Study Tips For University Students
Study Tips For University Students

Introduction
Achieving success as a university student involves mastering effective study methods, time management, and maintaining overall well-being. In this comprehensive discussion, we will major into the top 10 university study tips that can prepare students for the challenges and opportunities that university life presents.
Preview and Review Study Resources
Understanding the importance of previewing study materials before lectures.
Incorporating regular reviews to consolidate knowledge and prepare for new concepts.
Exploring advanced reading techniques for improved comprehension.
2. Customizing Your Note-Taking System
Recognizing the power of note-taking in mastering any subject.
Exploring digital and handwritten note-taking approaches.
Utilizing advanced note-taking apps for organization and efficiency.
Discussing the Cornell Method, mind mapping, and other note-taking strategies.

. Establishing a daily study routine for consistency.
Adapting study habits during holidays to balance academics and festivities.
Creating to-do lists and prioritizing tasks for optimal time management.
Examining time-blocking techniques for enhanced productivity.
4. Setting Goals and Focusing
Setting specific, realistic goals to enhance study sessions.
Avoiding multitasking and using goal-oriented apps for focus.
Exploring the concept of SMART goals in academic settings.

Recognizing the importance of breaks for maintaining attention levels.
Introducing the Pomodoro Technique for efficient study sessions.
Discussing mindfulness and relaxation techniques during breaks.
6. Creating a Suitable Studying Environment
Maximizing productivity by minimizing distractions.
Establishing environmental cues to signal study mode.
Exploring the impact of ergonomics on study efficiency.

Motivating regular study habits by incorporating rewards.
Breaking down tasks into smaller goals for increased control.
Exploring the psychology of rewards and their impact on motivation.
8. Utilizing Study Groups
. Exploring the benefits of studying in groups.
Ensuring structured and accountable study group dynamics.
Discussing effective group communication and collaboration.
9 .Seeking Help When Needed
Overcoming the reluctance to ask for help.
Recognizing the importance of seeking assistance for academic success.
Discussing the role of tutors, mentors, and academic resources.

Understanding the impact of sleep and exercise on academic performance.
Incorporating a consistent sleep schedule and daily exercise routine.
Discussing the link between physical well-being and cognitive function.
Conclusion
In conclusion, success in university requires a holistic approach that encompasses effective study techniques, time management, and self-care. By implementing these ten study tips and delving into related topics, students can not only excel academically but also enhance their overall university experience. Balancing academic commitments with a healthy lifestyle is crucial for long-term success, and these strategies provide a foundation for thriving in the challenging yet rewarding university environment.
We wish you all the best in your University study program.
Incase of any challenges or need assistance and guidance during the process, do not hesitate ,just;
Email us at; williamsassignmenthelpfredrick@gmail.com
More Posts from Expertacademicassignmenthelp and Others

Thank you @kitteena and everyone who got me to 5 reblogs!
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com
How Does The Drug Got Excreted / Eliminated From The Body?

Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: expertassignment46@gmail.com
Your excellence our pride.
10 Tips on How to Study for Medical School

