10 Simple Tips For Caring For Your Heart.
10 Simple Tips for Caring for Your Heart.

The heart, a tireless worker at the core of our well-being, demands our attention and care. As we navigate through Heart Health Month this February, let’s explore ten simple yet impactful tips to ensure our hearts thrive. These practices, ranging from physical activity to laughter and dental hygiene, collectively contribute to a holistic approach to cardiovascular wellness.
1.Cardiovascular Exercise: A Heart’s Best Friend
Engaging in regular cardiovascular or aerobic activities is fundamental for heart health. Following the American Heart Association’s recommendations of 75 minutes of vigorous exercise or 150 minutes of moderate-intensity exercise weekly can significantly boost cardiorespiratory fitness. Activities such as running, cycling, or brisk walking not only elevate heart rate but also enhance overall cardiovascular function. The rhythmic contraction and relaxation of muscles during exercise contribute to improved blood flow and reduced strain on the heart.
2.Embrace a Smoke-Free Lifestyle
Quitting smoking is a paramount step in safeguarding your heart. Smoking damages both the heart and blood vessels, escalating the risk of cardiovascular diseases. Additionally, avoiding second-hand smoke is crucial, as it has been linked to heart attacks and strokes. The harmful chemicals in tobacco smoke lead to the narrowing of blood vessels, increasing the workload on the heart and elevating the risk of high blood pressure.
3.Prioritize Quality Sleep
Adequate sleep, often underestimated, plays a pivotal role in heart health. With at least seven hours of nightly rest, blood pressure lowers, and the body undergoes essential repair processes. Research underscores the correlation between poor sleep and heightened risks of high blood pressure, subsequently increasing the likelihood of heart diseases. Establishing a consistent sleep routine and creating a conducive sleep environment are crucial steps in promoting optimal cardiovascular health.
4.Regular Checkups: A Heart-Healthy Habit
Consistent visits to the doctor for heart health checkups are essential. Assessing risk factors such as diet, blood pressure, cholesterol, and family history enables early detection and management of potential issues. A proactive approach to heart health empowers individuals to make informed lifestyle choices. Regular checkups also provide an opportunity for healthcare professionals to offer personalized guidance on maintaining heart health through tailored interventions.
5.Laughter: The Heart’s Natural Tonic
Laughing, whether through entertainment or social interactions, yields surprising benefits for the heart. The act of laughter reduces artery inflammation, lowers stress hormones, and increases levels of good cholesterol. Integrating humor into daily life becomes a delightful prescription for heart health. Laughter promotes the release of endorphins, the body’s natural feel-good chemicals, which contribute to overall well-being and stress reduction.
6.Dental Hygiene and Heart Connection
Surprising as it may seem, maintaining good dental hygiene contributes to heart health. Studies reveal a link between poor dental health and the presence of bacteria in the bloodstream, impacting heart valves. Simple practices such as regular brushing can significantly decrease the risk of cardiovascular disease. Furthermore, regular dental checkups not only preserve oral health but also serve as a preventive measure against potential cardiovascular complications.
7.Fuel Your Heart with a Healthy Diet
A heart-healthy diet rich in fruits, whole grains, vegetables, and legumes significantly improves blood pressure and cholesterol levels. Steering clear of salty foods and saturated fats is crucial, as they contribute to elevated blood pressure and increased bad cholesterol. Incorporating omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, further supports heart health by reducing inflammation and promoting optimal functioning of blood vessels.
8.Maintaining a Healthy Weight: A Heart’s Delight
Striving for and maintaining a healthy weight is a powerful defense against heart disease and high blood pressure. A combination of a balanced diet, regular exercise, and mindful calorie intake promotes overall well-being and cardiovascular health. Excess weight puts additional strain on the heart, leading to conditions such as hypertension and diabetes. Adopting sustainable lifestyle changes, including portion control and regular physical activity, contributes to achieving and sustaining a healthy weight.
9.Hydration: The Heart’s Elixir
Staying adequately hydrated is a simple yet often overlooked aspect of heart care. Considering the heart’s continuous effort in pumping around 2,000 gallons of blood daily, increased water intake supports its optimal functioning. Dehydration can lead to thicker blood, making the heart work harder to pump blood through the vessels. Maintaining proper hydration levels ensures the efficient transport of nutrients and oxygen to cells, promoting overall cardiovascular health.
10.Stay Active, Break Inactivity
Combatting sedentary lifestyles is crucial in preserving heart health. Incorporating simple changes like taking the stairs, walking, playing with pets, or engaging in household chores helps keep the heart active, reducing the risk of cardiovascular diseases. Prolonged sitting has been associated with various health risks, including obesity and heart disease. Regular physical activity not only supports cardiovascular health but also contributes to weight management and overall well-being.
In conclusion, adopting these ten heart-healthy habits provides a comprehensive approach to cardiovascular wellness. Whether it’s the joyous act of laughter, the discipline of regular exercise, or the mindfulness of a balanced diet, each step contributes to the harmonious symphony of a healthy heart. As we celebrate Heart Health Month, let’s embrace these practices and gift our hearts the care they deserve. Through consistent efforts and lifestyle modifications, we can ensure that our hearts continue to beat with vitality and resilience.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance.
More Posts from Expertacademicassignmenthelp and Others
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com
Cervical Cancer

Introduction
Cervical cancer is a significant health concern affecting women worldwide. It arises from abnormal cell growth in the cervix, often linked to the human papillomavirus (HPV). Despite advancements in prevention and treatment, cervical cancer remains a leading cause of cancer-related deaths among women. Understanding its causes, symptoms, risk factors, and prevention strategies is crucial for early detection and effective management.
1. Understanding Cervical Cancer

