ORGANS OF EXCRETION
ORGANS OF EXCRETION

Excretion, a fundamental process in living organisms, plays a critical role in maintaining internal equilibrium and ensuring the efficient removal of waste products. This detailed discussion will involve deeper into the importance of excretion, the organs involved, their functions, and their contributions to overall health and homeostasis.
Importance of Excretion
Excretion is essential for the survival of all living organisms, from single-celled organisms to complex multicellular organisms like humans. It involves the elimination of metabolic waste products, toxins, and excess substances that accumulate within the body. By removing these waste materials, excretion helps regulate the internal environment, ensuring optimal conditions for cellular function and metabolic processes. Without effective excretory mechanisms, the buildup of waste products would lead to toxicity, impaired physiological function, and ultimately, organismal death.
Organs of Excretion
The human body employs a variety of organs for excretion, each with its own specialized functions and mechanisms for waste elimination. These organs include the skin, liver, large intestine, lungs, and kidneys. While some organs primarily eliminate specific types of waste products, others have multifunctional roles in metabolism, digestion, and detoxification, in addition to excretion.
1. Skin
The skin, the body’s largest organ, serves as a multifunctional barrier between the internal and external environments. In addition to its protective role, the skin participates in excretion through the production of sweat by sweat glands located in the dermis. Sweat, composed of water, salts, and urea, is released through sweat pores onto the skin’s surface, where it evaporates and helps regulate body temperature. Sweating also facilitates the elimination of metabolic wastes, toxins, and excess salts from the body, contributing to overall homeostasis.
2. Liver

The liver, a vital organ located in the upper right abdomen, is involved in numerous metabolic processes, including digestion, detoxification, and the synthesis of essential molecules. As part of its excretory function, the liver processes and eliminates various waste products and toxins from the bloodstream. It metabolizes ammonia, a toxic byproduct of protein metabolism, into urea, a less toxic compound that is excreted by the kidneys in urine. Additionally, the liver excretes bilirubin, a waste product of heme metabolism, into bile, which is then eliminated from the body through the feces.
3. Large Intestine

The large intestine, the final segment of the gastrointestinal tract, plays a crucial role in the absorption of water and electrolytes from undigested food residues. In addition to its role in digestion and water reabsorption, the large intestine serves as a site for the accumulation and elimination of solid waste materials. Bile pigments, such as bilirubin, are excreted into the gastrointestinal tract via bile and eventually eliminated in feces, contributing to the characteristic color of stool.
4. Lungs

The lungs, the primary organs of respiration, also play a role in excretion by removing gaseous waste products, such as carbon dioxide, from the bloodstream. During the process of cellular respiration, carbon dioxide is produced as a byproduct and transported via the bloodstream to the lungs for elimination. Through the process of gas exchange in the alveoli, carbon dioxide is expelled from the body during exhalation, helping to regulate blood pH and maintain acid-base balance.
5. Kidneys

The kidneys are often regarded as the primary organs of excretion in the human body, responsible for filtering waste products and excess substances from the bloodstream and producing urine for elimination. Each kidney contains millions of functional units called nephrons, which play a crucial role in the filtration, reabsorption, and secretion of various substances. Nephrons filter blood to remove waste products, such as urea, creatinine, and uric acid, while reabsorbing essential nutrients and maintaining electrolyte balance. The resulting urine is then transported from the kidneys to the urinary bladder via the ureters and excreted from the body through the urethra during urination.
6. Urinary System

The kidneys, along with the ureters, urinary bladder, and urethra, collectively form the urinary system, which functions to transport, store, and eliminate urine from the body. The ureters carry urine from the kidneys to the urinary bladder, where it is stored until it is expelled from the body through the urethra. The urinary system plays a crucial role in maintaining fluid balance, electrolyte concentration, and pH regulation within the body, thereby supporting overall homeostasis and physiological function.
Conclusion
In conclusion, excretion is a vital process that enables living organisms to eliminate waste products and maintain internal balance. Through the coordinated efforts of various organs, including the skin, liver, large intestine, lungs, and kidneys, the body effectively removes metabolic wastes, toxins, and excess substances, thereby supporting overall health and homeostasis. Understanding the mechanisms of excretion and the roles of excretory organs is essential for appreciating the complexity of physiological regulation and the interconnection of bodily systems. By studying excretory processes, researchers and healthcare professionals can gain insights into disease mechanisms, develop therapeutic interventions, and promote optimal health and well-being.
For students seeking guidance and assistance with their academic assignments, Expert Academic Assignment Help stands out as an invaluable resource. With their unique and top-notch content, they offer solutions to various academic challenges, ranging from essays to research papers ,Clinical case studies and homework. Don’t hesitate to reach out to them for expert assistance and take your academic journey to the next level. For inquiries, contact expertassignment46@gmail.com
More Posts from Expertacademicassignmenthelp and Others
The Pathophysiology and Therapeutic Intervention of Migraine

Introduction
Migraine, a prevalent neurological disorder characterized by recurrent headaches, sensory disturbances, and autonomic dysregulation, poses a significant global health burden. We are going to provide a comprehensive review citing out the unique pathophysiological mechanisms underlying migraine and discuss the evolving landscape of therapeutic interventions.
Understanding Migraine Pathophysiology

1. Genetic Predisposition
Migraine exhibits a strong familial aggregation, suggesting a genetic component in its etiology. Genome-wide association studies have identified numerous susceptibility loci implicated in migraine susceptibility, including genes involved in neuronal excitability, neurotransmitter release, and vascular regulation.
2.Environmental Factors
Environmental triggers such as stress, sleep disturbances, hormonal fluctuations, dietary factors, and sensory stimuli play a crucial role in migraine onset and exacerbation. These triggers interact with genetic predispositions to precipitate migraine attacks, underscoring the threshold nature of the disorder.
Sensory Processing Abnormalities
Migraine pathophysiology revolves around the concept of a cyclic sensory threshold model, wherein aberrant processing of sensory inputs leads to hypersensitivity and pain amplification. Dysregulation of cortical excitability, thalamocortical networks, and descending pain modulatory pathways contribute to the sensory manifestations of migraine.
Phases of Migraine

Migraine progression is characterized by distinct phases, including premonitory, aura, pain, and postdrome phase, each associated with specific neurophysiological changes. The premonitory phase, marked by various symptoms preceding the headache, reflects hypothalamic and brainstem activation. Aura, a transient neurological phenomenon, involves cortical spreading depression and cortical spreading depolarization, leading to visual, sensory, or motor disturbances. The pain phase, mediated by trigeminal vascular activation and central sensitization, culminates into headache and associated symptoms. The postdrome phase, characterized by residual symptoms following headache resolution, implicates persistent alterations in cortical and brainstem function.
a) Trigeminal vascular System

Central to migraine pathophysiology is the trigeminal vascular system, comprising peripheral trigeminal afferents and central brain nuclei involved in pain processing. Activation of trigeminal vascular pathways, mediated by neuropeptides like Calcitonin gene-related peptide, substance P, and neurokinin A, initiates neurogenic inflammation and sensitization of meningeal nociceptors, contributing to headache generation.
b) Brainstem Nuclei
Brainstem regions, including the dorsolateral pons, periaqueductal gray, and locus coeruleus, serve as crucial modulators of trigeminal vascular transmission. Dysregulation of brainstem nuclei leads to unbearable pain processing and autonomic dysfunction, characteristic of migraine attacks.
c) Hypothalamic Involvement
The hypothalamus plays an important role in migraine initiation and progression, integrating nociceptive, autonomic, and circadian inputs. Dysregulation of hypothalamic neurotransmitters, including orexin, serotonin, and dopamine, contributes to migraine susceptibility and triggers stress-induced attacks.
d) Thalamic Dysfunction
The thalamus, a key relay station in sensory processing, exhibits structural and functional abnormalities in migraine. Altered thalamocortical connectivity, thalamic excitability, and neurotransmitter imbalance contribute to central sensitization, photophobia, and allodynia, hallmark features of migraine.
e) Cortical Alterations
Beyond aura generation, the cerebral cortex demonstrates widespread abnormalities in migraineurs, including changes in cortical thickness, gray matter volume, and functional connectivity. Genetic variants associated with glutamatergic neurotransmission and cortical excitability further implicate cortical dysfunction in migraine pathophysiology.
Therapeutic Approaches

