How Does The Drug Got Excreted / Eliminated From The Body?
How Does The Drug Got Excreted / Eliminated From The Body?

Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: expertassignment46@gmail.com
Your excellence our pride.
More Posts from Expertacademicassignmenthelp and Others
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
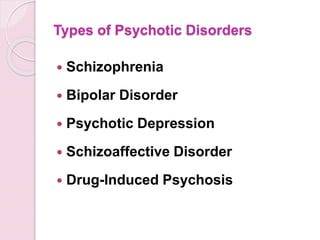
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
Osteoporosis in Aging

Introduction
Osteoporosis, a progressive skeletal disorder characterized by reduced bone mass and deteriorating bone quality, poses significant health challenges, especially among the aging population. This discussion involves dynamics of bone health, the factors contributing to osteoporosis, and proactive measures individuals can adopt to protect and strengthen their bones as they age.
1.Understanding Bone Structure and Dynamics
Bones, seemingly solid, have an internal honeycomb-like structure. This structural framework undergoes constant remodeling, with cells building new bone tissue while others dissolve existing bone to release essential minerals. As individuals age, this delicate balance shifts, resulting in a gradual loss of bone density and an increased susceptibility to fractures.
2.Prevalence and Impact of Osteoporosis
Osteoporosis is a widespread concern, affecting over 10 million people nationwide. Its consequences, particularly in Adults, extend beyond fractures, leading to a variety of issues such as disability and loss of dependence. The vulnerability of specific areas, including the;
hips, wrists, and spine, underscores the importance of understanding and addressing this condition.
3.Hormonal Influence and Screening
Estrogen, a crucial hormone, plays a major role in bone formation and regeneration. Postmenopausal women, experiencing a decline in estrogen levels, face a high risk of an increased bone loss. Regular screening, typically recommended for women aged 65 and older, involves non-invasive tests like;
Bone density scan(DXA), measuring bone mineral density. A total score of -2.5 or lower is indicative of osteoporosis.
4.Nutritional Factors
The role of nutrition in maintaining bone health cannot be overstated. Calcium, an essential mineral for bone strength and formation, is obtainable from various dietary sources such as, dairy products and leafy greens. Vitamin D, facilitating calcium absorption, becomes increasingly critical with age. This emphasizes the importance of adequate nutrient intake, either through dietary means or supplements. Specific daily calcium requirements for women over 50 and men over 70 are outlined.
5.Exercise as a Protective Measure
Physical activity, especially weight-bearing exercises like jogging, walking, tennis, and dancing, significantly contributes to bone health. These exercises serve as signals to bone cells, promoting density and reducing the risk of fractures. Conversely, lifestyle choices such as smoking and heavy drinking weaken bones, while certain medications may increase the risk of osteoporosis.
Medical Interventions and Future Prospects
Medical interventions, including medications like bisphosphonates, are commonly prescribed to combat bone loss. Ongoing research is exploring drugs aimed at stimulating bone growth, with parathyroid hormone being a current option. The article discusses the potential of these interventions and highlights the importance of timely medical advice and interventions, even after an osteoporosis diagnosis, to positively impact bone health.
Fall Prevention and Fracture Avoidance
More than 2 million fragility fractures occur annually due to falls, highlighting the need for a comprehensive approach to bone health. Combining efforts to enhance bone strength with fall prevention strategies is crucial. Factors such as balance, environmental hazards, and the type of fall play significant roles in fracture risk. The discussion underscores the effectiveness of exercises that improve balance and coordination, such as slow intentional movement in preventing fractures.
Conclusion
Maintaining optimal bone health is a course that involves a combination of nutrition, exercise, and proactive healthcare measures. Given the critical impact of osteoporosis on aging populations, raising awareness and implementing early intervention strategies are paramount. This comprehensive approach empowers individuals to foresee the risks associated with osteoporosis, ensuring a resilient and active lifestyle in their later years. The discussion concludes by encouraging individuals concerned about their bone health to engage or consult with their healthcare specialists, pressing on the importance of personalized guidance and bone density testing for proactive management.
For Health Sciences Assignment Help;
Email us at;
williamsliason@outlook.com
Medical ethics