Cervical cancer originates in the cervix, the lower part of the uterus connecting to the vagina.
HPV, a common sexually transmitted infection, is a primary cause of cervical cancer, with certain strains posing higher risks.
The body’s immune response typically clears HPV infections, but persistent infections can lead to cervical cell abnormalities and eventually cancer.
2. Symptoms and Diagnosis

Cervical cancer may not present noticeable symptoms initially, making regular screenings essential for early detection.
Symptoms can include abnormal vaginal bleeding, pelvic pain, and unusual discharge.
Diagnostic methods include Pap tests, HPV DNA testing, colposcopy, and biopsy to confirm cervical cancer and determine its stage.
3. Treatment Options

Treatment depends on the cancer’s stage, size, and type, as well as the patient’s overall health and preferences.
Surgical interventions, such as hysterectomy or removal of cancerous tissue, are common for early-stage cervical cancer.
Advanced stages may require a combination of surgery, chemotherapy, radiation therapy, or targeted therapy to eliminate cancer cells and prevent recurrence.
4. Risk Factors and Prevention
Several factors increase the risk of developing cervical cancer, including HPV infection, smoking, early sexual activity, and weakened immune system.
Prevention strategies include HPV vaccination, routine Pap tests for early detection of precancerous lesions, practicing safe sex, and smoking cessation.
5. Impact on Women’s Health

Cervical cancer not only affects physical health but also has emotional, social, and financial repercussions on women and their families.
Access to screening, vaccination, and treatment services significantly impacts the prognosis and survival rates of women diagnosed with cervical cancer.
Addressing disparities in healthcare access and promoting awareness about cervical cancer prevention are crucial for improving women’s health outcomes globally.
Conclusion
Cervical cancer remains a significant public health challenge despite advancements in prevention and treatment. Early detection through regular screenings and vaccination against HPV can significantly reduce the burden of this disease. Moreover, addressing risk factors such as smoking and promoting safe sexual practices are vital for cervical cancer prevention. By raising awareness, improving access to healthcare services, and advocating for comprehensive cervical cancer prevention programs, we can strive towards reducing the incidence and mortality associated with this preventable disease, ultimately enhancing women’s health and well-being worldwide.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
Cirrhosis Of The Liver

Introduction
Cirrhosis stands as a challenge in the narrative of liver disease, marking the culmination of a complex interplay of factors that converge to undermine the organ’s structural integrity and functional capacity. This condition, characterized by the progressive accumulation of scar tissue within the liver parenchyma, holds a cascade of physiological network that reverberate throughout the body, manifesting in a spectrum of symptoms and complications. From its inner onset to its profound implications for morbidity and mortality, cirrhosis generate the intricate interplay between genetic predisposition, environmental influences, and individual behaviors.
In this comprehensive discussion, we embark on an exploration of the multifaceted dimensions of cirrhosis, traversing its etiological underpinnings, clinical manifestations, diagnostic modalities, therapeutic strategies, and avenues for prevention and self-care. By delving into the intricacies of cirrhosis, we endeavor to elucidate the imperative of early recognition, proactive intervention, and holistic management in ameliorating its adverse sequelae and fostering optimal outcomes for affected individuals
Pathophysiology of Cirrhosis

Central to the pathogenesis of cirrhosis lies a complex interplay of molecular and cellular events that precipitate the gradual transformation of healthy hepatic tissue into fibrotic scar tissue. At the heart of this process lies fibrogenesis, wherein a multitude of cellular players, including hepatic stellate cells, inflammatory mediators, and extracellular matrix proteins, triggers a profibrotic milieu in response to persistent liver injury and inflammation. The ensuing deposition of collagen-rich scar tissue disrupts the structure of the liver lobules, impeding normal hepatocellular function and vascular dynamics.
Symptoms and Clinical Manifestations

The clinical presentation of cirrhosis spans a broad spectrum, reflecting the diverse array of physiological derangements engendered by advanced liver disease. Early-stage cirrhosis may manifest subtly, with nonspecific symptoms such as fatigue, malaise, and vague abdominal discomfort, often eluding timely diagnosis. However, as the disease progresses, overt signs of hepatic decompensation emerge, including jaundice, ascites, hepatic encephalopathy, and gastrointestinal bleeding, heralding the onset of life-threatening complications. Moreover, cirrhosis exerts systemic effects beyond the confines of the liver, precipitating coagulopathy, renal dysfunction, and metabolic disturbances.
Etiology and Risk Factors
Cirrhosis arises from an influence of etiological insults, encompassing a diverse spectrum of predisposing factors that contribute to hepatocellular injury and fibrogenesis. Foremost among these is chronic alcohol abuse, which inflicts direct hepatotoxic effects and potentiates oxidative stress and inflammatory cascades within the liver microenvironment. Additionally, viral hepatitis infections, particularly hepatitis B and C, constitute major drivers of cirrhosis worldwide, underscoring the imperative of vaccination and antiviral therapy in disease prevention and management. Other contributing factors include nonalcoholic fatty liver disease, autoimmune disorders, hereditary hemochromatosis, and biliary tract diseases, each exerting a unique influence on cirrhosis pathogenesis.
Diagnostic Modalities