a) Acute Treatments
Triptans, serotonin receptor agonists, have long been the mainstay of acute migraine therapy. However, emerging classes of medications, including ditans and gepants, offer alternative treatment options with improved tolerability and efficacy. Lasmiditan, a selective 5-HT1F receptor agonist, provides rapid relief without vasoconstrictive effects, making it suitable for patients with contraindications to triptans. Gepants, small-molecule CGRP receptor antagonists, block CGRP-mediated vasodilation and neurogenic inflammation, offering effective pain relief without cardiovascular risks.
b) Preventive Treatments
Monoclonal antibodies targeting CGRP or its receptors represent a breakthrough in migraine prevention, providing sustained efficacy with monthly or quarterly dosing regimens. Erenumab, fremanezumab, and galcanezumab have demonstrated superior efficacy compared to placebo in reducing migraine frequency and severity, with favorable safety profiles. Gepants such as atogepant and Rimegepant offer additional options for migraine prophylaxis, particularly in patients intolerant to traditional preventive therapies.
c) Neuromodulation Techniques
Non-invasive neuromodulation modalities, including transcranial magnetic stimulation and transcutaneous supraorbital nerve stimulation, offer adjunctive therapeutic options for acute migraine management. TMS delivers magnetic pulses to cortical regions implicated in migraine pathophysiology, modulating cortical excitability and pain perception. tSNS targets the supraorbital nerve, inhibiting nociceptive transmission and providing rapid pain relief without systemic side effects. Additionally, vagus nerve stimulation (VNS) offers a promising approach for both acute and preventive migraine treatment, modulating autonomic function and central pain processing.
Conclusion
In conclusion, migraine represents a complex neurological disorder with a diverse clinical manifestations. Advances in our understanding of migraine pathophysiology have paved the way for the development of novel therapeutic agents targeting key molecular and neural pathways. By understanding the interplay between genetic predisposition, sensory processing abnormalities, and central pain modulation, clinicians can tailor treatment strategies to individual patient needs, optimizing therapeutic outcomes and improving quality of life for migraine patients worldwide. Continued research efforts and clinical innovations hold the promise of further advancements in migraine management, underscoring the collective commitment to alleviating the global burden of this devastating condition.
Understanding the pathophysiology of migraine is crucial for effective management, and this comprehensive analysis sheds light on the complex mechanisms underlying this neurological disorder. For medical students facing challenges in studying migraine or any other medical topic, seeking professional help from Expert Academic Assignment Help can provide valuable guidance and support. With our expert assistance, students can overcome obstacles and excel in their academic endeavors. Contact us at expertassignment46@gmail.com to elevate your understanding and mastery of medical concepts.
Osteoporosis in Aging

Introduction
Osteoporosis, a progressive skeletal disorder characterized by reduced bone mass and deteriorating bone quality, poses significant health challenges, especially among the aging population. This discussion involves dynamics of bone health, the factors contributing to osteoporosis, and proactive measures individuals can adopt to protect and strengthen their bones as they age.
1.Understanding Bone Structure and Dynamics
Bones, seemingly solid, have an internal honeycomb-like structure. This structural framework undergoes constant remodeling, with cells building new bone tissue while others dissolve existing bone to release essential minerals. As individuals age, this delicate balance shifts, resulting in a gradual loss of bone density and an increased susceptibility to fractures.
2.Prevalence and Impact of Osteoporosis
Osteoporosis is a widespread concern, affecting over 10 million people nationwide. Its consequences, particularly in Adults, extend beyond fractures, leading to a variety of issues such as disability and loss of dependence. The vulnerability of specific areas, including the;
hips, wrists, and spine, underscores the importance of understanding and addressing this condition.
3.Hormonal Influence and Screening
Estrogen, a crucial hormone, plays a major role in bone formation and regeneration. Postmenopausal women, experiencing a decline in estrogen levels, face a high risk of an increased bone loss. Regular screening, typically recommended for women aged 65 and older, involves non-invasive tests like;
Bone density scan(DXA), measuring bone mineral density. A total score of -2.5 or lower is indicative of osteoporosis.
4.Nutritional Factors
The role of nutrition in maintaining bone health cannot be overstated. Calcium, an essential mineral for bone strength and formation, is obtainable from various dietary sources such as, dairy products and leafy greens. Vitamin D, facilitating calcium absorption, becomes increasingly critical with age. This emphasizes the importance of adequate nutrient intake, either through dietary means or supplements. Specific daily calcium requirements for women over 50 and men over 70 are outlined.
5.Exercise as a Protective Measure
Physical activity, especially weight-bearing exercises like jogging, walking, tennis, and dancing, significantly contributes to bone health. These exercises serve as signals to bone cells, promoting density and reducing the risk of fractures. Conversely, lifestyle choices such as smoking and heavy drinking weaken bones, while certain medications may increase the risk of osteoporosis.
Medical Interventions and Future Prospects
Medical interventions, including medications like bisphosphonates, are commonly prescribed to combat bone loss. Ongoing research is exploring drugs aimed at stimulating bone growth, with parathyroid hormone being a current option. The article discusses the potential of these interventions and highlights the importance of timely medical advice and interventions, even after an osteoporosis diagnosis, to positively impact bone health.
Fall Prevention and Fracture Avoidance
More than 2 million fragility fractures occur annually due to falls, highlighting the need for a comprehensive approach to bone health. Combining efforts to enhance bone strength with fall prevention strategies is crucial. Factors such as balance, environmental hazards, and the type of fall play significant roles in fracture risk. The discussion underscores the effectiveness of exercises that improve balance and coordination, such as slow intentional movement in preventing fractures.
Conclusion
Maintaining optimal bone health is a course that involves a combination of nutrition, exercise, and proactive healthcare measures. Given the critical impact of osteoporosis on aging populations, raising awareness and implementing early intervention strategies are paramount. This comprehensive approach empowers individuals to foresee the risks associated with osteoporosis, ensuring a resilient and active lifestyle in their later years. The discussion concludes by encouraging individuals concerned about their bone health to engage or consult with their healthcare specialists, pressing on the importance of personalized guidance and bone density testing for proactive management.
For Health Sciences Assignment Help;
Email us at;
williamsliason@outlook.com
What Makes a PhD Dissertation Different from a Masters Thesis?

Introduction
In the realm of academia, pursuing advanced degrees such as a Master’s or a PhD involves rigorous research and scholarly endeavors. Central to this academic journey are the culminating projects — the Master’s thesis and the PhD dissertation. While often used interchangeably, these two academic works possess distinct characteristics that set them apart. In this comprehensive discussion, we will major into the differences between a PhD dissertation and a Master’s thesis, exploring various aspects including the depth of research, original contribution to knowledge, duration and intensity of study, evaluation and defense process, as well as career implications and academic prestige.
Depth of Research

One of the fundamental disparities between a PhD dissertation and a Master’s thesis lies in the depth of research. A Master’s thesis typically explores a specific topic within a field of study, offering a comprehensive analysis but within a more confined framework. In contrast, a PhD dissertation delves into original research, contributing novel insights or advancing existing knowledge within the chosen discipline. The depth of investigation required for a dissertation is considerably greater, often involving extensive data collection, analysis, and interpretation.
Original Contribution to Knowledge

Building upon the notion of originality, a PhD dissertation is expected to make a significant contribution to the body of knowledge within the respective field. It must demonstrate a unique perspective, innovative methodology, or novel findings that add value to the academic discourse. On the other hand, while a Master’s thesis also involves original research, its contribution may be more incremental or focused on synthesizing existing literature rather than forging new paths of inquiry.
Duration and Intensity of Study