Medical ethics is a complex field that intersects with various aspects of
1.Medicine
2. Ethics
3.Philosophy and
5.Society
The study of medical ethics involves the exploration of moral values and judgments as they pertain to the practice of medicine. This interdisciplinary field delves into the practical application of ethical principles in clinical settings and encompasses a broader understanding of its history, philosophy, theology, and sociology.
Historical Evolution:
The roots of Western medical ethics can be traced back to ancient guidelines, including the famous Hippocratic Oath. In the medieval and early modern period, contributions from Muslim physicians like Ishaq bin Ali Rahawi and figures such as Maimonides and Thomas Aquinas shaped ethical discourse. The emergence of a self-conscious discourse around medical ethics gained momentum in the 18th and 19th centuries, with notable figures like Thomas Percival contributing to the ethical framework. In 1847, the American Medical Association adopted its first code of ethics, rooted in Percival’s work.
Core Values in Medical Ethics:
Six fundamental values commonly applied in medical ethics discussions are:
1.Autonomy
Emphasizes a patient’s right to refuse or choose their treatment, rooted in the principle of self-determination.
2.Beneficence
Advocates for practitioners to act in the best interest of the patient, prioritizing their well-being.
3.Non-maleficence
Encompasses the principle of “first, do no harm,” emphasizing the importance of avoiding harm to the patient.
4.Justice
Focuses on the fair distribution of scarce health resources and the ethical decision-making process concerning who receives what treatment.
5.Dignity
Recognizes the right to dignity for both the patient and the healthcare provider.
6.Truthfulness and Honesty
Stresses the significance of informed consent, gaining prominence after historical events like the Nuremberg trials and Tuskegee Syphilis Study.
Ethical Dilemmas and Resolutions:
Ethical conflicts often arise when these values are in conflict, leading to dilemmas that require careful consideration. For instance, conflicts between autonomy and beneficence/non-maleficence can occur when patients disagree with recommended treatments. Euthanasia presents a poignant example where autonomy clashes with the principle of preserving life.
Informed Consent and Confidentiality:
Informed consent is a critical aspect of medical ethics, ensuring that individuals are fully informed about the potential benefits and risks of their chosen treatment. Confidentiality, including patient-physician privilege, is a cornerstone, with legal protections in place.
Criticisms and Cultural Considerations:
Medical ethics faces criticisms, including bias in a framework where individuals may not be free to contract for medical treatment. The balance between beneficence and autonomy is debated, with considerations about state or supplier group interests over patient welfare.
Cultural differences can complicate medical ethics, as diverse beliefs about disease origins and treatment may conflict with Western medicine. Practices like truth-telling vary among cultures, impacting the doctor-patient relationship.
Conflicts of Interest and Online Practices:
Physicians must navigate conflicts of interest to ensure unbiased medical judgment. Online business practices have introduced challenges, with concerns about the influence of pharmaceutical companies and the commodification of medical diagnoses.
Importance of Communication:
Open lines of communication are crucial in resolving ethical conflicts. Communication breakdowns among patients, healthcare teams, family members, and the medical community can lead to disagreements. Remedying these breakdowns is essential for ethical problem-solving.
Control and Resolution Mechanisms:
Hospital accreditation emphasizes ethical considerations, including physician integrity, conflicts of interest, research ethics, and organ transplantation ethics. Ethical guidelines, such as the Declaration of Helsinki, provide a framework, and ethics committees play a role in deciding complex matters.
Future Challenges and Developments:
As medical ethics continues to evolve, ongoing challenges include addressing cultural differences, advancing communication practices, and adapting to the changing landscape of healthcare, including the role of technology and online platforms.
In conclusion, medical ethics is a dynamic and multifaceted field that constantly grapples with the evolving landscape of medicine and society. Its principles serve as a compass for healthcare professionals, ensuring ethical decision-making and the promotion of patient welfare. The field’s rich history, diverse values, and ongoing challenges contribute to its significance in shaping the ethical dimensions of medical practice.
For Health Sciences Assignment Help;
Email Us At;
williamsliason@outlook.com
What is The Process Of Sleep?

Introduction
Sleep is a complex physiological process that encompasses more than merely closing one’s eyes and drifting into unconsciousness. It is an active state of unconsciousness in which the brain, while relatively at rest, remains responsive primarily to internal stimuli. Despite extensive research, the precise purpose of sleep remains incompletely understood. Several prominent theories attempt to elaborate the purpose of sleep, including the Inactivity Theory, Energy Conservation Theory, Restoration Theory, and Brain Plasticity Theory.
Inactivity Theory involves that inactivity during nighttime reduces the risk of predation, offering an evolutionary advantage. This theory suggests that creatures that remained inactive during the night were less likely to fall victim to predators, thereby enhancing survival and reproductive success.
Energy Conservation Theory proposes that the primary function of sleep is to decrease energy demand during periods when it is less efficient to procure food, supported by evidence of a 10% reduction in metabolism during sleep. This theory aligns with the observation that many species exhibit lower metabolic rates during sleep, thereby conserving energy.
Restorative Theory asserts that sleep facilitates the repair and replenishment of cellular components, as evidenced by processes such as muscle repair, tissue growth, protein synthesis, and hormone release occurring predominantly during sleep. This theory is supported by findings that various restorative functions are activated during sleep, promoting physical health and well-being.
Brain Plasticity Theory suggests that sleep is essential for neural reorganization and brain development, particularly in infants and children who require extensive sleep. This theory underscores the role of sleep in cognitive functions, learning, and memory consolidation.
These theories collectively indicate that sleep serves multiple functions, and a combination of these concepts likely explains the necessity of sleep.
Function

Sleep follows a cyclical pattern, alternating between two major phases: Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep. NREM sleep is subdivided into stages 1 through 3, each representing different depths of sleep characterized by unique brain wave patterns, muscle tone, and eye movement patterns. NREM sleep comprises approximately 75–80% of total sleep time, while REM sleep accounts for the remaining 20–25%.
The sleep cycle begins with a short NREM stage 1 phase, progresses through NREM stages 2 and 3, and culminates in REM sleep. This cycle repeats throughout the night, with initial cycles lasting 70–100 minutes and subsequent cycles 90–120 minutes. As the night progresses, the duration of REM sleep increases, eventually comprising up to 30% of the sleep cycle later in the night. Typically, an individual undergoes 4 to 5 sleep cycles per night.
NREM Stage 1: A shallow sleep stage lasting 1–7 minutes, characterized by rhythmical alpha waves (8–13 Hz). This stage represents the transition from wakefulness to sleep, during which the individual can be easily awakened.
NREM Stage 2: A deeper sleep state lasting 10–25 minutes initially, progressing to encompass 50% of the total sleep cycle. EEG recordings during this stage show sleep spindles and K-complexes. Memory consolidation is believed to occur primarily in this stage.
NREM Stage 3: Lasting 20–40 minutes initially, characterized by high-voltage, slow-wave frequency on EEG. This stage, also known as slow-wave sleep (SWS), is crucial for restorative processes.
REM Sleep: Responsible for dreaming, characterized by muscle paralysis (except for the extraocular muscles) and sawtooth waveforms on EEG. REM sleep involves increased brain activity and is essential for cognitive functions such as learning, memory consolidation, and emotional regulation.
Mechanism