Mastering Time Management
Embarking on the journey of medical school introduces a myriad of challenges, chief among them being the effective management of time. Recognizing the seemingly limited hours in a day, the key lies in adopting a day-by-day approach and establishing a routine that fosters success. Prioritizing tasks, meticulous planning, and incorporating strategic breaks are integral components that enhance both confidence and efficacy in the demanding role of a medical student.
Thorough preparation before the commencement of each class is an impactful strategy. Engaging in pre-class reading enables students to gain a deeper grasp of the lecture’s organization, allowing them to focus on pivotal concepts. This not only facilitates active participation but also positions students to ask informed questions, showcasing a genuine interest and mastery of the subject matter.
2. The Power of Note-Taking
In the intricate landscape of medical school, note-taking emerges as a linchpin for success. Beyond the lecture hall, effective note-taking during readings serves as a powerful tool for managing the deluge of information. Organizing this wealth of material systematically, capturing the essence of each concept, transforms these notes into a potent study guide.
Taking notes not only aids in the recording of information but also serves as an invaluable aid in understanding complex material. The act of transcribing information in one’s own words, essentially explaining concepts to oneself, deepens comprehension and acts as a reinforcing mechanism for challenging subjects.
3. Continuous Learning
Unlike the strategies that sufficed during undergraduate studies, medical school demands a paradigm shift toward continuous learning. The vast curriculum and extensive memorization requirements necessitate a commitment to ongoing, consistent learning. Regular self-testing, routine revisiting of material, and the cultivation of ‘clinical pearls’ — succinct, significant pieces of information — become daily habits that fortify a student’s knowledge base.
The concept of ‘clinical pearls’ transcends the classroom, extending into the professional realm of practicing physicians. As future doctors, adopting these daily learning practices positions students on the trajectory of lifelong learning, a cornerstone of the medical profession.
4. Memory Tricks and Mnemonics
Navigating the labyrinthine landscape of medical knowledge requires innovative memory aids, and mnemonic devices emerge as indispensable allies. Acronyms, memorization phrases, and even the melodic arrangement of information to music serve as effective tools for enhancing memory retention.
Physicians themselves often rely on these mnemonic devices, creating a lexicon of memorable acronyms and phrases that enable them to recall critical information effortlessly. From recalling the signs of a stroke to understanding what passes through the placenta, these memory tricks transform the daunting task of memorization into an engaging and effective learning experience.
5. Know Your Study Sweet Zone
Understanding one’s individual learning strengths is a cornerstone of effective study strategies. Every student possesses a unique learning style, whether through auditory, visual, or other methods. Tailoring study techniques to align with these strengths enhances the overall learning experience and optimizes the absorption of complex medical concepts.
For auditory learners, exploring options such as recording lectures for later review over headphones can be particularly beneficial. On the other hand, visual learners may find sketching and diagramming organ systems to be powerful aids for comprehension. The key to success lies in identifying one’s strengths and leveraging them in the pursuit of medical knowledge.
6. Create Your Study Sanctuary
Amidst the bustling demands of medical school, the creation of a dedicated study space, a ‘study palace,’ becomes imperative. This sanctuary, a space entirely under your control, serves as an oasis of concentration free from distractions. Whether it’s a private room at home or a cubicle in the library, this designated study space becomes the canvas for focused and uninterrupted learning.
Minimizing electronic distractions within this study sanctuary is crucial. In an era of constant connectivity, silencing notifications and carving out dedicated time for focused learning contributes significantly to concentration and overall academic success.
7. Seek Help When Needed
Navigating the complexities of medical school inevitably brings moments of challenge and confusion. During these times, the importance of seeking help cannot be overstated. Whether turning to peers, instructors, or professors, recognizing the need for assistance is a strength, not a weakness.
Approaching professors with questions or seeking clarification on unclear concepts is a proactive step toward academic success. Instructors are not only well-equipped to provide guidance but also appreciate students who show initiative in their learning journey. Additionally, post-exam meetings with professors offer invaluable opportunities for deeper insights, clarification, and personalized study techniques.
8. Form Study Groups
The friendships forged in medical school extend beyond mere camaraderie; they become a cornerstone of academic support. The intensity of studying in medical school is a shared experience among peers. Forming study groups not only provides mutual support but also enhances collaborative learning.
Teaching concepts to fellow students within these study groups serves a dual purpose. Not only does it enhance your own understanding of a concept, but it also creates a dynamic and engaging learning environment. As you collectively navigate the challenges of medical school, the bonds formed in these study groups can last a lifetime.
9. Get Quality Sleep
Pulling an all-nighter to study at the last minute is only going to hurt you in the long run. Your brain needs sleep to retain all the information you’re reviewing. Getting enough sleep each night and keeping a fairly regular schedule is vital to feeling and performing your best.
10. Stay Encouraged
You may be accustomed to school success coming easily, but medical school challenges even the brightest students. No matter how challenging the courses, don’t give up. Remember why you started this journey in the first place!
For Instant Health Science Assignment Help Email: williamsliason@outlook.com
Medical microbiology


A clinical or medical microbiologist, typically with a Bachelor’s or Master’s degree in Microbiology and sometimes a Ph.D. in life sciences, studies the characteristics of pathogens, their transmission modes, and mechanisms of infection. They play a vital role in providing identification of pathogens, suggesting treatment options, and contributing to the development of health practices.

The historical milestones in medical microbiology include Anton van Leeuwenhoek’s observations of microorganisms in 1676, Edward Jenner’s development of the smallpox vaccine in 1796, and Louis Pasteur’s work on vaccines and pasteurization in 1857. Robert Koch’s germ theory and postulates in the late 19th century were pivotal. The Gram stain, developed by Hans Christian Gram in 1884, revolutionized bacterial identification.

Infectious diseases, including bacterial, viral, parasitic, and fungal, are commonly treated in medical microbiology. Diagnostic tests involve microbial culture, microscopy, biochemical tests, and genotyping. Microbiological culture isolates pathogens in the laboratory, while microscopy provides detailed observations. Biochemical tests and serological methods aid in identifying infectious agents.