Another factor that distinguishes a PhD dissertation from a Master’s thesis is the duration and intensity of study involved. Pursuing a PhD typically entails a more prolonged and immersive engagement with the research topic, spanning several years of dedicated study and inquiry. The process of conducting original research, analyzing data, and drafting a dissertation demands a substantial commitment of time and effort. In contrast, a Master’s thesis can often be completed within a shorter timeframe, typically ranging from one to two years, depending on the program’s requirements.
Evaluation and Defense Process
The evaluation and defense process also differ between a PhD dissertation and a Master’s thesis. For a PhD dissertation, the candidate must present their research findings to a committee of faculty members or experts in the field. This oral defense involves a rigorous examination of the dissertation’s methodology, results, and conclusions, as well as the candidate’s ability to articulate and defend their research. In contrast, while some Master’s programs may require a thesis defense, the level of scrutiny and formality is often less intense compared to a PhD dissertation defense.
Career Implications and Academic Prestige

Furthermore, the completion of a PhD dissertation carries significant career implications and academic prestige. Attaining a PhD is often regarded as the highest level of academic achievement, opening doors to advanced research positions, teaching opportunities, and leadership roles within academia and industry. A PhD dissertation serves as a hallmark of expertise and scholarly rigor, signaling to the academic community and potential employers the candidate’s ability to conduct independent research at a high level. On the other hand, while a Master’s thesis is a commendable accomplishment in its own right, it may not carry the same weight in terms of career advancement or academic recognition as a PhD dissertation.
Conclusion
In conclusion, the comparison between a PhD dissertation and a Master’s thesis reveals the intricate differences that exist between these two academic endeavors. While both represent significant milestones in academic scholarship, they embody distinct attributes that reflect the depth of research, originality of contribution, and level of academic achievement. Whether seeking thesis vs. dissertation writing help or PhD dissertation assistance, students embarking on these scholarly endeavors can benefit from the guidance and support offered by dissertation writing services. With expert assistance, aspiring scholars can navigate the complexities of research, writing, and presentation, ensuring their academic work meets the highest standards of excellence and scholarly rigor
Understanding the differences between a PhD dissertation and a Master’s thesis is crucial for students embarking on academic research. Expert Academic Assignment Help offers personalized support at every stage of the process, ensuring academic excellence. Reach out at expertassignment46@gmail.com to benefit from expertise and guidance in navigating the complexities of research, writing, and presentation.
10 Strategies For Handling Online Exams.

Online examinations have emerged as a reliable method for evaluating students in today’s digital era. However, navigating through these virtual assessments can present challenges, particularly for individuals new to the format or struggling to adapt. Fortunately, online exam assignment assistance services like Expert Academic Assignment Help provide invaluable guidance to students, empowering them not only to approach examinations with confidence but also to excel in them. Let’s focuses into ten effective strategies recommended by assignment assistance experts to successfully ace online examinations.
1. Familiarize Yourself With The Exam Format
Understanding the structure and format of the examination is paramount. By comprehending what to anticipate, students can better prepare their study approach and manage their time effectively during the examination.
2. Create A Study Schedule
Effective time management is imperative. Establishing a study schedule that encompasses dedicated time for reviewing course materials, practicing sample questions, and undertaking mock examinations ensures comprehensive preparation.
3. Utilize Online Resources
Exploit the varieties of online resources available to supplement learning. Websites, forums, and educational platforms offer a treasure trove of information, including study guides and interactive quizzes, augmenting students’ understanding of the examination material.
4. Practice Regularly
Practice breeds perfection. Allocating time each day to tackle examination questions under timed conditions not only enhances speed and accuracy but also diminishes anxiety by acquainting students with the examination interface.
5. Seek Clarification
Do not hesitate to seek clarification from instructors or peers when encountering difficulties or questions about the examination material. Engaging in discussions through online forums or study groups can enrich understanding and boost confidence.
6. Minimize Distractions
Cultivating a conducive study environment by minimizing distractions is imperative. Identifying a tranquil, well-lit space and disabling electronic device notifications optimize concentration and information retention.
7. Take Regular Breaks
Striking a balance between study sessions and short breaks is crucial for sustaining focus and preventing burnout. Rejuvenating the mind with stretching and relaxation exercises ensures optimal performance.
8. Develop Exam Strategies
Mastery of effective examination strategies can significantly enhance performance. Learning to prioritize questions, manage time efficiently, and utilize available resources enriches examination outcomes.
9. Review And Revise
Thoroughly reviewing course materials in the days leading up to the examination reinforces comprehension and aids retention. Crafting summary notes and mnemonic devices facilitates the recall of key concepts and definitions.
10. Stay Calm And Confident

On the day of the examination, maintaining composure and confidence is paramount. Trusting in one’s preparation, staying focused, and approaching each question methodically are important contributors to success.
In conclusion, mastering online examinations necessitates thorough preparation, consistent practice, and strategic thinking. By adhering to these ten strategies and availing themselves of support from online exam assignment assistance services like Expert Academic Assignment Help, students can elevate their performance, surmount challenges, and attain academic success. With dedication, perseverance, and the right support system in place, excelling in online examinations is entirely attainable.
The strategies for handling online exams is essential for achieving academic success in the digital era. If you’re aiming to enhance your performance and ensure success in your online examinations, don’t hesitate to reach out to Expert Academic Assignment. Connect with us via email: expertassignment46@gmail.com to explore how our specialized assistance can elevate your exam preparation and performance. Remember, seeking support when needed is a wise decision, particularly when it comes to excelling in challenging assessments like online exams.
Medical ethics

