The Pathophysiology Of Hypertension
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com
More Posts from Expertacademicassignmenthelp and Others
14 Common Lung Diseases

Introduction
Lung diseases represent some of the most severe health threats globally. The rise of industrialization, environmental pollution, and tobacco usage significantly contribute to the prevalence of these diseases. This article, outlines the most common lung diseases, their symptoms, causes, and treatments.
1. Pneumonia

Pneumonia is an inflammation of the lung parenchyma caused by bacteria, viruses, fungi, or other pathogens. It poses a significant risk to the elderly, immunocompromised individuals, and those with chronic conditions but can also affect healthy individuals. Pneumonia can be classified based on the causative agent, such as bacterial pneumonia (e.g., Streptococcus pneumoniae), viral pneumonia (e.g., influenza virus), or fungal pneumonia (e.g., Pneumocystis jirovecii).
Symptoms
Fever
Cough with sputum
Chest pain
Shortness of breath
Fatigue
Sweating and shaking chills
Nausea, vomiting, or diarrhea (less common)
Diagnosis Diagnosis of pneumonia typically involves a combination of patient history, physical examination, chest X-rays, and sputum cultures. Blood tests may also be conducted to identify the causative agent.
Treatment Depending on the cause, treatments may include:
Antibiotics for bacterial pneumonia.
Antiviral medications for viral pneumonia.
Antifungal therapies for fungal pneumonia. Supportive care such as rest, fluids, and over-the-counter medications to reduce fever and manage pain can also alleviate symptoms. In severe cases, hospitalization may be required to provide intravenous antibiotics, oxygen therapy, or mechanical ventilation.
2. Bronchitis

Bronchitis involves the inflammation of the bronchial tubes, which carry air to and from the lungs. It can be acute, often following colds or the flu, or chronic, usually resulting from smoking or long-term exposure to irritants like pollution or dust.
Symptoms
Persistent cough (productive or dry)
Sputum production (clear, white, yellowish-gray, or green)
Fatigue
Shortness of breath
Slight fever and chills
Chest discomfort
Diagnosis Diagnosis typically involves a physical examination, where a doctor listens to the patient’s lungs with a stethoscope. Additional tests, such as a chest X-ray, sputum tests, or pulmonary function tests, may be conducted to rule out other conditions like pneumonia or asthma.
Treatment
Acute bronchitis: Symptomatic treatment includes rest, fluids, and over-the-counter pain relievers and cough medications. Inhalers or nebulizers may be prescribed to ease breathing.
Chronic bronchitis: Management may involve bronchodilators, steroids, and pulmonary rehabilitation. Smoking cessation and avoiding lung irritants are crucial for treatment.
3. Chronic Obstructive Pulmonary Disease (COPD)

COPD is a progressive, irreversible disease characterized by chronic inflammation of the airways, primarily due to smoking, environmental pollutants, or long-term exposure to respiratory irritants. COPD includes chronic bronchitis and emphysema, conditions that often coexist and lead to airflow obstruction.
Symptoms
Chronic cough
Sputum production
Shortness of breath, especially during physical activities
Wheezing
Chest tightness
Frequent respiratory infections
Fatigue
Unintended weight loss (in advanced stages)
Diagnosis COPD is diagnosed through a combination of patient history, physical examination, and spirometry, a test that measures the amount of air a person can exhale and how quickly they can do so. Chest X-rays, CT scans, and arterial blood gas analysis may also be used.
Prevention and Treatment Preventive measures include:
Smoking cessation
Vaccinations (influenza and pneumococcal vaccines)
Reducing exposure to lung irritants
Treatments involves;
Bronchodilators to relax the muscles around the airways
Inhaled steroids to reduce airway inflammation
Pulmonary rehabilitation programs
Oxygen therapy for severe cases
Surgery (e.g., lung volume reduction surgery or lung transplant) in advanced cases
4. Lung Cancer

Lung cancer involves the uncontrolled growth of malignant cells in the lung tissues. Major risk factors include smoking, exposure to secondhand smoke, exposure to carcinogens (e.g., asbestos, radon), and genetic predisposition.
Types
Small cell lung cancer (SCLC): Often linked to heavy smoking, SCLC is aggressive and spreads quickly.
Non-small cell lung cancer (NSCLC): More common and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Symptoms
Persistent cough
Chest pain
Weight loss
Hemoptysis (coughing up blood)
Shortness of breath
Hoarseness
Bone pain (in advanced stages)
Headache (if cancer spreads to the brain)
Diagnosis Diagnosis involves imaging tests (chest X-rays, CT scans, PET scans), sputum cytology, and tissue biopsy. Molecular testing may be done to identify specific genetic mutations that can be targeted with specific treatments.
Treatment
Surgery to remove the tumor or part of the lung
Chemotherapy to kill cancer cells
Radiation therapy to destroy cancer cells or shrink tumors
Targeted drug therapies to attack specific genetic changes in cancer cells
Immunotherapy to help the immune system fight cancer
5. Pleurisy
Pleurisy, or pleuritis, is the inflammation of the pleura, the tissue lining the lungs and chest cavity. It can be caused by infections (viral, bacterial, or fungal), injuries, autoimmune diseases (e.g., lupus, rheumatoid arthritis), or other underlying conditions.
Symptoms
Sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing
Shortness of breath
Cough
Fever (if infection is present)
Diagnosis Diagnosis involves a physical examination, chest X-rays, ultrasound, CT scans, and blood tests to identify the underlying cause. Thoracentesis, a procedure to remove and analyze pleural fluid, may be performed.
Treatment Treatment depends on the underlying cause and may include:
Antibiotics for bacterial infections
Antiviral medications for viral infections
Anti-inflammatory medications (e.g., NSAIDs) to reduce pain and inflammation
Pain management with medications
Thoracentesis to drain excess fluid from the pleural space
6. Pulmonary Embolism

A pulmonary embolism (PE) occurs when a blood clot, usually originating in the legs (deep vein thrombosis), travels to the lungs, blocking blood flow and causing tissue damage. Risk factors include prolonged immobility, surgery, cancer, and certain genetic conditions.
Symptoms
Sudden shortness of breath
Chest pain (may be sharp and worsen with deep breathing or coughing)
Cough (sometimes with bloody sputum)
Rapid or irregular heartbeat
Lightheadedness or dizziness
Leg pain or swelling (if DVT is present)
Diagnosis: Diagnosis involves imaging tests such as chest X-rays, CT pulmonary angiography, and ventilation-perfusion (V/Q) scans. D-dimer blood tests and ultrasound of the legs may also be conducted.
Treatment Immediate treatment includes:
Anticoagulants (blood thinners) to prevent further clotting
Thrombolytics (clot-dissolving medications) for severe cases
Surgical or catheter-based procedures to remove the clot
Long-term anticoagulation therapy to prevent recurrence
7. Pulmonary Edema