However, the rise of antibiotic resistance poses a significant challenge. Medical microbiologists must consider the specificity and effectiveness of antimicrobial drugs, as well as the presence of resistant strains. Phage therapy, an alternative to antibiotics, is being explored to combat antimicrobial resistance.
In conclusion, medical microbiology is a dynamic field that not only diagnoses and treats diseases but also explores the benefits of microbes for human health. With historical milestones and continuous advancements, this field plays a crucial role in shaping healthcare practices and combating infectious diseases.
Wishing you all the best in pursuing your studies in Medical Bacteriology. It involves a lot of detailed focus on the causative agents of diseases.
In case of any challenges or if you’re looking for guidance during the study period, do not hesitate to;
Email us at;williamsassignmenthelpfredrick@mail.com
How Does The Brain Work?

The brain stands as a marvel of biological engineering, Composing of a multitude of bodily functions ranging from cognition and memory to emotions and sensory perception. Together with the spinal cord, it constitutes the central nervous system (CNS), the command center of the human body.
Composition of the Brain

Weighing approximately 3 pounds in adults, the brain’s main structure comprises about 60% fat, interspersed with water, protein, carbohydrates, and salts. Unlike muscles, it houses a complex network of blood vessels and nerves, including neurons and glial cells.
a) Gray and White Matter
Within the central nervous system, gray matter and white matter occupies distinct regions. In the brain, gray matter forms the outer layer, rich in neuron somas, while white matter constitutes the inner section, primarily composed of axons unsheathed in myelin. Conversely, in the spinal cord, this arrangement is reversed.
b) Brain Functionality
The brain operates by transmitting and receiving chemical and electrical signals throughout the body. These signals regulate a myriad of processes, with the brain disseminating each input. Some signals remain confined within the brain, while others traverse the spinal cord and nerves, disseminating information across the body’s expanse. This composes neural network relies on billions of interconnected neurons.
Major Brain Regions and Their Functions

1.Cerebrum
Dominating the brain’s landscape, the cerebrum encompasses the cerebral cortex and underlying white matter. It governs a spectrum of functions, including motor coordination, temperature regulation, language processing, emotional regulation, and sensory perception.
2. Brainstem
Serving as the bridge between the cerebrum and spinal cord, the brainstem comprises the midbrain, pons, and medulla. It regulates vital autonomic functions such as heart rate, breathing, and reflexive responses.
3. Cerebellum
Nestled at the posterior aspect of the brain, the cerebellum coordinates voluntary muscle movements, posture, balance, and motor learning.
Brain Coverings

a) Meninges
Three layers of protective membranes, collectively known as meninges, enshroud the brain and spinal cord. These layers — dura mater, arachnoid mater, and pia mater — shield the delicate neural tissue from physical trauma and infection.
b) Lobes of the Brain
Each hemisphere of the brain comprises four lobes, each harboring distinct functional domains:
Frontal Lobe: Governing executive functions, motor control, and higher cognitive processes.
Parietal Lobe: Integrating sensory information, spatial awareness, and perception of pain and touch.
Occipital Lobe: Specialized for visual processing and perception.
Temporal Lobe: Involved in auditory processing, language comprehension, and memory consolidation.
Deeper Brain Structures
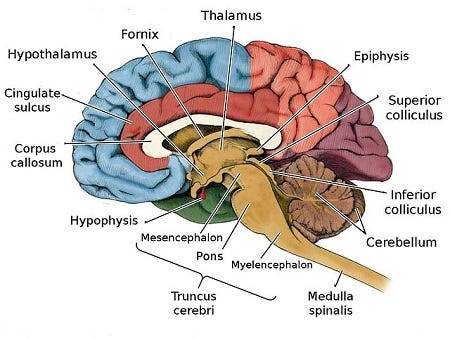
These encompass important structures such as the pituitary gland, hypothalamus, amygdala, hippocampus, and pineal gland, orchestrating hormone secretion, emotional regulation, memory consolidation, and circadian rhythms.
Blood Supply
The brain receives its oxygenated blood supply through the vertebral and carotid arteries, ensuring adequate perfusion of neural tissue. The main network of blood vessels, including the Circle of Willis, safeguards against ischemic insults and facilitates intraarterial communication.
Cranial Nerves

The twelve pairs of cranial nerves, originating from the brainstem, mediate a diverse array of sensory and motor functions, encompassing olfaction, vision, facial expression, and auditory perception.
Comprehending the anatomy and functionality of the brain fosters a deeper appreciation of its complexity and facilitates advances in neuroscientific research and therapeutic interventions aimed at diminishing neurological disorders.
Understanding the detailed anatomy and functionality of the brain is crucial for medical students embarking on their journey of study. Expert Academic Assignment Help offers invaluable assistance in navigating the complexities of neuroscience and related subjects. By leveraging expert guidance and support, students can excel in their medical education and contribute to advancements in the field of Medicine. Email us at expertassignment46@gmail.com to embark on your path to scholarly excellence and professional competency.