Medical ethics is a complex field that intersects with various aspects of
1.Medicine
2. Ethics
3.Philosophy and
5.Society
The study of medical ethics involves the exploration of moral values and judgments as they pertain to the practice of medicine. This interdisciplinary field delves into the practical application of ethical principles in clinical settings and encompasses a broader understanding of its history, philosophy, theology, and sociology.
Historical Evolution:
The roots of Western medical ethics can be traced back to ancient guidelines, including the famous Hippocratic Oath. In the medieval and early modern period, contributions from Muslim physicians like Ishaq bin Ali Rahawi and figures such as Maimonides and Thomas Aquinas shaped ethical discourse. The emergence of a self-conscious discourse around medical ethics gained momentum in the 18th and 19th centuries, with notable figures like Thomas Percival contributing to the ethical framework. In 1847, the American Medical Association adopted its first code of ethics, rooted in Percival’s work.
Core Values in Medical Ethics:
Six fundamental values commonly applied in medical ethics discussions are:
1.Autonomy
Emphasizes a patient’s right to refuse or choose their treatment, rooted in the principle of self-determination.
2.Beneficence
Advocates for practitioners to act in the best interest of the patient, prioritizing their well-being.
3.Non-maleficence
Encompasses the principle of “first, do no harm,” emphasizing the importance of avoiding harm to the patient.
4.Justice
Focuses on the fair distribution of scarce health resources and the ethical decision-making process concerning who receives what treatment.
5.Dignity
Recognizes the right to dignity for both the patient and the healthcare provider.
6.Truthfulness and Honesty
Stresses the significance of informed consent, gaining prominence after historical events like the Nuremberg trials and Tuskegee Syphilis Study.
Ethical Dilemmas and Resolutions:
Ethical conflicts often arise when these values are in conflict, leading to dilemmas that require careful consideration. For instance, conflicts between autonomy and beneficence/non-maleficence can occur when patients disagree with recommended treatments. Euthanasia presents a poignant example where autonomy clashes with the principle of preserving life.
Informed Consent and Confidentiality:
Informed consent is a critical aspect of medical ethics, ensuring that individuals are fully informed about the potential benefits and risks of their chosen treatment. Confidentiality, including patient-physician privilege, is a cornerstone, with legal protections in place.
Criticisms and Cultural Considerations:
Medical ethics faces criticisms, including bias in a framework where individuals may not be free to contract for medical treatment. The balance between beneficence and autonomy is debated, with considerations about state or supplier group interests over patient welfare.
Cultural differences can complicate medical ethics, as diverse beliefs about disease origins and treatment may conflict with Western medicine. Practices like truth-telling vary among cultures, impacting the doctor-patient relationship.
Conflicts of Interest and Online Practices:
Physicians must navigate conflicts of interest to ensure unbiased medical judgment. Online business practices have introduced challenges, with concerns about the influence of pharmaceutical companies and the commodification of medical diagnoses.
Importance of Communication:
Open lines of communication are crucial in resolving ethical conflicts. Communication breakdowns among patients, healthcare teams, family members, and the medical community can lead to disagreements. Remedying these breakdowns is essential for ethical problem-solving.
Control and Resolution Mechanisms:
Hospital accreditation emphasizes ethical considerations, including physician integrity, conflicts of interest, research ethics, and organ transplantation ethics. Ethical guidelines, such as the Declaration of Helsinki, provide a framework, and ethics committees play a role in deciding complex matters.
Future Challenges and Developments:
As medical ethics continues to evolve, ongoing challenges include addressing cultural differences, advancing communication practices, and adapting to the changing landscape of healthcare, including the role of technology and online platforms.
In conclusion, medical ethics is a dynamic and multifaceted field that constantly grapples with the evolving landscape of medicine and society. Its principles serve as a compass for healthcare professionals, ensuring ethical decision-making and the promotion of patient welfare. The field’s rich history, diverse values, and ongoing challenges contribute to its significance in shaping the ethical dimensions of medical practice.
For Health Sciences Assignment Help;
Email Us At;
williamsliason@outlook.com
How to Write Nursing Research Papers The process of nursing research paper writing involves exploring relevant issues within the field and proposing viable solutions. The complexity of nursing necessitates in-depth research, analytical thinking, and critical analysis. Topics may span various areas such as psychiatric nursing, healthcare management, evidence-based medicine, clinic hygiene, home-based healthcare, healthcare practices, and ethics, all of which revolve around the central goal of alleviating patient suffering and addressing their psychological well-being. Before delving into the writing process, it is crucial to determine the type of research paper – analytical or argumentative. Analytical research papers involve a specific analysis of issues or literary texts, employing designs like question/answer, comparison/contrast, problem/solution, cause/effect, hypothesis/proof, or change over time. On the other hand, argumentative research papers focus on presenting diverse viewpoints on a debatable issue, requiring an investigation of different studies to provide compelling arguments while addressing opposing views objectively. Selecting an appropriate topic is a critical aspect of the research paper process. The chosen topic should be specific, relevant to nursing, interesting to the writer, and within the prescribed length and format guidelines. Topics like Nursing Science During the 20th Century, Nurses’ Safety on the Working Place, or The Importance of Neonatal Care Nursing exemplify suitable choices. Once a topic is chosen, the next step involves sourcing information from reliable primary, secondary, and tertiary sources. Primary sources include original materials like academic journals, interviews, surveys, and court records. Secondary sources analyze or describe primary sources, encompassing books, articles, encyclopedias, dictionaries, and textbooks. Tertiary sources aid in organizing or locating both primary and secondary sources and typically involve databases and indexes. Pre-writing activities, such as brainstorming, freewriting, mindmapping, and outlining, play a pivotal role in organizing ideas before the actual writing process. These activities help in collecting and structuring major points and arguments effectively. In terms of formatting styles, the APA style is commonly used in nursing research papers. It dictates a specific structure with a title page, abstract, main body, and reference page. In-text citations follow a specific format with the author's last name and year of publication. The entire paper is typed in twelve-point Times New Roman font. The basic structure of a nursing research paper includes a title page containing the title, running head, author’s name, and institutional affiliation. The abstract, written on a separate page, provides a summary of key points, not less than 250 words, along with keywords. The main body comprises an introduction, body paragraphs addressing each point from the abstract with citations, and a conclusion restating the thesis and supporting arguments. The reference page, placed after the main body, lists all sources alphabetically with one-half inch indentation. Adhering to these guidelines ensures the creation of a well-structured and comprehensive nursing research paper. For further assistance contact us at williamsliason@outloock.com
Pulmonary Edema

Introduction
Pulmonary edema is a condition that results from the abnormal accumulation of fluid in the lungs, leading to impaired gas exchange and respiratory distress. This comprehensive discourse aims to provide an in-depth analysis of pulmonary edema, covering its pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications.
Pathophysiology of Pulmonary Edema

Pulmonary edema develops when there is an imbalance between the hydrostatic and oncotic pressures within the pulmonary vasculature. This imbalance leads to an increase in capillary permeability and the extravasation of fluid into the interstitial space and alveoli of the lungs. Several mechanisms contribute to this process, including increased capillary hydrostatic pressure due to heart failure, increased vascular permeability due to inflammation or injury, and decreased oncotic pressure due to hypoalbuminemia or capillary leak syndrome.
Etiology of Pulmonary Edema
The etiology of pulmonary edema can be categorized into cardiogenic and noncardiogenic causes. Cardiogenic pulmonary edema occurs secondary to heart failure or other cardiac conditions that result in elevated left atrial pressure and pulmonary venous congestion. Noncardiogenic pulmonary edema, on the other hand, is caused by factors unrelated to heart dysfunction, such as acute respiratory distress syndrome (ARDS), aspiration, sepsis, or neurogenic pulmonary edema.
Clinical Manifestations of Pulmonary Edema

The clinical presentation of pulmonary edema varies depending on the underlying cause and severity of the condition. Common symptoms include dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, frothy sputum, cyanosis, and crackles on auscultation. Severe cases may progress to respiratory failure, hypoxemia, and hemodynamic instability.
Diagnostic Modalities for Pulmonary Edema

Diagnosing pulmonary edema requires a thorough clinical evaluation, including a detailed medical history, physical examination, and various diagnostic tests. Imaging studies such as chest X-ray, computed tomography (CT) scan, and lung ultrasound can provide valuable information about lung parenchymal changes and the presence of pulmonary congestion. Laboratory tests, including arterial blood gas analysis, brain natriuretic peptide levels, and electrolyte measurements, may also aid in the diagnosis and assessment of disease severity.
Treatment Strategies for Pulmonary Edema
The management of pulmonary edema involves addressing the underlying cause, relieving symptoms, and preventing complications. Initial treatment often includes supplemental oxygen therapy to improve oxygenation and reduce respiratory distress. Diuretics, such as furosemide or bumetanide, are commonly used to reduce fluid overload and alleviate pulmonary congestion. In cases of cardiogenic pulmonary edema, vasodilators, inotropes, or mechanical ventilation may be necessary to improve cardiac function and gas exchange.
Prevention Strategies for Pulmonary Edema
Preventing pulmonary edema requires a broad approach aimed at managing underlying risk factors and promoting healthy lifestyle habits. Patients with known cardiac conditions should adhere to prescribed medications, maintain a low-sodium diet, and monitor fluid intake to prevent fluid retention and exacerbation of heart failure. Individuals at risk of noncardiogenic pulmonary edema should avoid exposure to toxins, practice proper respiratory hygiene, and seek prompt medical attention for respiratory infections or injuries.
Complications of Pulmonary Edema

Untreated or inadequately managed pulmonary edema can lead to several complications, including acute respiratory distress syndrome (ARDS), cardiogenic shock, acute kidney injury, pulmonary hypertension, and death. Prompt recognition and intervention are essential to prevent progression to these life-threatening complications and improve patient outcomes.
Conclusion
Pulmonary edema is a complex and potentially life-threatening condition that requires prompt recognition, accurate diagnosis, and appropriate management. By understanding the underlying pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications of pulmonary edema, healthcare providers can optimize patient care and outcomes. Continued research efforts aimed at elucidating the mechanisms underlying pulmonary edema and identifying novel therapeutic targets are essential to further improve patient outcomes and reduce the global burden of this condition.
Embarking on your journey in the field of medicine is both exciting and challenging. As you navigate through your rigorous study period, it’s essential to seek guidance and assistance whenever needed to ensure your success.
At Expert Academic Assignment Help, we understand the demands of medical education and are here to support you every step of the way. Whether you require assistance with assignments, research papers, or exam preparation, our team of experts is dedicated to providing you with the help you need to excel in your studies.
Don’t hesitate to reach out to us for guidance, academic support, or any questions you may have. You can contact us via email at expertassignment46@gmail.com
14 Common Lung Diseases