Pulmonary edema is the accumulation of fluid in the lung alveoli, making breathing difficult. It can result from heart failure (cardiogenic pulmonary edema), acute respiratory distress syndrome (ARDS), or exposure to high altitudes (non-cardiogenic pulmonary edema).
Symptoms
Difficulty breathing (dyspnea), especially when lying down
Rapid heartbeat (tachycardia)
Wheezing or gasping for breath
Coughing up frothy, pink-tinged sputum
Excessive sweating
Cyanosis (bluish skin or lips)
Diagnosis Diagnosis involves physical examination, chest X-rays, and blood tests. Echocardiography and pulmonary artery catheterization may be used to determine the underlying cause and severity.
Treatment Treatment involves addressing the underlying cause and may include:
Diuretics to remove excess fluid
Medications to improve heart function (for cardiogenic pulmonary edema)
Supplemental oxygen or mechanical ventilation
Treating underlying conditions such as infections or high altitude exposure
8. Pulmonary Fibrosis

Pulmonary fibrosis is the thickening and scarring of lung tissue, leading to reduced oxygen absorption. Causes include chronic exposure to environmental pollutants, infections, genetic factors, and autoimmune diseases (e.g., scleroderma).
Symptoms
Shortness of breath (dyspnea)
Persistent dry cough
Fatigue
Unexplained weight loss
Aching muscles and joints
Clubbing (widening and rounding) of the fingertips or toes
Diagnosis Diagnosis involves a combination of patient history, physical examination, imaging tests (chest X-rays, high-resolution CT scans), pulmonary function tests, and sometimes lung biopsy. Blood tests may be used to identify underlying autoimmune diseases.
Treatment While there is no cure for pulmonary fibrosis, treatments focus on symptom management and slowing progression:
Medications such as pirfenidone and nintedanib to slow disease progression
Oxygen therapy
Pulmonary rehabilitation
Lung transplant in severe cases
9. Pneumoconiosis
Pneumoconiosis is a lung disease caused by inhaling dust particles, such as asbestos, silica, or coal dust, leading to lung scarring. It is a type of occupational lung disease commonly seen in miners, construction workers, and industrial workers.
Symptoms:
Chronic cough
Shortness of breath
Chest tightness
Progressive loss of lung function
Diagnosis: Diagnosis involves a detailed occupational history, physical examination, chest X-rays, and CT scans. Pulmonary function tests may also be conducted to assess the extent of lung damage.
Treatment Treatment includes:
Avoiding further exposure to dust
Medications to manage symptoms, such as bronchodilators and corticosteroids
Respiratory therapies
Pulmonary rehabilitation
10. Pulmonary Arterial Hypertension (PAH)
PAH is a form of high blood pressure affecting the arteries in the lungs and the right side of the heart. It can be idiopathic, familial, or associated with other conditions such as connective tissue diseases, congenital heart disease, or chronic liver disease.
Symptoms
Breathing difficulties (dyspnea), especially during physical activities
Dizziness or fainting (syncope)
Chest pain
Fatigue
Swelling in the ankles, legs, and abdomen (edema)
Cyanosis (bluish lips and skin)
Diagnosis Diagnosis involves echocardiography, right heart catheterization, chest X-rays, and CT scans. Blood tests and pulmonary function tests may also be conducted to assess lung and heart function.
Treatment Treatment strategies include:
Medications to relax blood vessels and improve blood flow, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs
Diuretics to reduce fluid retention
Oxygen therapy
Anticoagulants to prevent blood clots
In severe cases, surgical procedures such as atrial septostomy or lung transplant
11. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene, leading to thick, sticky mucus buildup in the lungs and other organs. This results in frequent infections, respiratory issues, and digestive problems.
Symptoms
Persistent cough with thick mucus
Recurrent lung infections
Wheezing or shortness of breath
Poor growth and weight gain in children
Salty-tasting skin
Severe constipation
Frequent greasy, bulky stools
Diagnosis Diagnosis involves genetic testing, sweat chloride tests, and newborn screening. Pulmonary function tests, chest X-rays, and sputum cultures may also be conducted to assess lung health.
Treatment Management includes:
Medications to thin mucus, antibiotics to treat infections, and bronchodilators to open airways
Chest physiotherapy to clear mucus
Enzyme supplements and high-calorie diets to manage digestive issues
Newer therapies targeting the underlying genetic defect, such as CFTR modulators
12. Respiratory Distress Syndrome (RDS)
RDS primarily affects premature infants due to a lack of surfactant, a substance necessary to keep the lungs open and facilitate gas exchange. Risk factors include premature birth, maternal diabetes, and multiple births.
Symptoms
Rapid, shallow breathing
Grunting sounds while breathing
Nasal flaring
Chest retractions (pulling in of the chest muscles)
Cyanosis (bluish color of the skin and mucous membranes)
Diagnosis Diagnosis involves clinical assessment, chest X-rays, and blood gas analysis to measure oxygen and carbon dioxide levels. Prenatal tests can also help identify at-risk pregnancies.
Treatment Treatment includes:
Surfactant replacement therapy to improve lung function
Mechanical ventilation or continuous positive airway pressure (CPAP) to support breathing
Oxygen therapy
Supportive care such as fluids and nutrition
13. Sarcoidosis
Sarcoidosis is characterized by the growth of granulomas (small clusters of inflammatory cells) in the lungs and other organs, likely as an immune response to unknown triggers. The exact cause remains unclear, but genetic and environmental factors are believed to play a role.
Symptoms
Dry cough
Shortness of breath
Chest pain
Fatigue
Fever
Swollen lymph nodes
Skin lesions (e.g., erythema nodosum)
Diagnosis Diagnosis involves a combination of patient history, physical examination, chest X-rays, CT scans, and pulmonary function tests. Biopsy of affected tissues may be performed to confirm the presence of granulomas.
Treatment While sarcoidosis is often self-limiting and may resolve without treatment, severe cases may require:
Corticosteroids to reduce inflammation
Immunosuppressive medications (e.g., methotrexate, azathioprine)
Antimalarial drugs (e.g., hydroxychloroquine) for skin lesions
Regular monitoring and follow-up care to manage chronic cases
14. Asthma
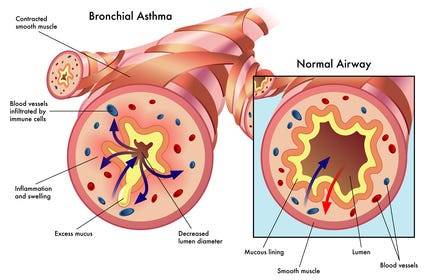
Definition and Causes: Asthma is a chronic inflammatory condition of the airways, causing episodes of wheezing, coughing, and chest tightness, often triggered by allergens, exercise, cold air, or respiratory infections. Genetic and environmental factors contribute to its development.
Symptoms
Wheezing
Shortness of breath
Chest tightness
Coughing, especially at night or early morning
Increased mucus production
Diagnosis: Diagnosis involves a detailed medical history, physical examination, and lung function tests (spirometry, peak flow measurement). Allergy testing and chest X-rays may also be conducted to identify triggers and rule out other conditions.
Treatment Management includes:
Avoiding known triggers
Inhalers (bronchodilators for quick relief, corticosteroids for long-term control)
Long-term control medications (e.g., leukotriene modifiers, long-acting beta agonists)
Immunotherapy (allergy shots) for severe allergies
Asthma action plans to manage symptoms and prevent attacks
Conclusion
Lung diseases encompass a wide range of conditions, each with distinct causes, symptoms, and treatments. Preventive measures such as avoiding smoking, reducing exposure to environmental pollutants, and timely vaccinations can significantly reduce the risk of developing many of these diseases. Early diagnosis and appropriate management are crucial in improving outcomes and quality of life for individuals affected by lung diseases. For personalized medical advice and treatment, consult with healthcare professionals.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: expertassignment46@gmail.com for professional guidance.
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
What is The Process Of Sleep?