Thank you @expertacademicassignmenthelp and everyone who got me to 10 reblogs!
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves a multifaceted exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
We hope this helps in improving our comprehension of the Hypertension condition. All the best in your journey in the medical field.
Incase of any challenges' and in need of professional guidance, contact;
Expert Academic Assignment Help at;
williamsassignmenthelpfredrick@gmail.com
How to Write a Case Study

The case study indulges into the ideal process of rehabilitating a semi-professional cyclist who underwent a traumatic transfemoral amputation due to a road traffic accident. This comprehensive analysis aims to shed light on the complexities of limb loss rehabilitation, emphasizing the importance of tailored interventions and evidence-based practice in optimizing outcomes for individuals facing similar challenges.
Client Characteristics

In this section, a detailed exploration of the patient’s background, lifestyle, and medical history provides crucial insights into his unique rehabilitation needs. Emphasis is placed on the impact of the accident on the patient’s physical and psychological well-being, as well as his aspirations for returning to an active lifestyle post-amputation.
The patient, a previously healthy 24-year-old male, was actively engaged in semi-professional cycling and held a physically demanding job at a bicycle shop. The road traffic accident resulted in a traumatic transfemoral amputation, significantly altering his physical capabilities and emotional state. His aspirations to return to his previous level of physical activity underscore the importance of addressing both the physical and psychological aspects of his rehabilitation journey.
Examination Findings
A thorough examination is conducted to assess the patient’s physical condition and identify areas of impairment resulting from the amputation. Objective measurements, including strength assessments and gait analysis, complement subjective reports of phantom limb pain and functional limitations, forming the basis for the subsequent formulation of a clinical hypothesis.
The examination reveals significant impairments in strength and mobility, as well as the presence of phantom limb pain, which negatively impacts the patient’s daily life and rehabilitation progress. These findings highlight the need for a comprehensive treatment approach that addresses both the physical and psychological aspects of the patient’s condition.
Clinical Hypothesis/Impression

Drawing on current research and clinical expertise, the clinical hypothesis focuses on addressing the patient’s complex pain experience and psychological distress following the amputation. The identification of neuropathic pain mechanisms and the potential efficacy of interventions such as mirror therapy and mental imagery inform the development of a tailored treatment plan aimed at promoting pain relief and enhancing functional recovery.
The clinical hypothesis highlights the importance of addressing the underlying causes of the patient’s pain and implementing evidence-based interventions to optimize his rehabilitation outcomes. By targeting both the physical and psychological aspects of his condition, the treatment plan aims to improve the patient’s overall quality of life and facilitate his successful return to daily activities.
Intervention
The intervention plan is majorly crafted to address the patient’s unique rehabilitation goals and challenges. A multi-disciplinary approach, incorporating pharmacological interventions, prosthetic care, and psychological support, is implemented to optimize outcomes and empower the patient in his journey towards recovery. Detailed descriptions of specific treatment modalities and their rationale are provided, highlighting the importance of individualized care and ongoing monitoring throughout the rehabilitation process.
The intervention plan includes a combination of pharmacological management, prosthetic fitting and training, and psychological support to address the patient’s physical and psychological needs. Each component of the plan is tailored to the patient’s specific goals and challenges, with regular monitoring and adjustments made to ensure optimal outcomes.
Outcome
Objective measures are used to track the patient’s progress and evaluate the effectiveness of the intervention plan. Significant improvements in pain management, functional mobility, and quality of life are observed over the course of treatment, with particular emphasis on the transformative impact of mirror therapy on the patient’s pain experience and overall well-being. The importance of ongoing follow-up and support is emphasized as integral to maintaining long-term gains and facilitating the patient’s successful reintegration into daily activities.
The patient demonstrates significant improvements in pain management, functional mobility, and overall quality of life following the implementation of the intervention plan. Objective measures, including pain intensity ratings and functional assessments, demonstrate tangible improvements in the patient’s physical and psychological well-being, highlighting the effectiveness of the multi-disciplinary approach employed in his rehabilitation.
Discussion
A comprehensive discussion examines the broader implications of the case study for physiotherapy practice, highlighting the importance of holistic rehabilitation approaches that address the complex interplay of physical, psychological, and social factors in individuals with limb loss. Key lessons learned from the case study, including the value of evidence-based practice and the need for ongoing collaboration between healthcare professionals, are discussed in relation to optimizing outcomes and promoting patient-centered care.
The discussion explores the broader implications of the case study for physiotherapy practice, emphasizing the importance of adopting a holistic approach to rehabilitation that addresses the complex needs of individuals with limb loss. By integrating evidence-based interventions and fostering interdisciplinary collaboration, healthcare professionals can enhance the effectiveness of rehabilitation interventions and improve outcomes for patients with limb loss.
Conclusion
In conclusion, the extended case study provides a detailed exploration of the rehabilitation journey of a semi-professional cyclist following a traumatic limb amputation. Through a comprehensive analysis of client characteristics, examination findings, intervention strategies, and outcomes, valuable insights are gained into the complexities of limb loss rehabilitation and the importance of personalized, evidence-based care in achieving optimal outcomes for individuals facing similar challenges.
The case study underscores the importance of adopting a holistic approach to rehabilitation that addresses the physical, psychological, and social aspects of limb loss by focusing on interventions to the unique needs of each patient and fostering interdisciplinary collaboration, healthcare professionals can optimize outcomes and improve the quality of life for individuals with limb loss.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
How Can You Make Your Assignment Better?