The regulation of sleep involves a delicate balance between homeostatic processes and circadian rhythms.
a) Homeostatic Processes
These processes reflect the body’s need for sleep, increasing the pressure to sleep the longer one stays awake. Sleep generation is initiated within the ventrolateral preoptic nucleus (VLPO) of the anterior hypothalamus, which inhibits arousal regions in the brain, including the tuberomammillary nucleus, lateral hypothalamus, locus coeruleus, dorsal raphe, laterodorsally segmental nucleus. Hypocretin (orexin) neurons in the lateral hypothalamus facilitate this process synergistically.
b) Circadian Rhythm
The circadian rhythm, or the internal body clock, regulates the sleep-wake cycle and is influenced by light levels detected by the retina. The hypothalamus, particularly the suprachiasmatic nucleus (SCN),initiates this rhythm. Melatonin, produced by the pineal gland, modulates the circadian rhythm, with levels peaking at night and decreasing during the day. The circadian rhythm typically spans approximately 24.2 hours, and variations in body temperature also play a role, with lower temperatures in the morning and higher temperatures in the evening.
NREM sleep involves a functional disconnection between the brain stem, thalamus, and cortex, maintained by hyperpolarizing GABA neurons. During this phase, corticothalamic neurons signal the thalamus, causing hyperpolarization of thalamic reticular neurons, resulting in delta waves from both thalamic reticular and cortical pyramidal sources.
REM sleep is generated by “REM-on neurons” in the mesencephalic and pontine cholinergic neurons. The pedunculopontine tegmental nucleus and lateral dorsal tegmental neurons trigger desynchronized cortical waveforms. The tonic component of REM sleep is parasympathetically mediated, while the phasic component is sympathetically mediated.
Related Testing
Polysomnography is the primary modality used to study sleep. It is a comprehensive test that includes an electrocardiogram (ECG), electroencephalography (EEG), electrooculography (EOG), electromyography (EMG), and oxygen saturation monitoring.
ECG: Measures the electrical activity of the heart to detect cardiac anomalies such as arrhythmias.
EEG: Non-invasively records brain wave activity to determine sleep stages and detect neurological abnormalities.
EOG: Measures eye movements to differentiate between NREM and REM sleep.
EMG: Assesses muscle activity, particularly in the respiratory muscles and peripheral limbs, to detect excessive movement or muscle tension during sleep.
Oxygen Saturation: Monitors respiratory function to ensure adequate oxygenation during sleep.
Clinical Significance

a) .Insomnia
Insomnia is characterized by difficulty falling or staying asleep and is the most common sleep disorder. It is often related to psychological stressors, poor sleep environments, irregular sleep schedules, or excessive mental, physical, or chemical stimulation. Treatment typically involves cognitive-behavioral therapy (CBT), sleep hygiene practices, and, in some cases, pharmacological interventions.
b) .Obstructive Sleep Apnea (OSA)
OSA is marked by repeated pauses in breathing during sleep due to airway obstruction, often caused by obesity or weak pharyngeal muscles. This condition leads to hypoxia and frequent awakenings, preventing restful sleep. OSA is classified into mild, moderate, and severe based on the frequency of apneic episodes per hour. Treatment options include Continuous Positive Airway Pressure (CPAP) therapy, Bilevel Positive Airway Pressure (BiPAP) therapy, mandibular advancement devices, and surgical interventions such as uvulopalatopharyngoplasty, adenotonsillectomy, and maxillomandibular advancement.
c) .Central Sleep Apnea
Central Sleep Apnea (CSA) results from a failure in the central respiratory drive, leading to diminished breathing effort during sleep. Conditions such as congenital central hypoventilation syndrome (Ondine’s curse) or congestive heart failure can cause CSA. Treatment includes CPAP, BiPAP, Adaptive-servo-ventilation, and medications like acetazolamide or theophylline.
d) .Mixed Sleep Apnea
Mixed Sleep Apnea, also known as Complex Sleep Apnea, involves symptoms of both OSA and CSA. This condition typically manifests when patients with OSA develop CSA symptoms upon treatment with CPAP. Treatment often involves low-pressure CPAP therapy.
d) .Ghrelin-Leptin Abnormalities
Sleep duration significantly influences hunger-regulating hormones, with reduced sleep linked to lower levels of leptin and higher levels of ghrelin. Leptin, produced by adipose cells, inhibits hunger, while ghrelin, produced in the gastrointestinal tract, stimulates appetite. Imbalances in these hormones due to inadequate sleep can increase appetite and contribute to higher body mass index (BMI), potentially leading to obesity. This phenomenon is particularly relevant in patients with OSA, where increased BMI is a risk factor.
e) .Narcolepsy
Narcolepsy is characterized by a loss of orexin (hypocretin) neurons, leading to unstable transitions between sleep and wakefulness. Symptoms include excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations. Narcolepsy type 1 involves a significant loss of orexin neurons, while type 2 is less severe. Treatment focuses on managing symptoms with medications such as stimulants, sodium oxybate, and selective serotonin and norepinephrine reuptake inhibitors (SSRIs and SNRIs), along with lifestyle modifications.
f) .Somnambulism (Sleepwalking)
Somnambulism, or sleepwalking, involves performing activities while in a state of combined sleep and wakefulness. Sleepwalking is associated with increased slow-wave sleep and sleep deprivation, and there is evidence of a genetic predisposition. Treatment includes ensuring a safe sleep environment, improving sleep hygiene, and, in some cases, pharmacological interventions such as benzodiazepines.
Conclusion
Sleep is a physiological process essential for various bodily functions, including energy conservation, cellular repair, brain development, and cognitive function. The precise mechanisms and purposes of sleep remain areas of active research. Understanding the complexities of sleep and its disorders is crucial for promoting overall health and addressing various medical conditions. Ongoing research aims to fully understand the mechanisms of sleep and its broad implications for human health..
Navigating the rigorous demands of medical studies requires support and collaboration. Whether you’re a nursing student, medical doctor, clinical student, pharmacist, or any other medical practitioner, don’t hesitate to seek assistance. Utilize available resources and value teamwork and mentorship.
For personalized support, expert advice, and comprehensive resources, contact Expert Academic Assignment Help at expertassignment46@gmail.com With the right support and dedication, you can achieve your goals and make significant contributions to healthcare.
Study Tips For University Students