Introduction
Sleep is a complex physiological process that encompasses more than merely closing one’s eyes and drifting into unconsciousness. It is an active state of unconsciousness in which the brain, while relatively at rest, remains responsive primarily to internal stimuli. Despite extensive research, the precise purpose of sleep remains incompletely understood. Several prominent theories attempt to elaborate the purpose of sleep, including the Inactivity Theory, Energy Conservation Theory, Restoration Theory, and Brain Plasticity Theory.
Inactivity Theory involves that inactivity during nighttime reduces the risk of predation, offering an evolutionary advantage. This theory suggests that creatures that remained inactive during the night were less likely to fall victim to predators, thereby enhancing survival and reproductive success.
Energy Conservation Theory proposes that the primary function of sleep is to decrease energy demand during periods when it is less efficient to procure food, supported by evidence of a 10% reduction in metabolism during sleep. This theory aligns with the observation that many species exhibit lower metabolic rates during sleep, thereby conserving energy.
Restorative Theory asserts that sleep facilitates the repair and replenishment of cellular components, as evidenced by processes such as muscle repair, tissue growth, protein synthesis, and hormone release occurring predominantly during sleep. This theory is supported by findings that various restorative functions are activated during sleep, promoting physical health and well-being.
Brain Plasticity Theory suggests that sleep is essential for neural reorganization and brain development, particularly in infants and children who require extensive sleep. This theory underscores the role of sleep in cognitive functions, learning, and memory consolidation.
These theories collectively indicate that sleep serves multiple functions, and a combination of these concepts likely explains the necessity of sleep.
Function

Sleep follows a cyclical pattern, alternating between two major phases: Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep. NREM sleep is subdivided into stages 1 through 3, each representing different depths of sleep characterized by unique brain wave patterns, muscle tone, and eye movement patterns. NREM sleep comprises approximately 75–80% of total sleep time, while REM sleep accounts for the remaining 20–25%.
The sleep cycle begins with a short NREM stage 1 phase, progresses through NREM stages 2 and 3, and culminates in REM sleep. This cycle repeats throughout the night, with initial cycles lasting 70–100 minutes and subsequent cycles 90–120 minutes. As the night progresses, the duration of REM sleep increases, eventually comprising up to 30% of the sleep cycle later in the night. Typically, an individual undergoes 4 to 5 sleep cycles per night.
NREM Stage 1: A shallow sleep stage lasting 1–7 minutes, characterized by rhythmical alpha waves (8–13 Hz). This stage represents the transition from wakefulness to sleep, during which the individual can be easily awakened.
NREM Stage 2: A deeper sleep state lasting 10–25 minutes initially, progressing to encompass 50% of the total sleep cycle. EEG recordings during this stage show sleep spindles and K-complexes. Memory consolidation is believed to occur primarily in this stage.
NREM Stage 3: Lasting 20–40 minutes initially, characterized by high-voltage, slow-wave frequency on EEG. This stage, also known as slow-wave sleep (SWS), is crucial for restorative processes.
REM Sleep: Responsible for dreaming, characterized by muscle paralysis (except for the extraocular muscles) and sawtooth waveforms on EEG. REM sleep involves increased brain activity and is essential for cognitive functions such as learning, memory consolidation, and emotional regulation.
Mechanism

The regulation of sleep involves a delicate balance between homeostatic processes and circadian rhythms.
a) Homeostatic Processes
These processes reflect the body’s need for sleep, increasing the pressure to sleep the longer one stays awake. Sleep generation is initiated within the ventrolateral preoptic nucleus (VLPO) of the anterior hypothalamus, which inhibits arousal regions in the brain, including the tuberomammillary nucleus, lateral hypothalamus, locus coeruleus, dorsal raphe, laterodorsally segmental nucleus. Hypocretin (orexin) neurons in the lateral hypothalamus facilitate this process synergistically.
b) Circadian Rhythm
The circadian rhythm, or the internal body clock, regulates the sleep-wake cycle and is influenced by light levels detected by the retina. The hypothalamus, particularly the suprachiasmatic nucleus (SCN),initiates this rhythm. Melatonin, produced by the pineal gland, modulates the circadian rhythm, with levels peaking at night and decreasing during the day. The circadian rhythm typically spans approximately 24.2 hours, and variations in body temperature also play a role, with lower temperatures in the morning and higher temperatures in the evening.
NREM sleep involves a functional disconnection between the brain stem, thalamus, and cortex, maintained by hyperpolarizing GABA neurons. During this phase, corticothalamic neurons signal the thalamus, causing hyperpolarization of thalamic reticular neurons, resulting in delta waves from both thalamic reticular and cortical pyramidal sources.
REM sleep is generated by “REM-on neurons” in the mesencephalic and pontine cholinergic neurons. The pedunculopontine tegmental nucleus and lateral dorsal tegmental neurons trigger desynchronized cortical waveforms. The tonic component of REM sleep is parasympathetically mediated, while the phasic component is sympathetically mediated.
Related Testing
Polysomnography is the primary modality used to study sleep. It is a comprehensive test that includes an electrocardiogram (ECG), electroencephalography (EEG), electrooculography (EOG), electromyography (EMG), and oxygen saturation monitoring.
ECG: Measures the electrical activity of the heart to detect cardiac anomalies such as arrhythmias.
EEG: Non-invasively records brain wave activity to determine sleep stages and detect neurological abnormalities.
EOG: Measures eye movements to differentiate between NREM and REM sleep.
EMG: Assesses muscle activity, particularly in the respiratory muscles and peripheral limbs, to detect excessive movement or muscle tension during sleep.
Oxygen Saturation: Monitors respiratory function to ensure adequate oxygenation during sleep.
Clinical Significance