Crafting high-quality assignments is a fundamental aspect of academic success, requiring a strategic approach and attention to detail. Let’s involve into a detailed discussion on each of the provided guidelines for improving assignment writing skills:
1. Understanding the Assignment Prompt
The assignment prompt serves as a roadmap for your task, outlining the expectations and requirements set by your instructor. Without a clear understanding of the prompt, you risk deviating from the intended focus and missing key elements necessary for a successful assignment. To ensure comprehension, it’s essential to break down the prompt into manageable components, identify keywords, and clarify any uncertainties with your instructor. By mastering this step, you lay a solid foundation for the rest of your assignment.
2. Thorough Research

Research is the backbone of academic writing, providing the necessary evidence and context to support your arguments. However, effective research goes beyond a simple gathering of information; it involves critical evaluation and synthesis of diverse sources to construct a coherent narrative. By consulting a variety of reputable sources, such as academic journals, books, and credible websites, you can deepen your understanding of the topic and bolster the credibility of your arguments. Additionally, employing advanced search strategies, such as Boolean operators and database filters, can streamline the research process and yield more targeted results.
3. Clear Thesis Statement
The thesis statement serves as the central claim or argument of your assignment, guiding the direction of your analysis and providing a roadmap for your readers. A strong thesis statement is concise, specific, and debatable, offering a clear stance on the topic while leaving room for exploration and interpretation. To craft an effective thesis statement, it’s crucial to conduct preliminary research, identify key themes or patterns, and articulate a focused argument that aligns with the scope of your assignment. By establishing a solid thesis statement early on, you can maintain clarity and coherence throughout your writing process.
4. Creating an Outline

An outline is a roadmap that organizes your ideas and structures your assignment in a logical sequence. By outlining the main points, arguments, and supporting evidence, you can ensure that your assignment flows cohesively and addresses all necessary components. Additionally, an outline provides a visual representation of your assignment’s structure, allowing you to identify gaps in your argumentation or areas that require further development. To create an effective outline, consider using a hierarchical format, such as Roman numerals or bullet points, to delineate the main sections and subtopics of your assignment. By investing time in outlining, you can streamline the writing process and produce a more polished final product.
5. Adhering to Formatting Guidelines
Formatting guidelines dictate the presentation and organization of your assignment, ensuring consistency and professionalism across academic work. While formatting requirements may vary depending on the discipline or institution, common elements include font size, margins, spacing, and citation style. By familiarizing yourself with the specific formatting guidelines provided by your instructor or institution, you can avoid unnecessary errors and present your work in a standardized format. Additionally, utilizing formatting tools or templates, such as Microsoft Word’s built-in styles or citation managers like EndNote, can simplify the formatting process and save time during document preparation.
6. Writing Clear and Concise Sentences
Clarity is paramount in academic writing, as it enhances comprehension and facilitates effective communication of ideas. Clear and concise sentences convey information efficiently, minimizing ambiguity and maximizing impact. To achieve clarity, it’s essential to use precise language, avoid unnecessary jargon or complex syntax, and structure sentences logically. Additionally, incorporating transition words and phrases, such as “however,” “therefore,” and “in addition,” can enhance coherence and flow between ideas. By prioritizing clarity and conciseness in your writing, you can engage your readers more effectively and convey your arguments with precision.
7. Supporting Arguments with Evidence