Introduction
Achieving success as a university student involves mastering effective study methods, time management, and maintaining overall well-being. In this comprehensive discussion, we will major into the top 10 university study tips that can prepare students for the challenges and opportunities that university life presents.
Preview and Review Study Resources
Understanding the importance of previewing study materials before lectures.
Incorporating regular reviews to consolidate knowledge and prepare for new concepts.
Exploring advanced reading techniques for improved comprehension.
2. Customizing Your Note-Taking System
Recognizing the power of note-taking in mastering any subject.
Exploring digital and handwritten note-taking approaches.
Utilizing advanced note-taking apps for organization and efficiency.
Discussing the Cornell Method, mind mapping, and other note-taking strategies.

. Establishing a daily study routine for consistency.
Adapting study habits during holidays to balance academics and festivities.
Creating to-do lists and prioritizing tasks for optimal time management.
Examining time-blocking techniques for enhanced productivity.
4. Setting Goals and Focusing
Setting specific, realistic goals to enhance study sessions.
Avoiding multitasking and using goal-oriented apps for focus.
Exploring the concept of SMART goals in academic settings.

Recognizing the importance of breaks for maintaining attention levels.
Introducing the Pomodoro Technique for efficient study sessions.
Discussing mindfulness and relaxation techniques during breaks.
6. Creating a Suitable Studying Environment
Maximizing productivity by minimizing distractions.
Establishing environmental cues to signal study mode.
Exploring the impact of ergonomics on study efficiency.

Motivating regular study habits by incorporating rewards.
Breaking down tasks into smaller goals for increased control.
Exploring the psychology of rewards and their impact on motivation.
8. Utilizing Study Groups
. Exploring the benefits of studying in groups.
Ensuring structured and accountable study group dynamics.
Discussing effective group communication and collaboration.
9 .Seeking Help When Needed
Overcoming the reluctance to ask for help.
Recognizing the importance of seeking assistance for academic success.
Discussing the role of tutors, mentors, and academic resources.

Understanding the impact of sleep and exercise on academic performance.
Incorporating a consistent sleep schedule and daily exercise routine.
Discussing the link between physical well-being and cognitive function.
Conclusion
In conclusion, success in university requires a holistic approach that encompasses effective study techniques, time management, and self-care. By implementing these ten study tips and delving into related topics, students can not only excel academically but also enhance their overall university experience. Balancing academic commitments with a healthy lifestyle is crucial for long-term success, and these strategies provide a foundation for thriving in the challenging yet rewarding university environment.
We wish you all the best in your University study program.
Incase of any challenges or need assistance and guidance during the process, do not hesitate ,just;
Email us at; williamsassignmenthelpfredrick@gmail.com
Nursing Essay

Introduction
Nursing, widely regarded as a challenging academic discipline, demands not only practical skills but also a profound ability to articulate one’s understanding through essays. Despite its predominantly practical nature, nursing essays serve as a critical medium for students to demonstrate their theoretical comprehension of nursing practice. This comprehensive guide aims to provide detailed recommendations, spanning from the methods of choosing a suitable topic to crafting a meticulously structured essay. By adhering to the guidance provided herein, nursing students can significantly enhance their writing skills, expand their knowledge base, and gain invaluable practical experience.
1. The Importance of Nursing

a. Understanding the Role of Nursing Essays
Nursing essays play a major role in assessing a student’s grasp of theoretical aspects of nursing practice. This section delves into the significance of essays in demonstrating clarity of thought, the ability to express arguments, and the implications for academic success.
b. The Link Between Writing Skills and Academic Achievement
Examining how proficient writing contributes to academic success, this subsection explores how essays serve as a direct reflection of a student’s ability to articulate complex ideas and arguments in a coherent manner.
2. Choosing a Suitable Topic

a. The Complexity of Nursing Practice
An in-depth analysis of the broad nature of nursing practice, discussing its various dimensions, functions, and roles. Understanding the complexity of the field is crucial in selecting an engaging and relevant essay topic.
b. Criteria for Choosing a Nursing Essay Topic
This subsection introduces specific criteria for selecting an appropriate essay topic. Emphasizing critical thinking, open-mindedness, and cultural competence, it provides practical advice on avoiding personal biases and ensuring a broad perspective.
c. Examples of Engaging Nursing Essay Topics
Offering a range of potential topics, this section provides concrete examples to inspire nursing students. Topics such as “Cultural Sensitivity in the Context of Advanced Nursing Practice” and “The Role of Informed Consent in Quantitative Research” are explored
3. Evaluating Evidence

a. The Importance of Evidence in Nursing Essays
An exploration of the main role evidence plays in substantiating arguments in nursing essays. This section emphasizes the need for practice-based evidence and the importance of critical evaluation.
b. Distinguishing Types of Evidence
A comprehensive breakdown of different types of evidence, including research-based and experiential evidence. Understanding these distinctions is essential in choosing evidence that aligns with the essay’s objectives.
c. Evaluating the Merits of Evidence
Indulging into the process of evaluating evidence, this subsection discusses the criteria for assessing the authority, reliability, and validity of research designs. Practical tips on making informed judgments about evidence are provided.
Section 4: Understanding Types of Evidence
4. Categorizing Evidence in Nursing Essay