Introduction
Lung diseases represent some of the most severe health threats globally. The rise of industrialization, environmental pollution, and tobacco usage significantly contribute to the prevalence of these diseases. This article, outlines the most common lung diseases, their symptoms, causes, and treatments.
1. Pneumonia

Pneumonia is an inflammation of the lung parenchyma caused by bacteria, viruses, fungi, or other pathogens. It poses a significant risk to the elderly, immunocompromised individuals, and those with chronic conditions but can also affect healthy individuals. Pneumonia can be classified based on the causative agent, such as bacterial pneumonia (e.g., Streptococcus pneumoniae), viral pneumonia (e.g., influenza virus), or fungal pneumonia (e.g., Pneumocystis jirovecii).
Symptoms
Fever
Cough with sputum
Chest pain
Shortness of breath
Fatigue
Sweating and shaking chills
Nausea, vomiting, or diarrhea (less common)
Diagnosis Diagnosis of pneumonia typically involves a combination of patient history, physical examination, chest X-rays, and sputum cultures. Blood tests may also be conducted to identify the causative agent.
Treatment Depending on the cause, treatments may include:
Antibiotics for bacterial pneumonia.
Antiviral medications for viral pneumonia.
Antifungal therapies for fungal pneumonia. Supportive care such as rest, fluids, and over-the-counter medications to reduce fever and manage pain can also alleviate symptoms. In severe cases, hospitalization may be required to provide intravenous antibiotics, oxygen therapy, or mechanical ventilation.
2. Bronchitis

Bronchitis involves the inflammation of the bronchial tubes, which carry air to and from the lungs. It can be acute, often following colds or the flu, or chronic, usually resulting from smoking or long-term exposure to irritants like pollution or dust.
Symptoms
Persistent cough (productive or dry)
Sputum production (clear, white, yellowish-gray, or green)
Fatigue
Shortness of breath
Slight fever and chills
Chest discomfort
Diagnosis Diagnosis typically involves a physical examination, where a doctor listens to the patient’s lungs with a stethoscope. Additional tests, such as a chest X-ray, sputum tests, or pulmonary function tests, may be conducted to rule out other conditions like pneumonia or asthma.
Treatment
Acute bronchitis: Symptomatic treatment includes rest, fluids, and over-the-counter pain relievers and cough medications. Inhalers or nebulizers may be prescribed to ease breathing.
Chronic bronchitis: Management may involve bronchodilators, steroids, and pulmonary rehabilitation. Smoking cessation and avoiding lung irritants are crucial for treatment.
3. Chronic Obstructive Pulmonary Disease (COPD)

COPD is a progressive, irreversible disease characterized by chronic inflammation of the airways, primarily due to smoking, environmental pollutants, or long-term exposure to respiratory irritants. COPD includes chronic bronchitis and emphysema, conditions that often coexist and lead to airflow obstruction.
Symptoms
Chronic cough
Sputum production
Shortness of breath, especially during physical activities
Wheezing
Chest tightness
Frequent respiratory infections
Fatigue
Unintended weight loss (in advanced stages)
Diagnosis COPD is diagnosed through a combination of patient history, physical examination, and spirometry, a test that measures the amount of air a person can exhale and how quickly they can do so. Chest X-rays, CT scans, and arterial blood gas analysis may also be used.
Prevention and Treatment Preventive measures include:
Smoking cessation
Vaccinations (influenza and pneumococcal vaccines)
Reducing exposure to lung irritants
Treatments involves;
Bronchodilators to relax the muscles around the airways
Inhaled steroids to reduce airway inflammation
Pulmonary rehabilitation programs
Oxygen therapy for severe cases
Surgery (e.g., lung volume reduction surgery or lung transplant) in advanced cases
4. Lung Cancer

Lung cancer involves the uncontrolled growth of malignant cells in the lung tissues. Major risk factors include smoking, exposure to secondhand smoke, exposure to carcinogens (e.g., asbestos, radon), and genetic predisposition.
Types
Small cell lung cancer (SCLC): Often linked to heavy smoking, SCLC is aggressive and spreads quickly.
Non-small cell lung cancer (NSCLC): More common and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Symptoms
Persistent cough
Chest pain
Weight loss
Hemoptysis (coughing up blood)
Shortness of breath
Hoarseness
Bone pain (in advanced stages)
Headache (if cancer spreads to the brain)
Diagnosis Diagnosis involves imaging tests (chest X-rays, CT scans, PET scans), sputum cytology, and tissue biopsy. Molecular testing may be done to identify specific genetic mutations that can be targeted with specific treatments.
Treatment
Surgery to remove the tumor or part of the lung
Chemotherapy to kill cancer cells
Radiation therapy to destroy cancer cells or shrink tumors
Targeted drug therapies to attack specific genetic changes in cancer cells
Immunotherapy to help the immune system fight cancer
5. Pleurisy
Pleurisy, or pleuritis, is the inflammation of the pleura, the tissue lining the lungs and chest cavity. It can be caused by infections (viral, bacterial, or fungal), injuries, autoimmune diseases (e.g., lupus, rheumatoid arthritis), or other underlying conditions.
Symptoms
Sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing
Shortness of breath
Cough
Fever (if infection is present)
Diagnosis Diagnosis involves a physical examination, chest X-rays, ultrasound, CT scans, and blood tests to identify the underlying cause. Thoracentesis, a procedure to remove and analyze pleural fluid, may be performed.
Treatment Treatment depends on the underlying cause and may include:
Antibiotics for bacterial infections
Antiviral medications for viral infections
Anti-inflammatory medications (e.g., NSAIDs) to reduce pain and inflammation
Pain management with medications
Thoracentesis to drain excess fluid from the pleural space
6. Pulmonary Embolism

A pulmonary embolism (PE) occurs when a blood clot, usually originating in the legs (deep vein thrombosis), travels to the lungs, blocking blood flow and causing tissue damage. Risk factors include prolonged immobility, surgery, cancer, and certain genetic conditions.
Symptoms
Sudden shortness of breath
Chest pain (may be sharp and worsen with deep breathing or coughing)
Cough (sometimes with bloody sputum)
Rapid or irregular heartbeat
Lightheadedness or dizziness
Leg pain or swelling (if DVT is present)
Diagnosis: Diagnosis involves imaging tests such as chest X-rays, CT pulmonary angiography, and ventilation-perfusion (V/Q) scans. D-dimer blood tests and ultrasound of the legs may also be conducted.
Treatment Immediate treatment includes:
Anticoagulants (blood thinners) to prevent further clotting
Thrombolytics (clot-dissolving medications) for severe cases
Surgical or catheter-based procedures to remove the clot
Long-term anticoagulation therapy to prevent recurrence
7. Pulmonary Edema

Pulmonary edema is the accumulation of fluid in the lung alveoli, making breathing difficult. It can result from heart failure (cardiogenic pulmonary edema), acute respiratory distress syndrome (ARDS), or exposure to high altitudes (non-cardiogenic pulmonary edema).
Symptoms
Difficulty breathing (dyspnea), especially when lying down
Rapid heartbeat (tachycardia)
Wheezing or gasping for breath
Coughing up frothy, pink-tinged sputum
Excessive sweating
Cyanosis (bluish skin or lips)
Diagnosis Diagnosis involves physical examination, chest X-rays, and blood tests. Echocardiography and pulmonary artery catheterization may be used to determine the underlying cause and severity.
Treatment Treatment involves addressing the underlying cause and may include:
Diuretics to remove excess fluid
Medications to improve heart function (for cardiogenic pulmonary edema)
Supplemental oxygen or mechanical ventilation
Treating underlying conditions such as infections or high altitude exposure
8. Pulmonary Fibrosis