Evidence serves as the backbone of persuasive writing, providing support for your claims and lending credibility to your arguments. Whether in the form of empirical data, scholarly research, or real-world examples, evidence should be relevant, reliable, and effectively integrated into your assignment. To effectively support your arguments with evidence, it’s essential to critically evaluate sources, consider alternative perspectives, and provide sufficient context for interpretation. Additionally, employing proper citation techniques, such as direct quotations or paraphrasing, ensures academic integrity and acknowledges the contributions of other scholars. By prioritizing evidence-based reasoning, you can strengthen the persuasiveness of your arguments and demonstrate your mastery of the subject matter.
8. Proper Source Citation
Accurate citation of sources is essential for maintaining academic integrity and avoiding plagiarism. Proper citation acknowledges the contributions of other scholars, provides context for your arguments, and allows readers to locate the original source material. Depending on the citation style specified by your instructor or institution, you may be required to include in-text citations, footnotes, or a bibliography/reference list. To ensure proper source citation, it’s important to familiarize yourself with the conventions of your chosen citation style and apply them consistently throughout your assignment. Additionally, utilizing citation management tools, such as Zotero, Mendeley, can streamline the citation process and minimize errors.
9. Revision and Editing

Revision and editing are essential stages of the writing process, allowing you to refine your ideas, clarify your arguments, and improve the overall quality of your assignment. Revision involves reviewing your work from a macro perspective, focusing on content, structure, and argumentation, while editing focuses on micro-level elements such as grammar, punctuation, and style. To effectively revise and edit your assignment, it’s helpful to approach the task systematically, taking breaks between drafts to gain fresh perspective and utilizing feedback from peers, instructors, or writing tutors. Additionally, employing self-editing techniques, such as reading your work aloud or using grammar-checking software, can help identify errors and inconsistencies that may have been overlooked.
9. Careful Proofreading

Proofreading is the final step before submission, ensuring that your assignment is free from errors and polished to perfection. While it may seem tedious, careful proofreading is essential for maintaining professionalism and credibility in academic writing. To effectively proofread your assignment, it’s helpful to approach the task methodically, focusing on one aspect at a time (e.g., spelling, grammar, punctuation) and utilizing tools such as spell-checkers or style guides for assistance. Additionally, seeking feedback from peers or mentors can provide valuable insights and help identify areas for improvement. By dedicating time and attention to proofreading, you can ensure that your assignment meets the highest standards of quality and excellence.
Incorporating these guidelines into your writing process can significantly enhance the quality of your assignments and contribute to your academic success. By prioritizing clarity, coherence, and evidence-based reasoning, you can effectively communicate your ideas, engage your readers, and achieve your academic goals. Additionally, seeking assistance from resources such as Expert Academic Assignment Help can provide valuable support and guidance, helping you navigate complex assignments and overcome challenges along the way. Remember, improvement takes time and effort, but with dedication and practice, you can elevate your assignment writing skills to new heights and achieve academic excellence.
Incase of need for any guidance or facing challenges during the study period, just email: expertassignment46@gmail.com
Pneumonia In Children And Adults

Introduction
Pneumonia stands as a prevalent respiratory infection, exerting a significant burden on global public health. Its impact extends beyond mere morbidity, contributing to substantial healthcare costs and socioeconomic consequences. This discussion aims to elucidate the general nature of pneumonia, encompassing its pathophysiology, clinical presentation, diagnostic modalities, treatment strategies, complications, and preventive measures. By indulging into these factors, we aim to provide a better understanding of pneumonia’s complexity and underscore the importance of timely recognition and management.
Pathophysiology

Pneumonia ensues from the infiltration of infectious agents, including bacteria, viruses, fungi, and less commonly, parasites, into the lower respiratory tract. Upon inhalation or aspiration of these pathogens, they gain access to the alveoli, where they incite an inflammatory response. This inflammatory cascade triggers the release of pro-inflammatory cytokines and chemokines, recruiting immune cells to the site of infection. Neutrophils, macrophages, and lymphocytes converge to eradicate the invading pathogens, leading to the characteristic consolidation and exudate formation within the affected lung tissue. As the infection progresses, alveolar edema, impaired gas exchange, and parenchymal damage ensue, culminating in the clinical manifestations of pneumonia.
Clinical Presentation