Examining the different types of evidence used in nursing essays and their specific roles. A detailed discussion on how various research designs impact the nature and relevance of evidence.
a. The Significance of Experiential Evidence
Highlighting the importance of experiential evidence in nursing essays, particularly in the analysis of case studies and risk management. Practical insights into incorporating experiential evidence effectively.
b. The Reliability of Research-Based Evidence
Exploring the reliability of evidence derived from research, with an emphasis on the meticulous design of studies to ensure objectivity and validity. A critical discussion on the role of authentic data in supporting claims.
5.The Ultimate Structure of a Nursing Essay

a. Setting the Stage
A comprehensive exploration of the introduction’s role in capturing the reader’s attention, presenting the essay topic, and establishing the rationale for the paper. Practical advice on incorporating hooks, such as questions, statistical data, or quotes, is provided.
b. Crafting a Powerful Thesis Statement
An in-depth examination of the thesis statement, exploring its role as the linchpin of the essay. Examples of strong thesis statements are dissected to illustrate effective positioning and claim formulation.
c. The Main Body: Developing Coherent Arguments
A thorough analysis of the main body’s structure, emphasizing the importance of organizing ideas into clear paragraphs. Practical guidelines on presenting topic sentences, evidence, discussions, and concluding statements are provided.
d. Conclusion: Reinforcing Key Points
A detailed discussion on the conclusion’s role in summarizing key arguments, restating the thesis, and offering recommendations. Practical insights on framing a compelling conclusion that reinforces the essay’s significance.
e. Proofreading and Editing Tips
6. The Importance of Proofreading in Nursing Essays

A critical examination of the proofreading process, highlighting its significance in identifying and rectifying common mistakes. Practical insights into maintaining a scholarly tone and avoiding first-person expression
a. Avoiding Plagiarism Through Proper Citation
An exploration of the importance of proper citation to prevent plagiarism. Guidelines on citing information that is not common knowledge, ensuring academic integrity in nursing essa
b. Evaluating Readability and Coherence
Practical tips on assessing the overall readability and coherence of a nursing essay. Guidance on examining figures, tables, and graphs to enhance visual appeal and effectiveness.
d. Ensuring Consistency in Writing
An exploration of the need for consistency in nursing essays. Practical advice on evaluating the consistency of arguments, statements, and overall presentation
7.Recapitulation of the key points

A concise recapitulation of the key points discussed throughout the guide, reinforcing the critical elements of successful nursing essay writing.
a. Empowering Nursing Students Through Effective Writing
A concluding reflection on how mastering the art of nursing essay writing empowers students to excel academically, contribute meaningfully to the field, and become articulate advocates for healthcare.
Conclusion:
Mastering the art of nursing essay writing is a multifaceted journey that demands a nuanced understanding of the discipline, from choosing a relevant topic to evaluating evidence and crafting a well-structured essay. This comprehensive guide serves as a roadmap for nursing students, providing them with the tools and insights necessary to navigate the complexities of academic writing successfully. By following the detailed recommendations outlined herein, aspiring nurses can not only fulfill the requirements of their coursework but also make substantial contributions to the field through articulate and well-supported essays.
Wishing you all the best in Writing Nursing Essays.
Incase of any Enquiries, Guidance or Challenges faced during the process;
Email us at;
williamsassignmenthelpfredrick@gmail.com
10 Common Dental Problems

Introduction
Maintaining optimal dental health is crucial not only for a winning smile but also for overall well-being. However, numerous individuals encounter common dental issues that can affect their quality of life. From tooth decay to gum disease, understanding these problems and their treatments is essential for preventing complications and preserving oral health. This comprehensive guide explores ten prevalent dental problems and outlines effective treatment options for each, empowering individuals to make informed decisions about their dental care.
1.Tooth Decay

Tooth decay, also known as dental caries, is a pervasive dental issue caused by the accumulation of plaque and the subsequent erosion of tooth enamel. This section delves into the causes, symptoms, and treatment options for tooth decay, emphasizing the importance of preventive measures such as regular brushing, flossing, and dental check-ups.
2. Gum Disease

Gingivitis and periodontitis are two stages of gum disease characterized by inflammation and bacterial infection of the gums. Exploring the risk factors, symptoms, and management strategies for gum disease sheds light on the importance of proper oral hygiene practices and professional dental interventions in preserving gum health.
3.Bad Breath

Halitosis, or bad breath, can stem from various underlying factors such as poor oral hygiene, dry mouth, and underlying medical conditions. This segment examines the causes of bad breath and highlights the significance of comprehensive dental assessments and tailored treatment plans to address this common concern effectively.
4.Sensitive Teeth

Tooth sensitivity, characterized by discomfort in response to hot, cold, or sweet stimuli, often results from enamel erosion or underlying dental issues. Delving into the potential causes and management options for sensitive teeth underscores the role of personalized dental care in alleviating discomfort and enhancing oral comfort.
5.Cracked or Broken Teeth

Cracks or fractures in teeth can result from trauma, bruxism (teeth grinding), or other factors, leading to pain and functional impairment. This section explores the diagnostic procedures and treatment modalities available for repairing cracked or broken teeth, emphasizing the importance of prompt intervention to prevent further damage.
6.Receding Gums

Receding gums, characterized by the exposure of tooth roots due to gum tissue loss, can result from various factors, including poor oral hygiene and genetic predispositions. Analyzing the causes, consequences, and treatment approaches for receding gums underscores the significance of preventive measures and professional interventions in preserving gum health.
7. Root Infection