Accurate diagnosis forms the linchpin of effective cirrhosis management, necessitating a judicious amalgamation of clinical symptoms, laboratory investigations, imaging modalities, and histopathological evaluation. Liver function tests serve as indispensable tools for gauging the synthetic and metabolic capacity of the liver, while imaging studies such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) afford insights into hepatic morphology, vascular dynamics, and the presence of focal lesions. Despite their utility, these modalities may be supplemented by liver biopsy, which remains the gold standard for assessing the degree of fibrosis and guiding therapeutic decisions, albeit fraught with procedural risks and sampling variability.
Treatment Strategies

While cirrhosis represents a chronic and irreversible condition, therapeutic interventions are geared toward monitoring disease progression, alleviating symptoms, and forestalling the onset of complications. Pharmacological therapies, including hepatoprotective agents, antifibrotic agents, and symptom-based medications, aim to attenuate hepatic inflammation, inhibit fibrogenesis, and ameliorate symptom burden in cirrhotic patients. Furthermore, endoscopic interventions such as variceal band ligation and trans jugular intrahepatic portosystemic shunting play a major role in the management of portal hypertension and its sequelae, including variceal bleeding and refractory ascites. For select individuals with end-stage liver disease, liver transplantation offers a definitive therapeutic option, affording a second lease on life and circumventing the inexorable progression of cirrhosis-related complications.
Self-Care and Lifestyle

Empowering individuals with cirrhosis to adopt proactive self-care measures constitutes a cornerstone of comprehensive disease management, emphasizing the role of lifestyle modifications, dietary interventions, and preventive strategies in optimizing health outcomes. Lifestyle modifications, including abstinence from alcohol, adherence to a liver-friendly diet, regular exercise, and smoking cessation, are paramount in attenuating hepatic inflammation, promoting metabolic homeostasis, and mitigating cardiovascular risk factors in cirrhotic patients. Additionally, vaccination against hepatitis viruses, avoidance of hepatotoxic medications, and judicious monitoring of comorbid conditions serve as essential pillars of preventive care, safeguarding against disease exacerbations and fostering long-term wellness in individuals with cirrhosis.
Conclusion
Cirrhosis emerges as a complex and a dangerous disease, syndrome characterized by progressive hepatic fibrosis, compromised organ function, and a plethora of systemic manifestations. The etiological heterogeneity of cirrhosis underscores the need for a personalized and multidisciplinary approach to disease management, Focusing to the unique pathophysiological mechanisms and clinical manifestations inherent to each individual. Through timely diagnosis, targeted interventions, and collaborative care, healthcare providers can mitigate the burden of cirrhosis, optimize patient quality of life, and prolong survival in affected individuals. As we navigate complexities of cirrhosis, a concerted emphasis on preventive measures, patient education, and therapeutic innovations holds the key to unlocking a brighter prognosis for those afflicted by this formidable liver disease.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
Blood cell

The blood cells serves as a comprehensive guide to understanding the intricacies of hematopoiesis, the process through which various blood cell types are formed and function in the human body. This detailed discussion aims to unravel the key aspects presented in the article, delving into the structure, functions, and disorders associated with;
Red blood cells (erythrocytes),
2.White blood cells (leukocytes), and
platelets (thrombocytes).
Blood Cell Types and Composition
At the core of the circulatory system lie three major types of blood cells: red blood cells, white blood cells, and platelets. These cellular components collectively contribute to 45% of blood tissue by volume, with the remaining 55% being plasma. This delicate balance underscores the dynamic nature of blood, serving as a conduit for various vital functions within the body.
1.Red Blood Cells (Erythrocytes)
The discussion commences with a focus on red blood cells, the primary carriers of oxygen in the bloodstream. Erythrocytes, characterized by their unique biconcave shape and lack of a nucleus, play a crucial role in gas exchange facilitated by the iron-containing protein hemoglobin. The intricate details of erythropoiesis, the process of RBC formation in the red bone marrow, offer a glimpse into the remarkable physiological mechanisms that ensure a constant supply of oxygen carriers. The staggering production rate of 2.4 million RBCs per second in adults highlights the body’s continuous demand for these essential cells. The information regarding the lifespan of RBCs (100–120 days) and their subsequent removal by the spleen adds another layer to our understanding of the life cycle of these vital cells. The absence of a nucleus in mature red blood cells, a unique characteristic among human cells, is highlighted. The pathological conditions of anemia and polycythemia are thoroughly explored, shedding light on the consequences of an imbalance in red blood cell count. Additionally, the erythrocyte sedimentation rate (ESR) provides valuable insights into the diagnostic tools used in assessing the health of red blood cells.
2.White Blood Cells (Leukocytes)
The immune system, our body’s defense mechanism, relies on white blood cells to combat infectious diseases and foreign materials. These leukocytes, originating from multipotent cells in the bone marrow, are categorized into granulocytes (basophils, eosinophils, neutrophils, mast cells) and agranulocytes (lymphocytes and monocytes). The discussion delves into the roles these distinct white blood cell types play in the human immune system, offering a nuanced understanding of their functions. The conditions of leukopenia and leukocytosis, indicating low and high white blood cell counts, respectively, are explored, emphasizing the diagnostic significance of monitoring these counts. The increased white blood cell count during infections and its association with hematological cancers underscore the pivotal role leukocytes play in our overall health.
3.Platelets (Thrombocytes)
The section on platelets elucidates their role in hemostasis, the process of preventing and stopping bleeding. These small, irregularly shaped cell fragments, derived from megakaryocytes, circulate in the blood and are essential for the formation of blood clots. The average lifespan of platelets, a mere 5 to 9 days, emphasizes the continuous production required for maintaining hemostatic balance. The normal range of platelet counts and the potential consequences of low or high platelet numbers provide valuable insights into the delicate equilibrium necessary for preventing excessive bleeding or the formation of thrombosis. Thrombocytopathy, a broad term encompassing disorders related to platelets, is discussed, including thrombocytopenia, thrombasthenia, and thrombocytosis. The intricate relationship between platelets and growth factors, as well as their role in wound healing, showcases the multifaceted contributions of these small but crucial cellular fragments.
Complete Blood Count (CBC): The article introduces the Complete Blood Count (CBC) as a vital diagnostic tool providing a comprehensive analysis of blood cell composition. The historical transition from manual counting to automated analyzers reflects the evolving landscape of medical technology, enhancing the efficiency and accuracy of blood cell analysis. The significance of CBC in offering an overview of a patient’s general health status is underscored, emphasizing its widespread use in medical diagnostics.
Historical Discoveries.
The historical perspective woven into the article traces the evolution of our understanding of blood cells. From Jan Swammerdam’s pioneering observation of red blood cells in 1658 to Paul Ehrlich’s techniques in staining blood films and differential blood cell counting in 1879, the narrative highlights key milestones in the establishment of hematology as a distinct field of medicine. The contributions of various scientists, including Antoni van Leeuwenhoek, Alfred Donne, and Gabriel Andal, collectively shaped our current knowledge of blood cells.
Conclusion
The blood cells provides a rich tapestry of information encompassing their structure, functions, and associated disorders. It serves as a comprehensive resource for understanding the dynamic nature of blood and the pivotal roles played by red blood cells, white blood cells, and platelets in maintaining homeostasis within the human body. The integration of historical discoveries adds depth to the narrative, highlighting the continuous quest for knowledge that has defined the field of hematology. This article not only serves as an educational tool but also showcases the remarkable advancements in medical science and technology that have propelled our understanding of blood cells to new heights. As we unravel the mysteries of hematopoiesis, we gain valuable insights into the machinery that sustains life within our veins.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance.
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
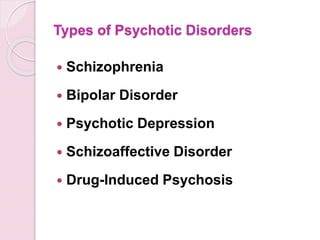
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science