a) .Insomnia
Insomnia is characterized by difficulty falling or staying asleep and is the most common sleep disorder. It is often related to psychological stressors, poor sleep environments, irregular sleep schedules, or excessive mental, physical, or chemical stimulation. Treatment typically involves cognitive-behavioral therapy (CBT), sleep hygiene practices, and, in some cases, pharmacological interventions.
b) .Obstructive Sleep Apnea (OSA)
OSA is marked by repeated pauses in breathing during sleep due to airway obstruction, often caused by obesity or weak pharyngeal muscles. This condition leads to hypoxia and frequent awakenings, preventing restful sleep. OSA is classified into mild, moderate, and severe based on the frequency of apneic episodes per hour. Treatment options include Continuous Positive Airway Pressure (CPAP) therapy, Bilevel Positive Airway Pressure (BiPAP) therapy, mandibular advancement devices, and surgical interventions such as uvulopalatopharyngoplasty, adenotonsillectomy, and maxillomandibular advancement.
c) .Central Sleep Apnea
Central Sleep Apnea (CSA) results from a failure in the central respiratory drive, leading to diminished breathing effort during sleep. Conditions such as congenital central hypoventilation syndrome (Ondine’s curse) or congestive heart failure can cause CSA. Treatment includes CPAP, BiPAP, Adaptive-servo-ventilation, and medications like acetazolamide or theophylline.
d) .Mixed Sleep Apnea
Mixed Sleep Apnea, also known as Complex Sleep Apnea, involves symptoms of both OSA and CSA. This condition typically manifests when patients with OSA develop CSA symptoms upon treatment with CPAP. Treatment often involves low-pressure CPAP therapy.
d) .Ghrelin-Leptin Abnormalities
Sleep duration significantly influences hunger-regulating hormones, with reduced sleep linked to lower levels of leptin and higher levels of ghrelin. Leptin, produced by adipose cells, inhibits hunger, while ghrelin, produced in the gastrointestinal tract, stimulates appetite. Imbalances in these hormones due to inadequate sleep can increase appetite and contribute to higher body mass index (BMI), potentially leading to obesity. This phenomenon is particularly relevant in patients with OSA, where increased BMI is a risk factor.
e) .Narcolepsy
Narcolepsy is characterized by a loss of orexin (hypocretin) neurons, leading to unstable transitions between sleep and wakefulness. Symptoms include excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations. Narcolepsy type 1 involves a significant loss of orexin neurons, while type 2 is less severe. Treatment focuses on managing symptoms with medications such as stimulants, sodium oxybate, and selective serotonin and norepinephrine reuptake inhibitors (SSRIs and SNRIs), along with lifestyle modifications.
f) .Somnambulism (Sleepwalking)
Somnambulism, or sleepwalking, involves performing activities while in a state of combined sleep and wakefulness. Sleepwalking is associated with increased slow-wave sleep and sleep deprivation, and there is evidence of a genetic predisposition. Treatment includes ensuring a safe sleep environment, improving sleep hygiene, and, in some cases, pharmacological interventions such as benzodiazepines.
Conclusion
Sleep is a physiological process essential for various bodily functions, including energy conservation, cellular repair, brain development, and cognitive function. The precise mechanisms and purposes of sleep remain areas of active research. Understanding the complexities of sleep and its disorders is crucial for promoting overall health and addressing various medical conditions. Ongoing research aims to fully understand the mechanisms of sleep and its broad implications for human health..
Navigating the rigorous demands of medical studies requires support and collaboration. Whether you’re a nursing student, medical doctor, clinical student, pharmacist, or any other medical practitioner, don’t hesitate to seek assistance. Utilize available resources and value teamwork and mentorship.
For personalized support, expert advice, and comprehensive resources, contact Expert Academic Assignment Help at expertassignment46@gmail.com With the right support and dedication, you can achieve your goals and make significant contributions to healthcare.
Alopecia Areata

Introduction
Alopecia areata is a complex autoimmune disease that targets the body’s hair follicles, resulting in patchy hair loss. While medications and therapies offer hope for regrowth, severe cases may pose challenges in responding to treatment. This comprehensive discussion will delve into the various aspects of alopecia areata, from its symptoms and causes to diagnosis, treatment options, prevention, and the psychosocial impact it can have on individuals.
Symptoms and Causes

Alopecia areata manifests as patchy hair loss on various body parts, commonly affecting the scalp. Understanding its classifications, which include total loss (alopecia areata totalis), full-body hair loss (alopecia areata universalis), diffuse thinning (diffuse alopecia areata), and a band of hair loss (ophiasis alopecia areata), provides insights into the diverse ways it can affect individuals.
Certain factors increase the likelihood of developing alopecia areata, such as being a child, having a family history of the condition, or having autoimmune disorders like diabetes, lupus, or thyroid disease. The prevalence of alopecia areata is significant, with nearly 7 million people in the United States affected, and it is the second-most common form of hair loss.
Psychosocial Impact of Alopecia Areata

Beyond its physical effects, alopecia areata can significantly impact an individual’s psychosocial well-being. The emotional toll of experiencing patchy hair loss, potential nail issues, and the uncertainty of its progression can lead to stress, anxiety, and depression. Recognizing these psychological aspects is crucial for holistic management.
Diagnosis and Tests