Root infections, often resulting from untreated cavities or trauma, can lead to severe pain and dental abscesses if left untreated. This segment elucidates the diagnostic techniques and treatment options for root infections, highlighting the role of root canal therapy in alleviating symptoms and preserving tooth structure.
8. Enamel Erosion

Enamel erosion, characterized by the gradual loss of tooth enamel due to acidic and sugary dietary habits, poses significant challenges to dental health. Exploring preventive strategies and restorative treatments for enamel erosion underscores the importance of dietary modifications and proactive dental care in preserving tooth structure and function.
9. Dry Mouth

Xerostomia, or dry mouth, can result from various factors, including medication side effects and underlying medical conditions. This section examines the causes, symptoms, and management strategies for dry mouth, emphasizing the importance of hydration and lifestyle modifications in alleviating discomfort and preventing oral complications.
10. Teeth Grinding
Bruxism, characterized by involuntary teeth grinding or clenching, can lead to tooth wear, jaw pain, and headaches. Exploring the underlying causes and treatment options for bruxism underscores the importance of stress management and protective dental appliances in mitigating symptoms and preserving dental health.
Conclusion
In conclusion, understanding and addressing common dental problems are essential steps toward maintaining optimal oral health and overall well-being. By recognizing the signs and symptoms of tooth decay, gum disease, and other dental issues, individuals can seek timely intervention and preventive care to mitigate risks and preserve their smiles. Through a combination of proper oral hygiene practices, regular dental check-ups, and personalized treatment plans, individuals can navigate common dental challenges with confidence and achieve lasting oral health. Embracing proactive dental care and seeking professional assistance when needed are crucial components of a comprehensive approach to dental wellness.
In exploring and pursuing your dental studies, we wish you all the best in becoming a dentist. In case you encounter challenges or need guidance during this study period, do not hesitate to contact us.
Email at;williamsassignmenthelpfredrick@gmail.com
ORGANS OF EXCRETION

Excretion, a fundamental process in living organisms, plays a critical role in maintaining internal equilibrium and ensuring the efficient removal of waste products. This detailed discussion will involve deeper into the importance of excretion, the organs involved, their functions, and their contributions to overall health and homeostasis.
Importance of Excretion
Excretion is essential for the survival of all living organisms, from single-celled organisms to complex multicellular organisms like humans. It involves the elimination of metabolic waste products, toxins, and excess substances that accumulate within the body. By removing these waste materials, excretion helps regulate the internal environment, ensuring optimal conditions for cellular function and metabolic processes. Without effective excretory mechanisms, the buildup of waste products would lead to toxicity, impaired physiological function, and ultimately, organismal death.
Organs of Excretion
The human body employs a variety of organs for excretion, each with its own specialized functions and mechanisms for waste elimination. These organs include the skin, liver, large intestine, lungs, and kidneys. While some organs primarily eliminate specific types of waste products, others have multifunctional roles in metabolism, digestion, and detoxification, in addition to excretion.
1. Skin
The skin, the body’s largest organ, serves as a multifunctional barrier between the internal and external environments. In addition to its protective role, the skin participates in excretion through the production of sweat by sweat glands located in the dermis. Sweat, composed of water, salts, and urea, is released through sweat pores onto the skin’s surface, where it evaporates and helps regulate body temperature. Sweating also facilitates the elimination of metabolic wastes, toxins, and excess salts from the body, contributing to overall homeostasis.
2. Liver

The liver, a vital organ located in the upper right abdomen, is involved in numerous metabolic processes, including digestion, detoxification, and the synthesis of essential molecules. As part of its excretory function, the liver processes and eliminates various waste products and toxins from the bloodstream. It metabolizes ammonia, a toxic byproduct of protein metabolism, into urea, a less toxic compound that is excreted by the kidneys in urine. Additionally, the liver excretes bilirubin, a waste product of heme metabolism, into bile, which is then eliminated from the body through the feces.
3. Large Intestine

The large intestine, the final segment of the gastrointestinal tract, plays a crucial role in the absorption of water and electrolytes from undigested food residues. In addition to its role in digestion and water reabsorption, the large intestine serves as a site for the accumulation and elimination of solid waste materials. Bile pigments, such as bilirubin, are excreted into the gastrointestinal tract via bile and eventually eliminated in feces, contributing to the characteristic color of stool.
4. Lungs

The lungs, the primary organs of respiration, also play a role in excretion by removing gaseous waste products, such as carbon dioxide, from the bloodstream. During the process of cellular respiration, carbon dioxide is produced as a byproduct and transported via the bloodstream to the lungs for elimination. Through the process of gas exchange in the alveoli, carbon dioxide is expelled from the body during exhalation, helping to regulate blood pH and maintain acid-base balance.
5. Kidneys

The kidneys are often regarded as the primary organs of excretion in the human body, responsible for filtering waste products and excess substances from the bloodstream and producing urine for elimination. Each kidney contains millions of functional units called nephrons, which play a crucial role in the filtration, reabsorption, and secretion of various substances. Nephrons filter blood to remove waste products, such as urea, creatinine, and uric acid, while reabsorbing essential nutrients and maintaining electrolyte balance. The resulting urine is then transported from the kidneys to the urinary bladder via the ureters and excreted from the body through the urethra during urination.
6. Urinary System