The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work

Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader

A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
First Aid Instructions for 10 Medical Emergencies

Introduction
First aid is the immediate care provided to a sick or injured person, often serving as a crucial bridge until professional medical help arrives. While formal first aid training is ideal, there are basic life-saving steps that everyone should be aware of. This article outlines first aid instructions for 10 common medical emergencies, along with practical tips and a comprehensive first aid kit list.
1.Stopped Heart (Cardiac Arrest)

In the event of a stopped heart, immediate action is crucial:
Initiate CPR (cardiopulmonary resuscitation) to maintain blood circulation.
Use an AED (automated external defibrillator) if available to shock the heart.
Call 911 and continue care until professional help arrives.
2. Bleeding

Effective bleeding control is essential
Apply direct pressure with a clean cloth or bandage to control bleeding.
Elevate the bleeding body part if possible to reduce blood flow.
Seek immediate medical help for severe bleeding.
3. Choking
https://cdn-images-1.medium.com/max/800/0*acrWmV_gxPmZh9JX
Swift response is vital when someone is choking:
Perform the Heimlich maneuver for a conscious choking victim.
If unconscious, initiate CPR and call for help.
Monitor airway and breathing.
4. Burns
Proper handling of burns is crucial for minimizing damage:
Stop the burning process by cooling the burn with running water.
For minor burns, use a light gauze bandage and avoid breaking blisters.
Seek medical attention for severe burns.
5. Blisters
Appropriate care can aid in the healing of blisters:
Leave small, unopened blisters alone to promote healing.
For larger, painful blisters, clean, drain, and apply antibiotic ointment.
Monitor for signs of infection.
6. Broken Bone/Fracturey
https://cdn-images-1.medium.com/max/800/0*4NouIgQSR_QHj-t6.jpeg
Careful management of fractures is essential:
Call 911 for severe fractures and avoid moving the person if a spinal injury is suspected.
Immobilize the injured area with a splint, elevate, and apply a cold pack for pain.
Seek prompt medical attention.
7. Sprains
Proper first aid can alleviate symptoms of sprains:
Rest the injured limb, apply a cold pack, and elevate if possible.
Seek medical attention for severe pain, inability to bear weight, or signs of infection.
Follow R.I.C.E. (Rest, Ice, Compression, Elevation) principles.
8. Nosebleeds
https://cdn-images-1.medium.com/max/800/0*jJd3qZg5Q8xI_IHf
Effective nosebleed management is essential:
Lean forward and pinch the nose just below the bridge to control bleeding.
Apply a cold pack and seek medical attention for persistent or frequent nosebleeds.
Address underlying causes such as dry air or trauma.
9. Frostbite
Timely response is critical to treating frostbite:
Get out of the cold and gradually warm the affected area with warm water.
Avoid rubbing the affected area, and do not use dry heat sources.
Seek medical attention for severe cases.
10. Bee Sting
Proper care for bee stings is vital, especially for allergic reactions:
Remove the stinger immediately using a straight-edged object.
Monitor for signs of an allergic reaction and call 911 if necessary.
Clean the area, apply a cold pack, and use antihistamines for swelling.
First Aid Kit List
https://cdn-images-1.medium.com/max/800/0*WM_HfAvd_-O5fZMC
A well-prepared first aid kit is an essential tool for handling emergencies. The kit should include:
Adhesive bandages in various sizes and shapes
Gauze pads and compress dressings
Adhesive cloth tape, latex gloves, and antiseptic wipes
Antibiotic ointment and hydrocortisone ointment
A breathing barrier for performing CPR
Instant cold compress, tweezers, and an oral thermometer
Emergency blanket for warmth and comfort
Conclusion
While formal first aid training is highly recommended, understanding the basics of immediate care can make a significant difference in emergencies. The outlined first aid instructions cover a range of medical situations, and having a well-stocked first aid kit further enhances preparedness. Quick and appropriate action can be a crucial factor in saving lives during medical emergencies. Remember, being informed and ready can make you a valuable first responder in times of need.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us expertassignment46@gmail.com for professional assistance and guidance
Cardiovascular System

