shouldered by this luminous yellowish liquid. Temperature regulation, reflected in the erythrocyte sedimentation rate (ESR), becomes a diagnostic tool unveiling the body’s response to acute inflammatory conditions.
Erythrocytes, the red blood cells, emerge as central protagonists in the oxygen transport narrative. Their biconcave discoidal structure, devoid of a nucleus, facilitates the essential tasks of delivering oxygen from the lungs to peripheral tissues and collecting carbon dioxide from peripheral cells for return to the lungs. The intricacies of erythropoiesis, unfolding in the red bone marrow, paint a picture of cellular renewal orchestrated with precision. The life cycle of erythrocytes, from anucleate immature cells to fully functioning mature cells, epitomizes the continuous process of blood cell replenishment.
Leucocytes, or white blood cells, emerge as the vigilant defenders of the immune system. Their diverse cast, including Neutrophils, Monocytes, Eosinophils, Basophils, and Lymphocytes, engages in a symphony of responses to infections, tissue regeneration, and immune regulation. Neutrophils, the first responders, combat bacteria and viruses, signaling other immune cells to join the defense. Monocytes, often referred to as the “garbage trucks” of the immune system, contribute to tissue regeneration and the removal of dead cells.
Eosinophils, with their presence in the digestive system, play a crucial role in combating invading bacteria and parasites. Basophils, representing a mere 1% of the total WBC count, become significant players in asthma, stimulating histamine release and contributing to inflammation. Lymphocytes, comprising B and T cells, produce antibodies and contribute to both humoral and cellular immunity. Their pivotal role in vaccine development adds a layer of significance to their function.
The pathophysiology of leucocytes introduces a diagnostic dimension, where elevated WBC counts can signal various conditions, including infection, inflammation, trauma, pregnancy, asthma, allergy, cancers, and intense physical exercise. Conversely, low WBC counts may indicate severe infections, bone marrow damage, autoimmune diseases, and splenic sequestration.
Hematopoiesis, the process of blood cell formation, becomes a focal point in understanding the intricacies of red and white blood cell production. The red bone marrow, a hub of hematopoietic activity, produces erythrocytes, leukocytes, and platelets. Hormones, including erythropoietin, regulate the rate of erythrocyte production, ensuring a constant supply to meet the body’s oxygen transport demands.
The formation of white blood cells and platelets, a collaborative effort involving the bone marrow, lymphatic tissues, and reticuloendothelial tissues, adds another layer to the symphony of hematopoiesis. Colony-stimulating factors and interleukins prompt red bone marrow to produce leukocytes, marshaling an army of WBCs to fend off attacks. Thrombopoietin, a hormone, accelerates platelet production, though the precise regulatory mechanisms remain an area of ongoing exploration.
As the journey through blood physiology unfolds, the narrative turns towards the shadowy realms of blood disorders. A myriad of conditions, ranging from sickle cell anemia and acute lymphoblastic leukemia to hypercoagulable disorders and iron deficiency anemia, cast shadows on the otherwise harmonious symphony of blood function. These disorders, rooted in anomalies affecting plasma, platelets, leukocytes, and erythrocytes, underscore the vulnerability of the hematologic system.
The pediatric perspective introduces a nuanced understanding of blood disorders, classifying them based on the affected blood components. Disorders of erythrocytes, labeled as red blood cell and iron disorders, manifest in various forms of anemia, including Iron-refractory iron deficiency anemia, Congenital sideroblastic anemia, and Megaloblastic anemia. Leukocytes disorders, affecting white blood cells, can result in conditions such as neutropenia, Shwachman-Diamond syndrome, and Kostmann Syndrome. Bleeding disorders, arising from malfunctioning plasma coagulants, lead to conditions like hemophilia and von Willebrand disease.
In reflection, the journey through blood physiology unveils the marvels and intricacies coursing through our veins. From the transient existence of red blood cells, living a mere four months before their components are recycled to form new blood cells, to the heightened defense mounted by white blood cells during illness, the symphony of blood orchestrates the dance of life within us. As we navigate the river of existence, let us cherish the vital fluid that carries within it the essence of our being.
Conclusion
In the vast tapestry of human existence, blood emerges as the fluid that intertwines with the very threads of life. The complexities and vulnerabilities revealed in the journey through blood physiology and disorders underscore the profound importance of this vital fluid. As we reflect on the symphony of functions performed by blood, from transporting nutrients to defending against pathogens and maintaining the intricate balance of the internal environment, we find ourselves immersed in the poetry of life.
The intricacies of blood physiology, encapsulated in the luminous yellowish liquid of blood plasma and the cellular ballet of erythrocytes and leucocytes, unveil the marvels coursing through our veins. The orchestration of hematopoiesis, unfolding in the red bone marrow, becomes a testament to the precision with which the body ensures a constant supply of red and white blood cells to meet its dynamic needs.
Yet, within this symphony of life, shadows loom in the form of blood disorders. Conditions such as sickle cell anemia, acute lymphoblastic leukemia, and hypercoagulable disorders remind us of the delicate equilibrium of the hematologic system. The pediatric perspective adds a layer of complexity, emphasizing the unique challenges faced by the young and the diverse manifestations of blood disorders affecting platelets, erythrocytes, and leucocytes.
In this reflective journey, we encounter the transient lifespan of red blood cells, living only four months before being replaced, and the dynamic response of white blood cells to infections, multiplying in their thousands to mount a defense. The symphony of blood is not merely a passive observer but an active participant in the ebb and flow of health and illness.
As we navigate the river of existence, let us cherish the vital fluid that carries within it the essence of our being. Red blood cells, akin to silent witnesses of our journey, break down, and their components are reused to give rise to new life. White blood cells, the defenders of our immune system, stand guard against invaders and foreign elements. The fluid reflection on life encapsulated in blood is a testament to the intricate dance of existence.
In conclusion, blood is not merely a physiological entity but a profound force that sustains life. From the pulsating dance of red and white blood cells to the orchestration of immune responses, every beat of this vital fluid echoes the rhythm of life within us. As we honor the marvels and vulnerabilities coursing through our veins, let us embrace the essence of blood — the fluid reflection on life that unites us all.
For Health Sciences Assignment Help,
Email us on, williamsfredrick46@gmail.com
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
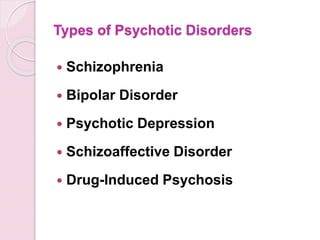
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.