The kidneys, along with the ureters, urinary bladder, and urethra, collectively form the urinary system, which functions to transport, store, and eliminate urine from the body. The ureters carry urine from the kidneys to the urinary bladder, where it is stored until it is expelled from the body through the urethra. The urinary system plays a crucial role in maintaining fluid balance, electrolyte concentration, and pH regulation within the body, thereby supporting overall homeostasis and physiological function.
Conclusion
In conclusion, excretion is a vital process that enables living organisms to eliminate waste products and maintain internal balance. Through the coordinated efforts of various organs, including the skin, liver, large intestine, lungs, and kidneys, the body effectively removes metabolic wastes, toxins, and excess substances, thereby supporting overall health and homeostasis. Understanding the mechanisms of excretion and the roles of excretory organs is essential for appreciating the complexity of physiological regulation and the interconnection of bodily systems. By studying excretory processes, researchers and healthcare professionals can gain insights into disease mechanisms, develop therapeutic interventions, and promote optimal health and well-being.
For students seeking guidance and assistance with their academic assignments, Expert Academic Assignment Help stands out as an invaluable resource. With their unique and top-notch content, they offer solutions to various academic challenges, ranging from essays to research papers ,Clinical case studies and homework. Don’t hesitate to reach out to them for expert assistance and take your academic journey to the next level. For inquiries, contact expertassignment46@gmail.com
Diabetes

Introduction to Diabetes
Diabetes, a metabolic disorder characterized by chronic hyperglycemia, arises from abnormalities in insulin secretion, insulin action, or both. The condition’s prevalence has reached epidemic proportions globally, with significant health, economic, and social implications.
Types of Diabetes

Type 1 Diabetes: This autoimmune disease results from the destruction of pancreatic beta cells, leading to absolute insulin deficiency. Genetics and environmental triggers play pivotal roles in its pathogenesis. Despite being less common than Type 2 diabetes, its onset during childhood or adolescence significantly impacts individuals’ lives.
Type 2 Diabetes: Predominantly a disorder of insulin resistance, Type 2 diabetes accounts for the majority of diabetes cases worldwide. Lifestyle factors, genetic predisposition, and obesity contribute to its development. Its insidious onset often leads to delayed diagnosis and increased risk of complications.
Gestational Diabetes: Occurring during pregnancy, gestational diabetes poses risks to both maternal and fetal health. Hormonal changes and insulin resistance characterize its pathophysiology. Effective screening and management are crucial to prevent adverse outcomes.
Other Types of Diabetes: Variants like MODY, LADA, and secondary diabetes present unique challenges in diagnosis and management, requiring tailored approaches to care.
Epidemiology and Prevalence
Diabetes prevalence varies across demographics, with disparities observed in age, gender, ethnicity, and socioeconomic status. The escalating burden of diabetes underscores the urgent need for targeted prevention and management strategies.
Symptoms and Causes

Hyperglycemia-induced symptoms like polyuria, polydipsia, and unexplained weight loss serve as clinical indicators for diabetes diagnosis. Understanding the complex interplay of genetic, environmental, and lifestyle factors elucidates the condition’s etiology.
Complications
Diabetes complications encompass a spectrum of microvascular and macrovascular disorders, significantly impacting quality of life and life expectancy. From diabetic retinopathy to cardiovascular disease, nephropathy, neuropathy, and diabetic foot complications, the ripple effects of uncontrolled diabetes are profound.
Diagnosis and Tests

Accurate diagnosis relies on comprehensive evaluation, including fasting glucose, oral glucose tolerance tests, and hemoglobin A1c measurements. Screening recommendations aim to identify at-risk individuals early, facilitating timely intervention and risk reduction.
Management and Treatment
Diabetes management strategies encompass pharmacotherapy, lifestyle modifications, patient education, and multidisciplinary care. Individualized treatment plans address glycemic control, blood pressure management, lipid optimization, and prevention of complications.
Prevention
Prevention initiatives target modifiable risk factors through health promotion, public health interventions, and community engagement. Emphasizing the role of nutrition, physical activity, and behavioral changes empowers individuals to mitigate their diabetes risk.
Outlook and Prognosis
Prognostic factors such as glycemic control, adherence to therapy, comorbidity burden, and psychosocial support influence long-term outcomes. Enhanced collaboration among healthcare providers, policymakers, and stakeholders is essential to improve diabetes prognosis globally.
Living With Diabetes

Coping with diabetes requires resilience, self-management skills, and social support networks. Empowering individuals through education, self-monitoring tools, and peer support enhances their capacity to navigate the challenges of daily diabetes management.
Impact on Individuals and Society
Diabetes exerts a profound socioeconomic burden, encompassing healthcare costs, productivity losses, and reduced quality of life. Addressing the psychosocial dimensions of diabetes care is integral to fostering holistic well-being and societal resilience.
Future Directions and Research

Advancements in diabetes research, including precision medicine, digital health technologies, and novel therapeutics, offer promising avenues for disease management and prevention. Collaborative research endeavors aim to translate scientific discoveries into tangible clinical benefits.
Conclusion
In conclusion, diabetes represents public health challenge necessitating a comprehensive, patient-centered approach. By fostering awareness, promoting early detection, and advancing evidence-based interventions, we can mitigate the impact of diabetes on individuals, families, and communities worldwide.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance.
Strategies to Writing a Perfect College Essay

1. Be Authentic
Authenticity is crucial in college essays. It involves selecting a topic or perspective that genuinely reflects who you are. Readers can often discern when a writer is not being authentic, whether it’s through overly embellished language or choosing a topic solely for its perceived impressiveness. Embrace your own voice, use humor naturally, and opt for subjects that hold genuine importance to you, providing a deeper insight into your character.
2. Grab the Reader From the Start
The opening of your essay is a critical opportunity to capture the reader’s attention. A bold statement, a thoughtful quote, an engaging question, or a vivid descriptive scene can set the tone for the entire piece. A clear and compelling thesis statement early on helps guide the reader and establishes the purpose of your essay. This initial impact is essential when competing with numerous other applicants for the admission officer’s attention.
3. Focus on Deeper Themes