The cardiovascular system, an intricate symphony of physiological marvels, stands as the linchpin of human existence. Woven intricately with the tapestry of life, it encompasses the heart, the rhythmic conductor, and a sprawling network of blood vessels navigating the human terrain. As we embark on this comprehensive expedition, our journey aims to unearth the multifaceted dimensions of the cardiovascular system, unraveling its nuanced functions, delving deep into its anatomical complexities, scrutinizing the spectrum of conditions it contends with, and exploring the exhaustive care practices imperative for the perpetual maintenance of its optimal health.
Overview and Function:
At the epicenter of biological vitality, the cardiovascular system unfurls its canvas, orchestrating a perpetual ballet of life-sustaining processes. Beyond the rudimentary task of blood transportation, this intricate network emerges as a dynamic conduit, ensuring the orchestrated delivery of oxygen, nutrients, and the expeditious removal of metabolic waste. The heart, a majestic organ with chambers that mirror the elegance of a grand ballroom, takes center stage, propelling nearly 2,000 volume of litters of life-essential fluid through the intricate channels of 1. Arteries, 2. veins, and 3. capillaries on a daily basis.
Anatomy:
Positioned majestically in the anatomical Centre of the chest, the heart assumes the role of the epicenter of the cardiovascular narrative. Intricately interwoven with blood vessels that traverse the entirety of the corporeal landscape, these conduits form a sophisticated network, ensuring the pervasive reach of oxygen, nutrients, and the removal of cellular detritus. This anatomical choreography mimics the intricate networks of water or sewer pipes, with large arteries and veins akin to main conduits beneath city streets, branching into diminishing tributaries that eventually culminate in microscopic capillaries facilitating the exchange of life’s essentials between blood and tissue cells.
Conditions and Disorders:
The robust fortitude of the cardiovascular system is not immune to the challenges posed by a diverse spectrum of conditions, frequently manifesting as impediments within the intricate vascular highways. These afflictions, akin to tempests in the circulatory teacup, include
1.Arrhythmia
2. myocardial infarction
3.malfunctioning heart valves
4.heart failure
5.Aneurysms
6.Strokes
7.Atherosclerosis
and an assortment of vascular abnormalities. The discernment of early warning signs, whether it be the thunderous symphony of chest pain, the breathless crescendo of shortness of breath, or the subtle nuances indicative of strokes, becomes the harbinger of timely intervention and meticulous management.
Tests and Treatments:
Within the echelons of cardiovascular health, the diagnostic arsenal assumes the mantle of an indispensable compass, navigating the terrain of system functionality. A cacophony of tests, including electrocardiograms capturing the heart’s melodic rhythm, blood tests unveiling biochemical orchestrations, echocardiograms crafting visual symphonies of the heart’s dynamics, and advanced imaging techniques such as cardiac CT and MRI, paints a comprehensive portrait of cardiovascular vitality. Treatments, akin to a therapeutic sonnet, are tailored with precision, embracing an expansive repertoire ranging from medical procedures like angioplasty, intricate surgeries addressing valvular intricacies, and the artistry of medication and lifestyle adjustments woven into the fabric of holistic care.
As we draw the curtains on this extensive odyssey through the labyrinthine landscapes of the cardiovascular system, the indomitable resilience of this physiological magnum opus comes to light. To comprehend its functions, to marvel at its anatomical symphony, and to acknowledge the variegated conditions it faces is to wield the reins of self-empowerment over cardiovascular well-being. In the realm of proactive health, the pillars of regular exercise, judicious blood pressure control, adherence to a heart-attuned diet, and the harmonious cadence of lifestyle adjustments stand as bulwarks fortifying the citadel of the heart and blood vessels. As we traverse this expansive exploration, let us not merely scrutinize but marvel at the complexity of the cardiovascular system, embracing the mantle of stewardship bestowed upon us to foster enduring health, vitality, and the pulsating rhythm of life itself.
The cardiovascular system, an intricate symphony of physiological marvels, stands as the linchpin of human existence. Woven intricately with the tapestry of life, it encompasses the heart, the rhythmic conductor, and a sprawling network of blood vessels navigating the human terrain. As we embark on this comprehensive expedition, our journey aims to unearth the multifaceted dimensions of the cardiovascular system, unraveling its nuanced functions, delving deep into its anatomical complexities, scrutinizing the spectrum of conditions it contends with, and exploring the exhaustive care practices imperative for the perpetual maintenance of its optimal health.
Overview and Function:
At the epicenter of biological vitality, the cardiovascular system unfurls its canvas, orchestrating a perpetual ballet of life-sustaining processes. Beyond the rudimentary task of blood transportation, this intricate network emerges as a dynamic conduit, ensuring the orchestrated delivery of oxygen, nutrients, and the expeditious removal of metabolic waste. The heart, a majestic organ with chambers that mirror the elegance of a grand ballroom, takes center stage, propelling nearly 2,000 volume of litters of life-essential fluid through the intricate channels of 1. Arteries, 2. veins, and 3. capillaries on a daily basis.
Anatomy:
Positioned majestically in the anatomical Centre of the chest, the heart assumes the role of the epicenter of the cardiovascular narrative. Intricately interwoven with blood vessels that traverse the entirety of the corporeal landscape, these conduits form a sophisticated network, ensuring the pervasive reach of oxygen, nutrients, and the removal of cellular detritus. This anatomical choreography mimics the intricate networks of water or sewer pipes, with large arteries and veins akin to main conduits beneath city streets, branching into diminishing tributaries that eventually culminate in microscopic capillaries facilitating the exchange of life’s essentials between blood and tissue cells.
Conditions and Disorders:
The robust fortitude of the cardiovascular system is not immune to the challenges posed by a diverse spectrum of conditions, frequently manifesting as impediments within the intricate vascular highways. These afflictions, akin to tempests in the circulatory teacup, include
1.Arrhythmia
2. myocardial infarction
3.malfunctioning heart valves
4.heart failure
5.Aneurysms
6.Strokes
7.Atherosclerosis
and an assortment of vascular abnormalities. The discernment of early warning signs, whether it be the thunderous symphony of chest pain, the breathless crescendo of shortness of breath, or the subtle nuances indicative of strokes, becomes the harbinger of timely intervention and meticulous management.
Tests and Treatments:
Within the echelons of cardiovascular health, the diagnostic arsenal assumes the mantle of an indispensable compass, navigating the terrain of system functionality. A cacophony of tests, including electrocardiograms capturing the heart’s melodic rhythm, blood tests unveiling biochemical orchestrations, echocardiograms crafting visual symphonies of the heart’s dynamics, and advanced imaging techniques such as cardiac CT and MRI, paints a comprehensive portrait of cardiovascular vitality. Treatments, akin to a therapeutic sonnet, are tailored with precision, embracing an expansive repertoire ranging from medical procedures like angioplasty, intricate surgeries addressing valvular intricacies, and the artistry of medication and lifestyle adjustments woven into the fabric of holistic care.
As we draw the curtains on this extensive odyssey through the labyrinthine landscapes of the cardiovascular system, the indomitable resilience of this physiological magnum opus comes to light. To comprehend its functions, to marvel at its anatomical symphony, and to acknowledge the variegated conditions it faces is to wield the reins of self-empowerment over cardiovascular well-being. In the realm of proactive health, the pillars of regular exercise, judicious blood pressure control, adherence to a heart-attuned diet, and the harmonious cadence of lifestyle adjustments stand as bulwarks fortifying the citadel of the heart and blood vessels. As we traverse this expansive exploration, let us not merely scrutinize but marvel at the complexity of the cardiovascular system, embracing the mantle of stewardship bestowed upon us to foster enduring health, vitality, and the pulsating rhythm of life itself.
For Health Sciences Assignment Help;
Email us at; williamsliason@outlook.com
Anatomy of the Heart