Diagnosing alopecia areata involves a thorough examination by healthcare providers, considering medical history, the pattern of hair loss, and familial autoimmune conditions. Additional tests, such as scalp examinations, hair analysis, scalp biopsies, and blood tests, may be conducted to confirm the diagnosis.
Management and Treatment

Managing alopecia areata is a nuanced process, and complete cure remains elusive. Treatment options include corticosteroids, administered through injections, oral pills, or topical applications. Minoxidil (Rogaine®), phototherapy, platelet-rich plasma therapy, and topical immunotherapy are among the diverse approaches employed. The unpredictability of alopecia areata necessitates tailored treatment plans, and response times may vary from weeks to months.
Can Alopecia Areata Go Away?
While alopecia areata itself doesn’t vanish, effective treatments can control hair loss. However, severe forms, such as alopecia areata totalis and alopecia areata universalis, pose greater challenges in treatment response.
Prevention and Outlook

Preventing alopecia areata is currently not feasible. The condition tends to have periods of remission and flare-ups throughout an individual’s life. Outlook varies, with mild cases showing remission and more severe forms being less responsive to available treatments.
Living With Alopecia Areata

Coping with alopecia areata involves adopting various cosmetic and protective measures. These include using makeup to conceal hair loss, wearing coverings like wigs or scarves, and protecting the eyes if eyelashes are affected. A balanced diet and vitamin D supplements may contribute to overall health. Avoiding stress, protecting the skin from the elements, and choosing hair products carefully are essential aspects of self-care.
Conclusion
In conclusion, alopecia areata is a multifaceted condition that extends beyond its physical symptoms. Understanding its classifications, causes, and the psychosocial impact on affected individuals is crucial for comprehensive management. While there is no cure, advancements in treatments offer hope for controlling hair loss and stimulating regrowth. A holistic approach, including psychological support and self-care strategies, empowers individuals to navigate life with alopecia areata confidently. As research progresses, further insights into this autoimmune disorder will likely pave the way for more effective interventions, improving the quality of life for those affected by alopecia areata.
We wish you all the best in your studies and knowledge of Alopecia Disease condition.
In case of any challenges during your studies and education journey, don’t hesitate to contact us for a flawless process.
Email us through;
williamsassignmenthelpfredrick@gmail.com
Leukemia in Children

Introduction
Leukemia in children presents a formidable challenge, demanding meticulous management and treatment. This detailed discussion aims to devolve into various facets of childhood leukemia, encompassing its definition, types, causes, risk factors, symptoms, diagnosis, treatment modalities, potential complications, preventive measures, and strategies for supporting a child living with leukemia.
Understanding Leukemia in Children

1. Definition
Leukemia is a hematological malignancy affecting the blood and bone marrow. Its prominence in childhood stems from the rapid proliferation of abnormal blood cells, disrupting the delicate balance within the body.
2. Types of Blood Cells
Understanding the roles of
Red blood cells (erythrocytes),
2.platelets (thrombocytes), and
3.white blood cells (leukocytes)
Is fundamental. An imbalance in these cells results in a spectrum of symptoms, from anemia to increased infection susceptibility.
3. Types of Leukemia

. Acute Lymphocytic Leukemia (ALL): Predominant in children.
Acute Myelogenous Leukemia (AML): The second most common type.
Hybrid or Mixed Lineage Leukemia: A rare amalgamation of ALL and AML.
Chronic Myelogenous Leukemia (CML): Uncommon in children.
Chronic Lymphocytic Leukemia (CLL): Extremely rare in pediatric cases.
Juvenile Myelomonocytic Leukemia (JMML): A rare type with unique growth characteristics.
Causes and Risk Factors
1. Causes
The exact etiology of childhood leukemia remains elusive. Genetic mutations in bone marrow cell genes may occur sporadically or, in some instances, be inherited.
2. Risk Factors
Exposure to Radiation.
Particularly high levels.
Inherited Syndromes.
Down syndrome.
Li-Fraumeni syndrome.
Immune System Conditions.
Inherited disorders affecting immune function.
Family History.
Having a sibling with leukemia elevates the risk.
Symptoms of Leukemia in Children
A diverse array of symptoms underscores leukemia’s impact on children, including;
.Pale skin
. Fatigue
.Dizziness
.Headaches
.Shortness of breath
.Frequent infections
.Fever
. Easy bruising
.Bleeding
.Bone or Joint pain, and
.Abdominal swelling.
Diagnosis:
1. Procedures:
.Blood Tests (Complete Blood Count — CBC): Essential for initial assessment.
Bone Marrow Aspiration or Biopsy: Crucial in detecting leukemia cells.
Lab Tests: Precisely determine leukemia type.
Diagnostic Imaging: X-rays, ultrasound,
lymph node biopsy, and
Lumbar puncture offer a comprehensive diagnostic perspective.
2. Classification
Unlike other cancers, leukemia is not staged but rather classified into groups, subtypes, or both based on type and specific characteristics, aiding in targeted treatment approaches.
Treatment Options:
1. Primary Treatments:
Blood Transfusions: Address low blood counts, bleeding, or infections.
Chemotherapy: The mainstay, killing or inhibiting cancer cells.
Radiation Therapy: High-energy X-rays to target and eradicate cancer cells.
Stem Cell Transplant: Involves high-dose chemotherapy followed by stem cell replacement.
Targeted Therapy: Specific medications tailored to combat certain types of leukemia.
Immunotherapy: Enhances the body’s immune system to combat cancer cells.
Complications:
1. Short-term:
Serious Infections: Resulting from compromised immune function.
Severe Bleeding: A consequence of low platelet levels.
Thickened Blood: Accumulation of leukemia cells in the bloodstream.
2. Long-term:
Leukemia Recurrence: A persistent concern.
Development of Other Cancers: A potential consequence of treatment.
Heart and Lung Problems: Arising from the impact of leukemia or its treatment.
Learning Issues and Growth Delays: Impacts on cognitive development and physical growth.
Fertility Problems and Bone Issues: Osteoporosis as a potential long-term complication.
Prevention:
Preventing childhood leukemia remains challenging, with a focus on caution regarding unnecessary exposure to radiation, especially in diagnostic procedures involving pregnant women and children.
Supporting a Child with Leukemia:
1. Ongoing Care:
Regular visits to oncologists and healthcare providers are crucial for monitoring and addressing emerging issues.
2. Balanced Lifestyle:
Managing eating difficulties and encouraging appropriate exercise play a vital role in supporting overall health.
3. Emotional Support:
Seeking counseling or participating in support groups helps both the child and their family navigate the emotional challenges associated with leukemia.
4. Follow-up Appointments:
Attending all scheduled appointments ensures continuous monitoring and timely intervention if complications arise.
When to Contact Healthcare Provider:
Prompt communication with healthcare providers is essential if the child experiences fever, worsening symptoms, new symptoms, or side effects from treatment.
Key Points Summary:
Leukemia necessitates a comprehensive approach, involving diagnosis, tailored treatment, and ongoing monitoring.
Varied symptoms demand timely medical attention for an optimal prognosis.
Treatment modalities, including chemotherapy and stem cell transplant, are tailored to the specific leukemia type.
Complications, both short-term and long-term, underscore the importance of ongoing follow-up care.
Prevention is limited, with a focus on minimizing unnecessary radiation exposure.
Comprehensive support, encompassing medical, emotional, and lifestyle aspects, is essential for the child’s well-being.
Next Steps:
1. Follow-up Care:
Continued regular check-ups and imaging tests remain integral to post-treatment monitoring.
2. Communication:
Maintaining open and transparent communication with healthcare providers ensures timely intervention if issues arise.
3. Research:
Inquiring about ongoing clinical trials or new treatments enables families to stay informed about emerging possibilities.
Conclusion:
Childhood leukemia mandates a collaborative effort from medical professionals, caregivers, and support networks to optimize outcomes and enhance the quality of life for affected children. As the landscape of pediatric oncology evolves, the commitment to advancing treatment options and minimizing the impact of complications remains paramount, offering hope for a brighter future for children navigating the complexities of leukemia.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance
Breast Cancer