Facts and achievements are important, college proffesers are interested in understanding who you are as a person. Delve into deeper themes by connecting your experiences, successes, and adversities to your personal growth. It’s not just about listing accomplishments but demonstrating how those experiences shaped you. This provides a more comprehensive view of your character and journey.
4. Show Don’t Tell

Instead of presenting a mere list of accomplishments, engage the reader by showing scenes and sharing anecdotes. The most captivating essays draw readers into the writer’s world, allowing them to experience the emotional journey. Highlighting the lessons learned and personal insights gained creates a more impactful narrative.
5. Try Doing Something Different
To make your essay stand out, consider approaching your subject from a unique perspective. While common themes like sports-related obstacles or volunteer stories are popular for a reason, exploring a different angle can set you apart. For instance, writing about lessons learned from losses rather than wins can demonstrate resilience and self-awareness.
6. Write With the Reader in Mind

Craft your essay with a clear and logical structure, ensuring that one idea flows naturally into the next. Effective use of transitions between paragraphs enhances the readability of your essay. Anticipate questions the reader might have, and provide the necessary background information. Ensure that the essay is well-organized, avoiding unnecessary wordiness.
7. Write Several Drafts
The importance of multiple drafts cannot be overstated. Setting your essay aside for a few days and returning to it with a fresh perspective often reveals new insights. Starting the writing process early allows sufficient time for revisions. Each draft provides an opportunity to refine your narrative, strengthen arguments, and enhance overall clarity.
8. Read It Aloud

Reading your essay aloud is a valuable editing technique. It helps identify awkward or unnatural-sounding passages. This method allows you to assess the flow of your writing and ensures that your voice remains consistent throughout the essay. It’s an effective way to catch any discrepancies that might be missed during silent reading.
9. Don’t Repeat
Avoid redundancy by not rehashing information already present in other parts of your application. Your essay should contribute new insights, providing a fresh perspective on who you are. Ensure that your essay aligns with the overall theme of your application and directly addresses any questions or prompts given.
10. Ask Others to Read Your Essay

Diverse perspectives are valuable in the editing process. Seek feedback from different individuals, such as teachers, parents, or siblings, to gain varied insights. Pay attention to their interpretations and revise the essay based on their feedback. If any confusion arises among readers, address it through revisions to ensure clarity.
11. Pay Attention to Form
While there might not be strict word limits for college essays, maintaining a balance is crucial. The Common App suggests around 650 words, and adhering to such guidelines is advisable. Additionally, pay attention to formatting details such as readable fonts, proper spacing, and correct dialogue presentation. A visually appealing essay contributes to a positive reader experience.
12. End Your Essay With a “Kicker”

The conclusion is as crucial as the introduction. A “kicker” provides a strong, memorable closing that leaves a lasting impression. It should effectively tie together the key points of your essay, leaving the reader satisfied. Aim for conciseness, coherence, and use vivid details to reinforce the overall message of your essay.
Incorporating these strategies into your college essay writing process can significantly enhance its impact and increase your chances of making a positive impression on admissions officers. Remember, a well-crafted essay can be a powerful tool in differentiating yourself from other applicants
We wish you all the best in your essay writing and studies.
For guidance and and Assistance in all your assignment Help;
Email us at; williamsassignmenthelpfredrick@gmail.com
-
 ripplepipple liked this · 2 weeks ago
ripplepipple liked this · 2 weeks ago -
 syuuchi liked this · 3 weeks ago
syuuchi liked this · 3 weeks ago -
 misharadeva liked this · 1 month ago
misharadeva liked this · 1 month ago -
 paranoidbpd liked this · 1 month ago
paranoidbpd liked this · 1 month ago -
 joannes-fabrics liked this · 4 months ago
joannes-fabrics liked this · 4 months ago -
 nimaah reblogged this · 6 months ago
nimaah reblogged this · 6 months ago -
 aishakhushbu liked this · 7 months ago
aishakhushbu liked this · 7 months ago -
 crystallatticed reblogged this · 7 months ago
crystallatticed reblogged this · 7 months ago -
 prollymaia liked this · 8 months ago
prollymaia liked this · 8 months ago -
 voiddaydreamsystem liked this · 9 months ago
voiddaydreamsystem liked this · 9 months ago -
 grumpyone3 reblogged this · 10 months ago
grumpyone3 reblogged this · 10 months ago -
 grumpyone3 liked this · 10 months ago
grumpyone3 liked this · 10 months ago -
 parkhanyoonjae liked this · 10 months ago
parkhanyoonjae liked this · 10 months ago -
 idle-mind3 liked this · 10 months ago
idle-mind3 liked this · 10 months ago -
 iconstasher reblogged this · 10 months ago
iconstasher reblogged this · 10 months ago -
 dutiful-stranger liked this · 10 months ago
dutiful-stranger liked this · 10 months ago -
 drippin-guac liked this · 11 months ago
drippin-guac liked this · 11 months ago -
 genleecosworth liked this · 1 year ago
genleecosworth liked this · 1 year ago -
 customcabinet liked this · 1 year ago
customcabinet liked this · 1 year ago -
 photomaster66 liked this · 1 year ago
photomaster66 liked this · 1 year ago -
 duressdarling liked this · 1 year ago
duressdarling liked this · 1 year ago -
 jrzyfarmer liked this · 1 year ago
jrzyfarmer liked this · 1 year ago -
 sparky1983 liked this · 1 year ago
sparky1983 liked this · 1 year ago -
 expertacademicassignmenthelp reblogged this · 1 year ago
expertacademicassignmenthelp reblogged this · 1 year ago