Introduction
The heart, an extraordinary organ vital to human life, serves as the epicenter of the circulatory system, tirelessly pumping blood throughout the body. Its intricate anatomy and physiological functions are the focus of extensive study and admiration in medical science. This comprehensive overview aims to delve into the intricate details of the heart’s anatomy, its valves, the circulation of blood within its chambers, and the critical role it plays in sustaining life.
Anatomy of the Heart
The heart, nestled within the middle mediastinum, is encased by a protective serous sac known as the pericardium. Structurally resembling a quadrangular pyramid, its base aligns posteriorly while its apex points anteriorly towards the thoracic wall. The heart’s significance is unparalleled; while one can survive without certain organs, the absence of a heart is incompatible with life.
The heart’s architecture is meticulously organized, with distinct surfaces and margins showing its boundaries. Its internal structure comprises four chambers: two atria and two ventricles. The right atrium and ventricle receive deoxygenated blood from systemic veins and propel it towards the lungs for oxygenation. Conversely, the left atrium and ventricle receive oxygen-rich blood from the lungs and distribute it throughout the body’s systemic vessels.
Heart Valves

Critical to maintaining unidirectional blood flow, the heart is equipped with valves that separate its chambers and prevent backflow. The atrioventricular valves, including the tricuspid and mitral valves, regulate blood flow between atria and ventricles. Semilunar valves, namely the pulmonary and aortic valves, guard the exits of the ventricles, ensuring blood flows into the appropriate vessels without regurgitation.
Blood Flow Through the Heart
The heart’s rhythmic contractions, orchestrated by the cardiac cycle, facilitate the circulation of blood through its chambers. Systole, characterized by ventricular contraction, propels blood into pulmonary and systemic circuits. Diastole, the phase of relaxation, allows chambers to refill with blood. This cyclical process ensures continuous nutrient and oxygen delivery to tissues and organs.
Coronary Circulation