Introduction
Breast cancer, a multifaceted and prevalent disease, poses a significant health challenge globally, transcending gender lines with its potential impact. Characterized by the abnormal proliferation of cells within breast tissue, breast cancer’s complex etiology remains an area of intense study and concern. Despite notable advancements in medical science and increased awareness, it continues to be a leading cause of morbidity and mortality worldwide. This comprehensive discussion aims to delve into the intricacies of breast cancer, encompassing its causes, risk factors, prevention strategies, diagnostic modalities, treatment options, and the evolving landscape of supportive care.
Causes and Risk Factors

Understanding the underlying causes and risk factors associated with breast cancer is paramount in developing effective prevention and management strategies. While the precise etiology of breast cancer remains elusive, various genetic, hormonal, environmental, and lifestyle factors contribute to its onset and progression. Genetic predispositions, such as mutations in the BRCA1 and BRCA2 genes, significantly elevate the risk of developing breast cancer. Additionally, hormonal influences, including early onset of menstruation, late menopause, and hormone replacement therapy, play a crucial role in disease pathogenesis. Lifestyle factors such as excessive alcohol consumption, obesity, lack of physical activity, and exposure to environmental carcinogens further augment the risk profile.
Preventive Measures

Empowering individuals with knowledge about preventive measures is essential in mitigating the burden of breast cancer. Promoting regular breast self-examinations, clinical breast examinations, and mammographic screenings facilitates early detection and intervention. Emphasizing lifestyle modifications, including maintaining a healthy weight, adopting a balanced diet rich in fruits and vegetables, limiting alcohol intake, and engaging in regular physical activity, can reduce the risk of breast cancer. For individuals with a heightened risk due to genetic predispositions or familial history, prophylactic surgeries, such as mastectomy or oophorectomy, and chemo preventive agents offer viable preventive options.
Diagnostic Modalities

Advances in diagnostic modalities have revolutionized the early detection and diagnosis of breast cancer, enabling prompt initiation of treatment and improved clinical outcomes. Mammography remains the cornerstone of breast cancer screening, capable of detecting abnormalities such as microcalcifications, masses, or architectural distortions. Complementary imaging techniques, including ultrasound, magnetic resonance imaging (MRI), and molecular breast imaging (MBI), enhance diagnostic accuracy, particularly in women with dense breast tissue or high-risk profiles. Biopsy procedures, such as core needle biopsy or surgical excision, facilitate histopathological examination, enabling precise diagnosis and classification of breast lesions.
Treatment Options

Tailoring treatment strategies to individual patient characteristics and disease parameters is essential in optimizing therapeutic outcomes in breast cancer. The treatment landscape encompasses a multidisciplinary approach, integrating surgical, medical, and radiation oncology interventions. Surgical options range from breast-conserving surgeries, such as lumpectomy or segmental mastectomy, to radical procedures like total mastectomy or modified radical mastectomy, depending on tumor size, location, and extent of spread. Adjuvant therapies, including chemotherapy, hormonal therapy, targeted therapy, and immunotherapy, aim to eradicate residual disease, prevent recurrence, and improve overall survival. Radiation therapy, administered either postoperatively or as a primary modality in selected cases, targets residual tumor cells, minimizing locoregional recurrence rates.
Supportive Care and Survivorship

Recognizing the holistic needs of breast cancer patients and survivors is integral in promoting comprehensive care and ensuring optimal quality of life. Supportive care interventions, including symptom management, psychosocial support, nutritional counseling, and rehabilitation services, address the multifaceted challenges associated with cancer diagnosis and treatment. Survivorship programs, focusing on survivorship care planning, surveillance for recurrence, long-term monitoring of treatment-related complications, and health promotion initiatives, facilitate the transition from active treatment to survivorship. Engaging patients and caregivers in survivorship care planning fosters empowerment, resilience, and a sense of agency in navigating the post-treatment phase.
Conclusion
In conclusion, breast cancer represents a formidable health challenge with profound implications for affected individuals, families, and communities worldwide. While significant strides have been made in understanding its pathophysiology, enhancing diagnostic capabilities, and expanding treatment options, concerted efforts are warranted to address existing gaps in prevention, early detection, and access to care. By fostering collaborative partnerships among stakeholders, advocating for evidence-based interventions, and promoting health equity, we can strive towards a future where breast cancer incidence and mortality rates are substantially reduced. Through continued innovation, education, and advocacy, we can transform the landscape of breast cancer care, offering hope, support, and healing to those impacted by this pervasive disease.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
How Does The Drug Got Excreted / Eliminated From The Body?

Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: expertassignment46@gmail.com
Your excellence our pride.
How to Write Nursing Research Papers The process of nursing research paper writing involves exploring relevant issues within the field and proposing viable solutions. The complexity of nursing necessitates in-depth research, analytical thinking, and critical analysis. Topics may span various areas such as psychiatric nursing, healthcare management, evidence-based medicine, clinic hygiene, home-based healthcare, healthcare practices, and ethics, all of which revolve around the central goal of alleviating patient suffering and addressing their psychological well-being. Before delving into the writing process, it is crucial to determine the type of research paper – analytical or argumentative. Analytical research papers involve a specific analysis of issues or literary texts, employing designs like question/answer, comparison/contrast, problem/solution, cause/effect, hypothesis/proof, or change over time. On the other hand, argumentative research papers focus on presenting diverse viewpoints on a debatable issue, requiring an investigation of different studies to provide compelling arguments while addressing opposing views objectively. Selecting an appropriate topic is a critical aspect of the research paper process. The chosen topic should be specific, relevant to nursing, interesting to the writer, and within the prescribed length and format guidelines. Topics like Nursing Science During the 20th Century, Nurses’ Safety on the Working Place, or The Importance of Neonatal Care Nursing exemplify suitable choices. Once a topic is chosen, the next step involves sourcing information from reliable primary, secondary, and tertiary sources. Primary sources include original materials like academic journals, interviews, surveys, and court records. Secondary sources analyze or describe primary sources, encompassing books, articles, encyclopedias, dictionaries, and textbooks. Tertiary sources aid in organizing or locating both primary and secondary sources and typically involve databases and indexes. Pre-writing activities, such as brainstorming, freewriting, mindmapping, and outlining, play a pivotal role in organizing ideas before the actual writing process. These activities help in collecting and structuring major points and arguments effectively. In terms of formatting styles, the APA style is commonly used in nursing research papers. It dictates a specific structure with a title page, abstract, main body, and reference page. In-text citations follow a specific format with the author's last name and year of publication. The entire paper is typed in twelve-point Times New Roman font. The basic structure of a nursing research paper includes a title page containing the title, running head, author’s name, and institutional affiliation. The abstract, written on a separate page, provides a summary of key points, not less than 250 words, along with keywords. The main body comprises an introduction, body paragraphs addressing each point from the abstract with citations, and a conclusion restating the thesis and supporting arguments. The reference page, placed after the main body, lists all sources alphabetically with one-half inch indentation. Adhering to these guidelines ensures the creation of a well-structured and comprehensive nursing research paper. For further assistance contact us at williamsliason@outloock.com
The Pathophysiology and Therapeutic Intervention of Migraine

Introduction
Migraine, a prevalent neurological disorder characterized by recurrent headaches, sensory disturbances, and autonomic dysregulation, poses a significant global health burden. We are going to provide a comprehensive review citing out the unique pathophysiological mechanisms underlying migraine and discuss the evolving landscape of therapeutic interventions.
Understanding Migraine Pathophysiology

1. Genetic Predisposition
Migraine exhibits a strong familial aggregation, suggesting a genetic component in its etiology. Genome-wide association studies have identified numerous susceptibility loci implicated in migraine susceptibility, including genes involved in neuronal excitability, neurotransmitter release, and vascular regulation.
2.Environmental Factors
Environmental triggers such as stress, sleep disturbances, hormonal fluctuations, dietary factors, and sensory stimuli play a crucial role in migraine onset and exacerbation. These triggers interact with genetic predispositions to precipitate migraine attacks, underscoring the threshold nature of the disorder.
Sensory Processing Abnormalities
Migraine pathophysiology revolves around the concept of a cyclic sensory threshold model, wherein aberrant processing of sensory inputs leads to hypersensitivity and pain amplification. Dysregulation of cortical excitability, thalamocortical networks, and descending pain modulatory pathways contribute to the sensory manifestations of migraine.
Phases of Migraine

Migraine progression is characterized by distinct phases, including premonitory, aura, pain, and postdrome phase, each associated with specific neurophysiological changes. The premonitory phase, marked by various symptoms preceding the headache, reflects hypothalamic and brainstem activation. Aura, a transient neurological phenomenon, involves cortical spreading depression and cortical spreading depolarization, leading to visual, sensory, or motor disturbances. The pain phase, mediated by trigeminal vascular activation and central sensitization, culminates into headache and associated symptoms. The postdrome phase, characterized by residual symptoms following headache resolution, implicates persistent alterations in cortical and brainstem function.
a) Trigeminal vascular System

Central to migraine pathophysiology is the trigeminal vascular system, comprising peripheral trigeminal afferents and central brain nuclei involved in pain processing. Activation of trigeminal vascular pathways, mediated by neuropeptides like Calcitonin gene-related peptide, substance P, and neurokinin A, initiates neurogenic inflammation and sensitization of meningeal nociceptors, contributing to headache generation.
b) Brainstem Nuclei
Brainstem regions, including the dorsolateral pons, periaqueductal gray, and locus coeruleus, serve as crucial modulators of trigeminal vascular transmission. Dysregulation of brainstem nuclei leads to unbearable pain processing and autonomic dysfunction, characteristic of migraine attacks.
c) Hypothalamic Involvement
The hypothalamus plays an important role in migraine initiation and progression, integrating nociceptive, autonomic, and circadian inputs. Dysregulation of hypothalamic neurotransmitters, including orexin, serotonin, and dopamine, contributes to migraine susceptibility and triggers stress-induced attacks.
d) Thalamic Dysfunction
The thalamus, a key relay station in sensory processing, exhibits structural and functional abnormalities in migraine. Altered thalamocortical connectivity, thalamic excitability, and neurotransmitter imbalance contribute to central sensitization, photophobia, and allodynia, hallmark features of migraine.
e) Cortical Alterations
Beyond aura generation, the cerebral cortex demonstrates widespread abnormalities in migraineurs, including changes in cortical thickness, gray matter volume, and functional connectivity. Genetic variants associated with glutamatergic neurotransmission and cortical excitability further implicate cortical dysfunction in migraine pathophysiology.
Therapeutic Approaches