Pulmonary fibrosis is the thickening and scarring of lung tissue, leading to reduced oxygen absorption. Causes include chronic exposure to environmental pollutants, infections, genetic factors, and autoimmune diseases (e.g., scleroderma).
Symptoms
Shortness of breath (dyspnea)
Persistent dry cough
Fatigue
Unexplained weight loss
Aching muscles and joints
Clubbing (widening and rounding) of the fingertips or toes
Diagnosis Diagnosis involves a combination of patient history, physical examination, imaging tests (chest X-rays, high-resolution CT scans), pulmonary function tests, and sometimes lung biopsy. Blood tests may be used to identify underlying autoimmune diseases.
Treatment While there is no cure for pulmonary fibrosis, treatments focus on symptom management and slowing progression:
Medications such as pirfenidone and nintedanib to slow disease progression
Oxygen therapy
Pulmonary rehabilitation
Lung transplant in severe cases
9. Pneumoconiosis
Pneumoconiosis is a lung disease caused by inhaling dust particles, such as asbestos, silica, or coal dust, leading to lung scarring. It is a type of occupational lung disease commonly seen in miners, construction workers, and industrial workers.
Symptoms:
Chronic cough
Shortness of breath
Chest tightness
Progressive loss of lung function
Diagnosis: Diagnosis involves a detailed occupational history, physical examination, chest X-rays, and CT scans. Pulmonary function tests may also be conducted to assess the extent of lung damage.
Treatment Treatment includes:
Avoiding further exposure to dust
Medications to manage symptoms, such as bronchodilators and corticosteroids
Respiratory therapies
Pulmonary rehabilitation
10. Pulmonary Arterial Hypertension (PAH)
PAH is a form of high blood pressure affecting the arteries in the lungs and the right side of the heart. It can be idiopathic, familial, or associated with other conditions such as connective tissue diseases, congenital heart disease, or chronic liver disease.
Symptoms
Breathing difficulties (dyspnea), especially during physical activities
Dizziness or fainting (syncope)
Chest pain
Fatigue
Swelling in the ankles, legs, and abdomen (edema)
Cyanosis (bluish lips and skin)
Diagnosis Diagnosis involves echocardiography, right heart catheterization, chest X-rays, and CT scans. Blood tests and pulmonary function tests may also be conducted to assess lung and heart function.
Treatment Treatment strategies include:
Medications to relax blood vessels and improve blood flow, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs
Diuretics to reduce fluid retention
Oxygen therapy
Anticoagulants to prevent blood clots
In severe cases, surgical procedures such as atrial septostomy or lung transplant
11. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene, leading to thick, sticky mucus buildup in the lungs and other organs. This results in frequent infections, respiratory issues, and digestive problems.
Symptoms
Persistent cough with thick mucus
Recurrent lung infections
Wheezing or shortness of breath
Poor growth and weight gain in children
Salty-tasting skin
Severe constipation
Frequent greasy, bulky stools
Diagnosis Diagnosis involves genetic testing, sweat chloride tests, and newborn screening. Pulmonary function tests, chest X-rays, and sputum cultures may also be conducted to assess lung health.
Treatment Management includes:
Medications to thin mucus, antibiotics to treat infections, and bronchodilators to open airways
Chest physiotherapy to clear mucus
Enzyme supplements and high-calorie diets to manage digestive issues
Newer therapies targeting the underlying genetic defect, such as CFTR modulators
12. Respiratory Distress Syndrome (RDS)
RDS primarily affects premature infants due to a lack of surfactant, a substance necessary to keep the lungs open and facilitate gas exchange. Risk factors include premature birth, maternal diabetes, and multiple births.
Symptoms
Rapid, shallow breathing
Grunting sounds while breathing
Nasal flaring
Chest retractions (pulling in of the chest muscles)
Cyanosis (bluish color of the skin and mucous membranes)
Diagnosis Diagnosis involves clinical assessment, chest X-rays, and blood gas analysis to measure oxygen and carbon dioxide levels. Prenatal tests can also help identify at-risk pregnancies.
Treatment Treatment includes:
Surfactant replacement therapy to improve lung function
Mechanical ventilation or continuous positive airway pressure (CPAP) to support breathing
Oxygen therapy
Supportive care such as fluids and nutrition
13. Sarcoidosis
Sarcoidosis is characterized by the growth of granulomas (small clusters of inflammatory cells) in the lungs and other organs, likely as an immune response to unknown triggers. The exact cause remains unclear, but genetic and environmental factors are believed to play a role.
Symptoms
Dry cough
Shortness of breath
Chest pain
Fatigue
Fever
Swollen lymph nodes
Skin lesions (e.g., erythema nodosum)
Diagnosis Diagnosis involves a combination of patient history, physical examination, chest X-rays, CT scans, and pulmonary function tests. Biopsy of affected tissues may be performed to confirm the presence of granulomas.
Treatment While sarcoidosis is often self-limiting and may resolve without treatment, severe cases may require:
Corticosteroids to reduce inflammation
Immunosuppressive medications (e.g., methotrexate, azathioprine)
Antimalarial drugs (e.g., hydroxychloroquine) for skin lesions
Regular monitoring and follow-up care to manage chronic cases
14. Asthma
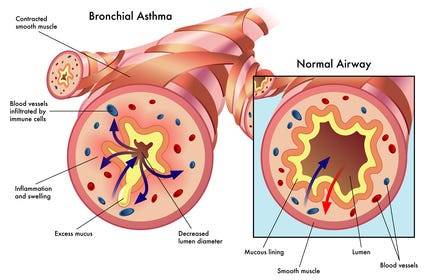
Definition and Causes: Asthma is a chronic inflammatory condition of the airways, causing episodes of wheezing, coughing, and chest tightness, often triggered by allergens, exercise, cold air, or respiratory infections. Genetic and environmental factors contribute to its development.
Symptoms
Wheezing
Shortness of breath
Chest tightness
Coughing, especially at night or early morning
Increased mucus production
Diagnosis: Diagnosis involves a detailed medical history, physical examination, and lung function tests (spirometry, peak flow measurement). Allergy testing and chest X-rays may also be conducted to identify triggers and rule out other conditions.
Treatment Management includes:
Avoiding known triggers
Inhalers (bronchodilators for quick relief, corticosteroids for long-term control)
Long-term control medications (e.g., leukotriene modifiers, long-acting beta agonists)
Immunotherapy (allergy shots) for severe allergies
Asthma action plans to manage symptoms and prevent attacks
Conclusion
Lung diseases encompass a wide range of conditions, each with distinct causes, symptoms, and treatments. Preventive measures such as avoiding smoking, reducing exposure to environmental pollutants, and timely vaccinations can significantly reduce the risk of developing many of these diseases. Early diagnosis and appropriate management are crucial in improving outcomes and quality of life for individuals affected by lung diseases. For personalized medical advice and treatment, consult with healthcare professionals.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: expertassignment46@gmail.com for professional guidance.
7 steps to writing a dissertation.

1. Choose Your Topic Wisely
Selecting a topic for your dissertation is a critical first step that sets the foundation for your entire research endeavor. This involves a comprehensive approach.
Relevance to Academic Discipline and Personal Interests
Choose a topic that aligns with your academic discipline and personal interests. This ensures that you are passionate about the subject matter, making the research process more engaging.
Consideration of Career Goals

Reflect on your career goals and aspirations. opt for a topic that not only complements your academic journey but also contributes to your professional growth. This alignment can enhance the practicality and relevance of your dissertation.
Guidance from Supervisor
Engage in regular discussions with your supervisor. Seek their guidance to refine your topic, identify potential challenges, and gain insights into the research landscape. Your supervisor’s experience can prove invaluable in shaping your research direction.
2. Check What’s Required

Understanding the requirements and expectations for your dissertation is crucial for successful completion. This step involves a detailed examination of marking criteria, module guidelines, and additional instructions:
Scrutinizing Marking Criteria
Thoroughly analyze the marking criteria provided by your educational institution. This ensures that your dissertation aligns with the assessment standards, maximizing your chances of achieving a favorable grade.
Grasping Academic Writing Expectations
Familiarize yourself with the academic writing conventions specific to your discipline. This includes understanding citation styles, formatting guidelines, and language conventions. Adhering to these expectations enhances the professionalism of your dissertation.
Word Count and Submission Details
Take note of the stipulated word count for your dissertation. Understanding the limitations ensures that your research remains concise and focused. Additionally, pay attention to submission details, such as deadlines and submission formats (online or hard copy).
Additional Components
Many dissertations require supplementary elements like a project plan, literature review, or critical reflection. Acknowledge and incorporate these components as per the provided instructions. Neglecting these elements can result in grade deductions.
3. Conduct In-Depth Research