To sustain its relentless activity, the heart receives its own blood supply through the coronary circulation. Coronary arteries originate from the aorta, branching to supply myocardial tissue. Cardiac veins collect deoxygenated blood and converge at the coronary sinus, which empties into the right atrium. This intricate network ensures the heart’s metabolic demands are met, essential for its function.
Great Vessels of the Heart
The great vessels, including the aorta, pulmonary artery, and pulmonary veins, facilitate blood transport to and from the heart. Major branches of the aorta distribute oxygenated blood throughout the body, while the superior and inferior vena cavae return deoxygenated blood from systemic circulation. These vessels play a pivotal role in maintaining systemic homeostasis.
Clinical Insights
Understanding the heart’s anatomy is crucial in diagnosing and managing various cardiac pathologies. Conditions such as angina pectoris, infective endocarditis, and congenital heart diseases underscore the importance of cardiac health. Medical professionals employ diverse interventions, ranging from pharmaceuticals to surgical procedures, to address these conditions and optimize patient outcomes.
In conclusion, the heart’s intricate structure and physiological functions underscore its indispensable role in sustaining life. A deeper comprehension of its anatomy and circulation elucidates the complexities of cardiovascular health and underscores the importance of preventive care and medical intervention in maintaining cardiac well-being.
This overview provides a comprehensive exploration of the heart’s anatomy and functions, offering insights into its pivotal role in human physiology and healthcare.
Best of luck in the strategic study of the heart,
In case you’re experiencing any challenges in the study journey,
Email us at;williamsassignmenthelpfredrick@gmail.com
What Are The Stages of Fetal Growth During Pregnancy?

The development of a fetus during pregnancy is a complex and remarkable process, marked by significant changes and growth each month. This journey is typically divided into three stages known as trimesters, each lasting approximately three months. For Healthcare professionals we discuss fetal development in terms of weeks. Here’s a detailed overview of what entails during each month of pregnancy.
a) First Trimester

The first trimester of pregnancy encompasses weeks 1 through 12 and is characterized by the initial formation and rapid development of the embryo. This period is critical for establishing the foundation of the future baby’s organs and body systems. The first trimester is often associated with the onset of pregnancy symptoms, such as nausea, fatigue, and hormonal changes.
Month 1 (Weeks 1–4)
Weeks 1–2: The first two weeks of pregnancy are technically considered a preparatory period. During this time, the body releases hormones and prepares the uterus for a potential pregnancy. This period includes ovulation, where an egg is released from the ovary. If fertilization occurs, the zygote forms and marks the beginning of pregnancy.
Week 3: Fertilization occurs when a sperm cell meets the egg, creating a zygote. This single-celled entity undergoes rapid cell division as it travels down the fallopian tube towards the uterus.
Week 4: The zygote becomes a blastocyst, which is a cluster of cells that implants itself into the uterine lining. The amniotic sac and placenta begin to form, playing crucial roles in protecting and nourishing the developing embryo. By the end of this month, the blastocyst is about 2 millimeters long, roughly the size of a poppy seed.
Month 2 (Weeks 5–8)
The second month of pregnancy marks significant developmental milestones as the embryo transitions into more complex forms.
Week 5: The neural tube, which will become the brain and spinal cord, begins to form. The heart, initially a simple tube, starts to pulse, setting the stage for the development of the circulatory system.
Week 6: Limb buds appear, which will eventually become arms and legs. Structures for the ears, eyes, and mouth start to take shape. Blood cells begin to form, and circulation starts within the embryo.
Week 7: The process of ossification starts as bones begin replacing the soft cartilage, and the formation of the genitals commences. The embryo now resembles a tadpole due to its prominent tail.
Week 8: Major organs and body systems continue to develop. The hands and feet start to form web-like structures, and the umbilical cord, which provides nutrients and oxygen to the embryo, is fully developed. By the end of this month, the embryo, now referred to as a fetus, is about 0.5 to 1 inch long, similar to a black bean.
Month 3 (Weeks 9–12)
The third month of pregnancy is marked by significant growth and maturation of the embryo, transitioning into a more recognizable human form.
Week 9: Teeth and taste buds begin to form. The fetus starts developing muscles, and its body takes on a more human appearance, although the head remains disproportionately large.
Week 10: Limbs and digits are fully formed, and the external genitals start to develop, although they are not yet visible on an ultrasound. The placenta continues to grow, providing essential nutrients to the fetus.
Week 11: The fetus begins to move spontaneously, exploring its surroundings by opening and closing its fists and mouth. The bones harden, though the skin remains translucent. Facial features such as the nose and lips become more defined.
Week 12: All essential organs, limbs, bones, and muscles are present and will continue to mature and develop. The fetus is about 2.5 to 3 inches long, roughly the size of a plum. At this stage, the risk of miscarriage decreases significantly, and many women begin to feel relief from early pregnancy symptoms like morning sickness.
Second Trimester