The clinical presentation of pneumonia encompasses a spectrum of symptoms, ranging from mild respiratory complaints to life-threatening respiratory failure. Common symptoms include cough, productive sputum production, fever, chills, pleuritic chest pain, dyspnea, tachypnea, and systemic manifestations such as malaise and fatigue. The severity of symptoms varies depending on factors such as the underlying pathogen, the extent of lung involvement, the host’s immune status, and comorbidities. In pediatric populations, pneumonia may present with nonspecific symptoms such as feeding difficulties, lethargy, and irritability, posing diagnostic challenges. Conversely, elderly individuals may exhibit atypical presentations characterized by confusion, hypothermia, and exacerbations of underlying chronic conditions.
Diagnostic Modalities

The diagnosis of pneumonia hinges on a comprehensive clinical assessment, augmented by various diagnostic modalities to confirm the presence of pulmonary infection and reveal its etiology. A thorough history and physical examination provide invaluable insights into the patient’s symptomatology, risk factors, and clinical trajectory. Symptomatic findings such as crackles, wheezes, and diminished breath sounds may aid in localizing the site of infection and assessing disease severity. Radiographic imaging, notably chest X-rays and computed tomography (CT) scans, serves as the cornerstone of pneumonia diagnosis, revealing characteristic radiographic findings such as airspace opacities, lobar consolidation, and interstitial infiltrates. Laboratory investigations, including complete blood count (CBC), C-reactive protein (CRP), and procalcitonin levels, may corroborate the clinical suspicion of pneumonia and guide therapeutic decisions. Additionally, microbiological testing of respiratory specimens through techniques such as sputum culture, blood cultures, and polymerase chain reaction (PCR) assays facilitates pathogen identification and antimicrobial susceptibility testing, thereby informing targeted therapy.
Treatment Strategies

The management of pneumonia hinges on prompt initiation of empiric antimicrobial therapy tailored to the likely causative pathogen(s) and disease severity. Antibiotics represent the mainstay of treatment for bacterial pneumonia, with the choice of agent dictated by factors such as local antimicrobial resistance patterns, patient age, comorbidities, and recent antibiotic exposure. Commonly prescribed antibiotics include beta-lactam agents (e.g., penicillins, cephalosporins), macrolides, fluoroquinolones, and combination regimens for severe or healthcare-associated infections. Conversely, viral pneumonia necessitates supportive care measures, given the limited efficacy of antiviral agents in most cases. Influenza-associated pneumonia may benefit from neuraminidase inhibitors such as oseltamivir, while respiratory syncytial virus (RSV) pneumonia may warrant ribavirin therapy in select cases. Adjunctive therapies such as oxygen supplementation, bronchodilators, and corticosteroids may mitigate respiratory distress and improve clinical outcomes, particularly in severe or hypoxemic patients. The duration of antimicrobial therapy varies depending on factors such as the causative pathogen, clinical response, radiographic resolution, and the presence of complications. Close monitoring of clinical parameters and serial imaging studies guide the decision-making process, enabling clinicians to tailor therapy to individual patient needs.
Complications

Pneumonia harbors the potential for various complications, ranging from mild to life-threatening sequelae, necessitating vigilant monitoring and timely intervention. Common complications include pleural effusion, empyema, lung abscess, respiratory failure, septic shock, and acute respiratory distress syndrome (ARDS). Pleural effusion denotes the accumulation of fluid within the pleural space, secondary to inflammation or impaired lymphatic drainage, manifesting as dyspnea, pleuritic chest pain, and dullness to percussion on physical examination. Empyema represents a purulent collection within the pleural cavity, often complicating bacterial pneumonia and necessitating drainage via thoracentesis or chest tube placement. Lung abscesses manifest as circumscribed cavities containing necrotic debris and pus within the lung parenchyma, triggered by persistent fever, productive cough, and hemoptysis. Respiratory failure ensues from impaired gas exchange and alveolar hypoventilation, caused by worsening hypoxemia, hypercapnia, and respiratory acidosis, necessitating mechanical ventilation and intensive care support. Septic shock represents a life-threatening complication of severe pneumonia, characterized by systemic inflammatory response syndrome (SIRS) and end-organ dysfunction, requiring aggressive fluid resuscitation, vasopressor therapy, and broad-spectrum antibiotics. ARDS denotes a severe form of acute lung injury, characterized by diffuse alveolar damage, refractory hypoxemia, and bilateral infiltrates on chest imaging, necessitating lung-protective ventilation and supportive care in the intensive care unit (ICU). The occurrence of complications portends a poor prognosis and underscores the need for early recognition and intervention to mitigate adverse outcomes.
Preventive Measures