The research phase of your dissertation involves a comprehensive exploration of existing literature to inform and support your study.
Literature Review
Conduct a thorough literature review to identify relevant sources, articles, and studies related to your chosen topic. This process allows you to understand the existing research landscape and identify gaps or areas for further exploration.
Development of Research Questions
Based on your literature review, formulate clear and concise research questions. These questions should guide the direction of your study, addressing specific aspects of the chosen topic. Articulating well-defined research questions contributes to the coherence of your dissertation.
Note-Taking and Source Organization
Systematically take notes on each source, capturing key findings, methodologies, and arguments. Organize your sources for easy reference during the writing phase. Implement a consistent method for citation and annotation to enhance traceability.
Critical Evaluation with Advisor Guidance
Engage with your advisor throughout the research process. Seek their guidance on critically evaluating the credibility and relevance of your chosen sources. A collaborative approach ensures that your research aligns with academic standards.
4. Develop a Strong Thesis Statement

The thesis statement serves as the focal point of your dissertation, encapsulating the main argument or research question. Crafting a robust thesis statement involves several considerations:
Specificity and Focus
Ensure that your thesis statement is specific and focused, avoiding broad or vague assertions. The clarity of your thesis statement sets the tone for the entire dissertation, guiding readers on the scope of your research.
Arguability
A strong thesis statement is one that is arguable. It presents a stance or perspective that can be supported or refuted through evidence. This encourages critical engagement with your research, fostering a dynamic discourse.
Realism
Consider the feasibility of your thesis statement within the allocated time and space. Ensure that your chosen topic allows for comprehensive research and analysis without exceeding practical constraints.
Feedback from Peers and Supervisor
Share your draft thesis statement with your peers and supervisor. Solicit feedback on its clarity, coherence, and alignment with your research goals. Iterative refinement based on feedback enhances the strength of your thesis statement.
5. Proofread and Edit

Proofreading and editing are integral steps to refine the quality and presentation of your dissertation. This phase goes beyond mere error correction and involves a holistic evaluation:
Thorough Proofreading
After completing the initial draft, engage in thorough proofreading. Reading your dissertation aloud can reveal nuances and errors that might be overlooked during silent reading. Pay attention to grammar, spelling, and punctuation.
Environmental Change for Fresh Perspective
Changing your environment before proofreading allows you to view your work with fresh eyes. This change in perspective facilitates the identification of structural or stylistic improvements. Consider reviewing your dissertation in a quiet, distraction-free setting.
Focused Editing
Focus on specific aspects during the editing phase, such as grammar, syntax, and coherence. Addressing one element at a time prevents overwhelming and ensures a systematic refinement of your dissertation’s overall quality.
Structural Review
Conduct a comprehensive review of your dissertation’s structure and flow. Verify that your arguments are logically organized, and ideas progress in a coherent manner. Identify any sections that require clarification or expansion.
Formatting and Referencing
Check your dissertation’s adherence to formatting guidelines, including font, font size, margins, and line spacing. Ensure that all references are accurately cited following the preferred citation style of your academic institution.
6. Seek Feedback and Finalize

Gaining feedback from your advisor or board members is a pivotal step in enhancing the robustness of your dissertation. This phase involves a collaborative approach:
Specific Feedback Requests:
When seeking feedback, be specific about the areas you want to be reviewed. Request input on overall structure, argument strength, writing clarity, or any specific concerns you may have. This targeted approach streamlines the feedback process.
Openness to Constructive Criticism
Approach feedback with an open mind, understanding that constructive criticism is aimed at improvement. Embrace suggestions for refinement, even if they challenge your initial perspectives. Incorporating diverse feedback strengthens the scholarly merit of your work.
Implementation of Feedback
Actively implement the feedback received. Revise sections based on recommendations, clarify ambiguous points, and strengthen areas identified as weak. This iterative process ensures that your dissertation undergoes continuous improvement.
7. Submit

The final submission of your dissertation requires meticulous attention to guidelines and deadlines. Proper preparation ensures a smooth submission process.
Guideline Adherence
Review the submission guidelines provided by your educational institution. Ensure that your dissertation meets all specified requirements, including formatting, additional components, and submission format (online or hard copy).
Timely Submission
Adhere to the submission deadline to avoid penalties or rejections. Plan your submission well in advance, considering the time required for any administrative processes. Late submissions may impact your academic assessment.
Submission Format
If online submission is the designated method, prepare a PDF file according to the platform’s specifications. Include any additional information, such as your student ID number or dissertation title, as required by the submission portal.
Hard Copy Submission
For institutions requiring hard copy submission, follow the specified procedures. Submit a bound copy of your dissertation to the department office, adhering to any additional requirements such as multiple copies, title page, abstract, and table of contents.
Consultation with Advisor
Before final submission, consult with your advisor to ensure that all aspects of your dissertation align with institutional expectations. Address any last-minute queries or concerns to ensure a seamless submission process.
For All your Assignments Help;
Email us at;
williamsliason@outlook.com
The Pathophysiology Of Spondylitis

Spondylitis is a comprehensive term used to describe a group of chronic inflammatory diseases that primarily affect the joints of the spine and the sacroiliac region, which includes the pelvis and lower spine. These conditions are characterized by arthritis-like symptoms and can lead to significant discomfort, reduced mobility, and other systemic complications. This detailed exploration will indulge into the nature of spondylitis, how it differs from the related condition known as spondylosis, the various types of spondylitis, diagnostic methods, treatment options, and complementary therapies.
What is Spondylitis?

Spondylitis involves inflammation of the joints, tendons, and ligaments within the spine and sacroiliac region. Tendons are connective tissues that attach muscles to bones, while ligaments connect bones to other bones. This inflammation can result in the fusion of bones (ankylosis) and the formation of new bone, leading to stiffness and reduced flexibility in the spine. In severe cases, excessive bone growth can cause significant curvature of the spine, known as kyphosis.
Spondylitis vs. Spondylosis
While both spondylitis and spondylosis cause pain in the hip and back, they are distinct conditions with different etiologies and characteristics.
Spondylitis is an autoimmune disorder where the immune system mistakenly attacks the joints, causing inflammation, bone fusion, and excessive bone formation. This condition typically develops in teenagers and young adults and can affect multiple organs and systems within the body.
Spondylosis, on the other hand, is a degenerative condition associated with aging and the natural wear and tear of the spine. It involves the degeneration of spinal joints and discs, often accompanied by the formation of bone spurs (osteophytes). Spondylosis primarily affects older individuals, with more than 85% of people over the age of 60 experiencing this condition.
Types of Spondylitis