The second trimester of pregnancy spans from weeks 13 to 26. This period is often considered the most comfortable phase of pregnancy as many early symptoms subside, and the risk of miscarriage decreases. The fetus undergoes significant growth and development, and the mother begins to feel fetal movements, known as quickening.
Month 4 (Weeks 13–16)
During the fourth month, the fetus continues to develop rapidly, and its features become more distinct.
Week 13: Vocal cords form, and the fetus’s head starts to grow proportionally to the rest of the body. The fetus begins to practice breathing movements by inhaling and exhaling amniotic fluid, which helps develop the lungs.
Week 14: The skin starts to thicken and fine hair, known as lanugo, begins to grow. The fetus can bring its fingers to its mouth and may start sucking its thumb. External genitals are fully formed, and fingerprints start to develop.
Week 15: The intestines and ears move to their final positions. The fetus practices more purposeful movements, such as thumb-sucking and smiling. The developing nervous system allows the fetus to respond to external stimuli, such as light and sound.
Week 16: The fetus can hear and respond to external sounds. Its eyes, although still closed, can perceive light. By the end of this month, the fetus is about 5 inches long and weighs around 4 ounces, comparable to an avocado.
Month 5 (Weeks 17–20)
The fifth month of pregnancy is marked by increased fetal activity and continued growth.
Week 17: Fat begins to accumulate under the skin, providing insulation and energy reserves. The fetus’s skin is covered with a protective coating called vernix, which prevents it from becoming chapped by the amniotic fluid.
Week 18: The fetus is covered in lanugo, which helps keep it warm and provides an additional layer of protection. The fetus starts to establish a sleep-wake cycle, and its movements become more noticeable to the mother.
Week 19: The fetus’s movements, including kicks and punches, become more frequent and noticeable. Unique fingerprints are fully formed, and the fetus may start to experience hiccups.
Week 20: Nails develop fully, and the sensory areas of the brain mature, allowing the fetus to respond more actively to its environment. By the end of this month, the fetus is about 9 to 10 inches long and weighs around 1 pound.
Month 6 (Weeks 21–24)
The sixth month of pregnancy is a period of significant development, particularly in the nervous and respiratory systems.
Week 21: Coordinated limb movements become more frequent, and the fetus’s bone marrow begins producing blood cells.
Week 22: The fetus’s grasping reflex strengthens, and it can touch its surroundings, including its own body and the umbilical cord. It can hear internal sounds, such as the mother’s heartbeat and external sounds, such as voices and music.
Week 23: The fetus’s viability outside the womb increases, though intensive medical care would be necessary if it were born prematurely. The fetus starts rapidly accumulating fat, which is essential for temperature regulation after birth.
Week 24: Lung development progresses, although the lungs are not yet mature enough for the fetus to breathe independently. The fetus is about 12 inches long and weighs around 2 pounds.
Third Trimester

The third trimester of pregnancy spans from weeks 27 to 40 and is characterized by rapid growth and final preparations for birth. During this period, the fetus gains weight quickly and undergoes the final stages of development necessary for survival outside the womb.
Month 7 (Weeks 25–28)
During the seventh month, the fetus continues to grow and develop reserves of body fat.
Week 25: Increased body fat makes the fetus’s skin less wrinkled and more plump. The nervous system matures rapidly, enhancing the fetus’s ability to respond to stimuli.
Week 26: Melanin production begins, contributing to the skin and eye color. The lungs start producing surfactant, a substance that helps the lungs function properly after birth.
Week 27: The fetus’s eyes open, and it develops eyelashes. The fetus begins to develop regular sleep and wake patterns, and its movements become more coordinated.
Week 28: The fetus may begin to position itself head-down in preparation for birth. By the end of this month, the fetus is about 14 to 15 inches long and weighs between 2 to 3 pounds.
Month 8 (Weeks 29–32)
The eighth month of pregnancy involves continued maturation and growth of the fetus, with a focus on brain development.
Week 29: The fetus’s movements become more distinct as space in the uterus becomes cramped. The brain develops rapidly, allowing the fetus to control its body temperature more effectively.
Week 30: The fetus’s brain continues to grow, and it can process information and respond to stimuli. The fetus begins to establish more distinct patterns of activity and rest.
Week 31: The fetus’s skin loses its translucency as fat accumulates beneath it. Most organs, except for the brain and lungs, are fully developed and ready for birth.
Week 32: The fetus is about 17 to 18 inches long and weighs up to 5 pounds. The brain continues to develop rapidly, and the fetus can hear and respond to a variety of sounds.
Month 9 (Weeks 33–36)
During the ninth month, the fetus continues to grow and mature, preparing for birth.
Week 33: The fetus’s bones harden, although the skull remains soft and flexible to facilitate passage through the birth canal.
Week 34: The protective vernix coating thickens, providing additional protection to the fetus’s skin.
Week 35: Brain growth continues, and the fetus’s brain is now capable of regulating essential body functions.
Week 36: The lanugo covering the fetus’s body begins to disappear, and hair growth occurs on the head. The fetus is about 17 to 19 inches long and weighs 6 to 7 pounds.
Month 10 (Weeks 37–40)
The final month of pregnancy is a period of final preparations for birth, with the fetus reaching full maturity.
Week 37: The fetus’s toenails reach the tips of its toes. It continues to gain weight rapidly, preparing for the energy demands of life outside the womb.
Week 38: The fetus’s weight gain continues, and it starts to shed the vernix coating. The fetus moves lower into the pelvis in preparation for birth.
Week 39: The fetus is considered full-term and continues to develop and gain weight. It measures about 18 to 20 inches long and weighs between 7 to 9 pounds.
Week 40: The fetus is ready for birth. Its organs are fully developed and capable of functioning independently. The fetus positions itself head-down in the pelvis, preparing for delivery.
Throughout pregnancy, the fetus undergoes substantial growth and development, preparing for the transition to life outside the womb. Regular monitoring and care by healthcare providers are crucial to ensure the health and well-being of both the mother and the fetus. This comprehensive journey from a single cell to a fully developed baby highlights the incredible complexity of human development.
Expert Academic Assignment Help specializes in supporting medical students to study fetal growth during pregnancy. Our assistance includes study materials, tutoring, assignment help, and exam preparation, ensuring students understand fetal development. We provide mentorship, empowering students to excel academically and become competent healthcare professionals. Email: expertassignment46@gmail.comac