a) Acute Treatments
Triptans, serotonin receptor agonists, have long been the mainstay of acute migraine therapy. However, emerging classes of medications, including ditans and gepants, offer alternative treatment options with improved tolerability and efficacy. Lasmiditan, a selective 5-HT1F receptor agonist, provides rapid relief without vasoconstrictive effects, making it suitable for patients with contraindications to triptans. Gepants, small-molecule CGRP receptor antagonists, block CGRP-mediated vasodilation and neurogenic inflammation, offering effective pain relief without cardiovascular risks.
b) Preventive Treatments
Monoclonal antibodies targeting CGRP or its receptors represent a breakthrough in migraine prevention, providing sustained efficacy with monthly or quarterly dosing regimens. Erenumab, fremanezumab, and galcanezumab have demonstrated superior efficacy compared to placebo in reducing migraine frequency and severity, with favorable safety profiles. Gepants such as atogepant and Rimegepant offer additional options for migraine prophylaxis, particularly in patients intolerant to traditional preventive therapies.
c) Neuromodulation Techniques
Non-invasive neuromodulation modalities, including transcranial magnetic stimulation and transcutaneous supraorbital nerve stimulation, offer adjunctive therapeutic options for acute migraine management. TMS delivers magnetic pulses to cortical regions implicated in migraine pathophysiology, modulating cortical excitability and pain perception. tSNS targets the supraorbital nerve, inhibiting nociceptive transmission and providing rapid pain relief without systemic side effects. Additionally, vagus nerve stimulation (VNS) offers a promising approach for both acute and preventive migraine treatment, modulating autonomic function and central pain processing.
Conclusion
In conclusion, migraine represents a complex neurological disorder with a diverse clinical manifestations. Advances in our understanding of migraine pathophysiology have paved the way for the development of novel therapeutic agents targeting key molecular and neural pathways. By understanding the interplay between genetic predisposition, sensory processing abnormalities, and central pain modulation, clinicians can tailor treatment strategies to individual patient needs, optimizing therapeutic outcomes and improving quality of life for migraine patients worldwide. Continued research efforts and clinical innovations hold the promise of further advancements in migraine management, underscoring the collective commitment to alleviating the global burden of this devastating condition.
Understanding the pathophysiology of migraine is crucial for effective management, and this comprehensive analysis sheds light on the complex mechanisms underlying this neurological disorder. For medical students facing challenges in studying migraine or any other medical topic, seeking professional help from Expert Academic Assignment Help can provide valuable guidance and support. With our expert assistance, students can overcome obstacles and excel in their academic endeavors. Contact us at expertassignment46@gmail.com to elevate your understanding and mastery of medical concepts.
Human musculoskeletal system.

Human musculoskeletal system, often referred to as the locomotor system, is a complex and integral component of human anatomy, enabling movement and providing structural support to the body. Comprising bones, muscles, cartilage, tendons, ligaments, and other connective tissues, this intricate system plays a crucial role in maintaining form, stability, and mobility. This comprehensive article aims to explore the various components and functions of the musculoskeletal system, addressing the nuanced interplay between bones, muscles, and joints. Additionally, it delves into the classification of bones, the functions of the skeletal system, the role of muscles in movement, and the clinical significance of this system. Understanding the musculoskeletal system is fundamental to appreciating its profound significance in human anatomy and physiology.
The Skeletal System:
At the core of the musculoskeletal system lies the skeletal framework, serving as the foundation for the attachment of tissues and organs. This section provides an in-depth exploration of the skeletal system, elucidating its dynamic structure, classifications of bones, and the critical functions they perform. From supporting the body’s shape to acting as a storage site for essential minerals such as calcium and phosphorus, bones play a multifaceted role. The controversies surrounding the number of bones in the human skeleton are addressed, emphasizing the dynamic nature of the skeletal system, which evolves from birth to maturity.
2.The Muscular System:
The musculoskeletal system’s functionality is inherently intertwined with the muscular system, comprising skeletal, smooth, and cardiac muscles. This section delves into the characteristics and roles of each muscle type, with a particular focus on the conscious control exerted by skeletal muscles. A comprehensive exploration of muscle contraction processes, initiation mechanisms, and the role of tendons in transmitting forces during contractions enriches our understanding of the system’s biomechanics. Recognizing the distinct attributes of cardiac and smooth muscles contributes to a holistic grasp of the musculoskeletal system’s dynamic nature.
3.Joints, Ligaments, and Bursae:
Movement within the musculoskeletal system is facilitated by joints, which connect bones and allow for a diverse range of motions. This section categorizes joints into diarthroses, amphiarthrosis, and synarthroses, elucidating their specific functions. A detailed examination of synovial joints, lubricated by synovial fluid, and the role of ligaments in limiting dislocation and controlling movement enhances our comprehension of joint dynamics. The significance of bursae, fluid-filled sacs providing cushioning around joints, is explored, emphasizing their role in minimizing friction and supporting efficient movement.
Clinical Significance:
The musculoskeletal system’s clinical significance extends to its susceptibility to disorders, impacting overall health. Diseases affecting this system can manifest as functional disorders, motion discrepancies, or complications arising from disorders in other body systems. This section explores the intricacies of musculoskeletal disorders, acknowledging the interconnections with the vascular, nervous, and integumentary systems that contribute to diagnostic challenges. Articular disorders are prevalent, but the musculoskeletal system is also affected by muscular diseases, neurologic deficits, toxins, endocrine abnormalities, metabolic disorders, infectious diseases, blood and vascular disorders, and nutritional imbalances. An exploration of inpatient procedures involving musculoskeletal interventions underscores the clinical importance of this system.
Conclusion:
In conclusion, the human musculoskeletal system stands as a marvel of biological engineering, orchestrating movement, providing support, and safeguarding vital organs. This comprehensive exploration, spanning bones, muscles, joints, and clinical significance, highlights the intricate interplay of various components that contribute to the system’s overall functionality. Despite the challenges posed by disorders and diseases, advancements in medical science, particularly in fields like rheumatology and orthopedic surgery, continue to enhance our understanding and treatment of musculoskeletal issues. Recognizing the complexity and clinical significance of this system is crucial for healthcare professionals in providing comprehensive care. As we delve deeper into the intricacies of the human body, the musculoskeletal system stands as a testament to the harmonious coordination of various components for the fundamental purpose of movement and stability. This expansive exploration serves as a valuable resource for those seeking a profound understanding of the human musculoskeletal system.
For Health Sciences Assignment Help,
email us on, williamsliason@outlook.com
-
 prollymaia liked this · 8 months ago
prollymaia liked this · 8 months ago -
 expertacademicassignmenthelp reblogged this · 1 year ago
expertacademicassignmenthelp reblogged this · 1 year ago -
 expertacademicassignmenthelp reblogged this · 1 year ago
expertacademicassignmenthelp reblogged this · 1 year ago -
 kitteena reblogged this · 1 year ago
kitteena reblogged this · 1 year ago -
 kitteena liked this · 1 year ago
kitteena liked this · 1 year ago -
 expertacademicassignmenthelp reblogged this · 1 year ago
expertacademicassignmenthelp reblogged this · 1 year ago