Medical professionals categorize spondylitis using two primary classification systems: the traditional system and the newer system. The traditional system recognizes six specific types of spondylitis, whereas the newer system categorizes spondylitis into two broad types based on the affected body region.
Traditional Spondylitis Classifications:
a) Ankylosing Spondylitis (AS)
Symptoms: Ankylosing spondylitis primarily affects the spine, causing symptoms such as fatigue, chronic back pain, stiffness, and inflammation in various areas of the body, including joints and tendons. Over time, the vertebrae may fuse, leading to reduced mobility and flexibility.
Causes: The exact cause of AS is unknown, but a strong genetic association exists with the HLA-B27 gene. Approximately 90% of individuals with AS carry this gene, although not all carriers develop the disease.
b) Reactive Arthritis
Symptoms: Reactive arthritis typically presents with a triad of symptoms including arthritis (swelling and pain in joints), conjunctivitis (inflammation of the eyes with a sticky discharge), and urethritis (genital and bladder inflammation with painful urination). However, not all patients exhibit all three symptoms.
Causes: often follows a gastrointestinal infection or a sexually transmitted infection (STI). The immune system overreacts to the initial infection, leading to inflammation and joint pain. The HLA-B27 gene is also strongly linked to ReA, with 30–50% of affected individuals carrying this gene.
c) Psoriatic Arthritis (PsA)
Symptoms: Psoriatic arthritis is associated with the inflammatory skin condition psoriasis. Symptoms include dactylitis (swelling in toes and fingers), changes in nails (such as pitting), eye pain, joint pain, reduced range of motion, and fatigue. PsA typically affects people aged 30–50.
Causes: PsA often follows psoriasis, but it can also develop in individuals without skin symptoms. There is a genetic predisposition to PsA, with at least 10% of the population inheriting genes that increase susceptibility to psoriasis and PsA.
d) Enteropathic Arthritis (EnA)
Symptoms
Enteropathic arthritis is linked to inflammatory bowel diseases (IBDs) such as ulcerative colitis and Crohn’s disease. Symptoms include abdominal pain, bloody diarrhea, and joint swelling and pain.
Causes
The precise cause of EnA is unclear, but it is associated with chronic inflammation in the bowel. This inflammation may allow bacteria to penetrate the bowel wall, triggering an immune response that leads to joint inflammation. The HLA-B27 gene is also linked to EnA.
d) Juvenile Spondyloarthritis (JSpA)
Symptoms
Juvenile spondyloarthritis begins in individuals aged 16 or younger and typically affects the leg joints. Symptoms include joint pain, tenderness, and bowel inflammation.
Causes
Similar to adult spondylitis, JSpA is often associated with the HLA-B27 gene. The exact cause remains unknown, but genetic and environmental factors likely play a role.
e)Undifferentiated Spondyloarthritis (USpA)
Symptoms
USpA is characterized by a variety of symptoms that do not fit neatly into a specific rheumatoid disorder. Symptoms may include persistent lower back pain, joint pain in small and large joints, heel pain, swelling in hands and feet, general stiffness, eye inflammation, rash, urinary tract symptoms, and intestinal inflammation.
Causes
The causes of USpA are diverse and not fully understood. It encompasses a range of symptoms that do not meet the criteria for other specific types of spondylitis.
Newer Spondylitis Categorizations
Peripheral Spondyloarthritis (pSpA)
Peripheral spondyloarthritis affects joints and tendons outside the spine and sacroiliac joints, such as the hands, wrists, elbows, shoulders, knees, ankles, and feet. It includes forms of spondylitis such as reactive arthritis, enteropathic arthritis, and undifferentiated arthritis.
2. Axial Spondyloarthritis (AxSpA)
Axial spondyloarthritis involves inflammation and pain in the pelvis and spine. This category covers a broad range of spondylitis types and includes individuals with and without sacroiliac joint fusion. AxSpA is further subdivided into non-radiographic AxSpA (without visible joint damage on X-rays) and radiographic AxSpA (visible joint damage).
Diagnosis
Diagnosing spondylitis involves abroad approach, combining physical examination, medical history, and various diagnostic tests. There is no single definitive test for spondylitis, making a comprehensive evaluation essential.
a) Physical Examination
During a physical examination, the doctor will assess the patient’s symptoms, medical history, and family history of autoimmune diseases such as psoriasis and spondyloarthritis. The examination may include evaluating joint tenderness, swelling, and range of motion.
b) Diagnostic Tests
Blood Tests: Blood tests can help identify markers of inflammation, such as elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Testing for the presence of the HLA-B27 gene can also provide valuable information, although not all individuals with spondylitis carry this gene.
Imaging Tests: Imaging techniques are crucial for diagnosing spondylitis and assessing the extent of joint and bone damage.
X-rays: X-rays can reveal changes in the spine and sacroiliac joints, such as joint fusion and bone spurs.
MRI Scans: MRI scans provide detailed images of soft tissues and can detect early signs of inflammation and joint damage that may not be visible on X-rays.
Ultrasound Scans: Ultrasound scans can be used to assess inflammation in peripheral joints and tendons.
Genetic Testing: Testing for the HLA-B27 gene can support the diagnosis, particularly in cases where clinical symptoms and imaging findings are inconclusive.
Treatment
While there is no cure for spondylitis, various treatments can help manage symptoms, reduce inflammation, and improve the patient’s quality of life. Treatment plans are often tailored to the individual’s specific symptoms and disease severity.
Medications
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs are commonly used to reduce inflammation and pain in spondylitis patients. Examples include ibuprofen and naproxen.
Corticosteroids: Corticosteroids, such as prednisone, can be prescribed for short-term use to control severe inflammation and pain.
Disease-Modifying Antirheumatic Drugs (DMARDs): DMARDs, including methotrexate and sulfasalazine, can help manage symptoms and slow disease progression in some types of spondylitis.
Biologic Agents: Biologic agents, such as tumor necrosis factor (TNF) inhibitors (e.g., adalimumab, etanercept) and interleukin-17 (IL-17) inhibitors (e.g., secukinumab), target specific components of the immune system to reduce inflammation and prevent joint damage.
Analgesics: Pain relievers, such as acetaminophen, may be used to manage pain when inflammation is not the primary issue.
Physical Therapy
Physical therapy plays a crucial role in managing spondylitis by improving and maintaining spine flexibility and overall mobility. Techniques may include:
Massage Therapy: Therapeutic massage can help reduce muscle tension, improve circulation, and alleviate pain.
Spinal Manipulation: Performed by a trained physical therapist or chiropractor, spinal manipulation can enhance mobility and reduce pain.
Exercises: Tailored exercise programs can help strengthen muscles, improve posture, and enhance flexibility. Stretching exercises are particularly beneficial for maintaining spine and joint flexibility.
Breathing Exercises: Breathing exercises are essential for individuals with ankylosing spondylitis, as the condition can affect chest expansion and respiratory function. These exercises help maintain normal lung function and prevent restrictive lung disease.
Surgery: Surgery is generally considered a last resort and is reserved for severe cases where conservative treatments have failed. Surgical options include:
Joint Replacement: For patients with severe joint damage, joint replacement surgery (e.g., hip or knee replacement) can restore function and relieve pain.
Spinal Surgery: In cases of severe spinal deformity or nerve compression, spinal surgery may be necessary to correct curvature and alleviate pressure on nerves.
Complementary Therapies
In addition to conventional treatments, complementary therapies can provide additional symptom relief and improve overall well-being. These therapies are often used alongside standard medical treatments.
Massage Therapy: Massage therapy can help reduce muscle tension, improve blood circulation, and alleviate pain and stiffness in the affected areas.
Relaxation Techniques: Techniques such as deep breathing, progressive muscle relaxation, and meditation can help manage stress and reduce pain perception.
Yoga: Yoga combines physical postures, breathing exercises, and meditation to improve flexibility, strength, and relaxation. Yoga can be particularly beneficial for maintaining spine flexibility and reducing pain.
Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the nervous system and promote natural pain relief and healing.
Cupping: Cupping is a traditional therapy that involves placing suction cups on the skin to improve blood flow and reduce muscle tension. It can be used to alleviate pain and stiffness in the back and other affected areas.
Summary
Spondylitis encompasses a range of chronic inflammatory diseases that affect the spine and sacroiliac region. It is characterized by autoimmune-driven inflammation, leading to joint pain, stiffness, and potential bone fusion. Spondylitis is distinct from spondylosis, a degenerative condition associated with aging. Medical professionals classify spondylitis into various types based on symptoms and affected body regions. Diagnosis involves a combination of physical examination, medical history, blood tests, imaging, and genetic testing. While there is no cure, treatments such as medications, physical therapy, and complementary therapies can help manage symptoms and improve the quality of life for those affected by spondylitis. By understanding the nature of spondylitis and the available management strategies, individuals can better navigate their condition and maintain an active, fulfilling life.
Medical students and healthcare professionals need to stay informed about the latest advancements in diagnosing and treating spondylitis. Continuous education and expert guidance are crucial for managing these complex conditions. For additional support with challenging medical units, clinical studies, research projects, assignments, and exam preparation, Expert Academic Assignment Help offers professional resources and online classes. For personalized assistance, contact expertassignment46@gmail.com Accessing expert guidance can significantly enhance your understanding and proficiency in medical education.