Preventing pneumonia entails a broad approach encompassing vaccination, infection control measures, and health promotion strategies aimed at reducing the risk of respiratory infections and their sequelae. Vaccination stands as a cornerstone of pneumonia prevention, targeting common bacterial and viral pathogens implicated in pneumonia pathogenesis. Vaccines such as the pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) confer protection against Streptococcus pneumoniae, the leading bacterial cause of pneumonia, particularly in high-risk populations such as young children, older adults, and immunocompromised individuals. Influenza vaccination remains paramount in mitigating influenza-associated pneumonia and reducing disease transmission, underscoring the importance of annual vaccination campaigns targeting vulnerable populations. Additionally, adherence to infection control measures, including hand hygiene, respiratory etiquette, and environmental sanitation, plays a pivotal role in reducing the spread of respiratory pathogens in healthcare settings and the community at large. Health promotion efforts aimed at smoking cessation, optimizing nutrition, and addressing underlying comorbidities such as chronic obstructive pulmonary disease (COPD), asthma, and immunodeficiency bolster immune resilience and mitigate pneumonia risk. Furthermore, early identification and management of predisposing factors such as malnutrition, homelessness, and overcrowded living conditions attenuate pneumonia susceptibility and enhance overall health outcomes.
Conclusion
In conclusion, pneumonia emerges as a formidable respiratory infection, posing significant challenges to global public health. Its diverse etiology, clinical manifestations, diagnostic modalities, treatment modalities, complications, and preventive measures underscore the nature of pneumonia management. Timely recognition and intervention are imperative in mitigating the morbidity and mortality associated with pneumonia, necessitating a collaborative approach among healthcare providers, public health authorities, and policymakers. By fostering a comprehensive understanding of pneumonia’s manifest and implementing evidence-based strategies, we can strive towards reducing its burden and improving patient outcomes. Through ongoing research, education, and advocacy efforts, we can envision a future where pneumonia-related morbidity and mortality are substantially diminished, paving the way for enhanced respiratory health and well-being worldwide.
In managing pneumonia, compassion, empathy, and a holistic approach are essential alongside clinical expertise. Striving for excellence in knowledge and practice allows us to enhance respiratory medicine and patient outcomes.
As we address pneumonia and broader cardiovascular health complexities, let’s remain committed to optimal patient care. Together, we can impact lives positively and foster a healthier future.
Email expertassignment46@gmail.com to discover how we can support your academic and professional goals. Wishing you ongoing success in your medical journey.
Digestive System

The digestive system is a marvel of biological engineering, orchestrating the journey of food through the body, from the moment it enters the mouth to its exit through the anus. This complex process involves a network of organs, each playing a crucial role in breaking down food, absorbing nutrients, and eliminating waste. In this detailed exploration, we delve into the anatomy, functions, common conditions, care practices, and the importance of seeking medical attention for digestive system issues.
Anatomy of the Digestive System
Gastrointestinal (GI) Tract:
1.Mouth:
Initiating Digestion: Salivary glands activate as the sight and scent of food trigger the digestive process.
Chewing and Mixing: Food is chewed into digestible pieces, mixed with saliva to facilitate breakdown.
Swallowing: The tongue propels the food into the throat and esophagus.
2. Esophagus:
Transportation: A muscular tube conducting food to the stomach through peristalsis.
Sphincter Function: The lower esophageal sphincter relaxes to allow food entry and contracts to prevent stomach content reflux.
3.Stomach:
Container and Mixer: A hollow organ holding and mixing food with stomach enzymes for further breakdown.
Acid Secretion: Cells in the stomach lining secrete powerful acids and enzymes crucial for digestion.
Release to Small Intestine: Processed stomach contents move to the small intestine for further digestion.
4.Small Intestine:
Segments and Functions: Comprising the duodenum, jejunum, and ileum, each segment has distinct roles in digestion and nutrient absorption.
Enzymatic Breakdown: Pancreatic enzymes and bile from the liver aid in breaking down food.
Nutrient Absorption: The jejunum and ileum absorb nutrients into the bloodstream.
Consistency Changes: Contents transition from semi-solid to liquid as water, bile, enzymes, and mucus contribute to the process.
Biliary System:
a. pancreas:
Enzyme Secretion: Releases digestive enzymes into the duodenum to break down proteins, fats, and carbohydrates.
Insulin Production: The pancreas produces insulin, a key hormone for sugar metabolism.
b. Liver:
Nutrient Processing: Processes nutrients absorbed by the small intestine.
Bile Production: Secretes bile into the small intestine, aiding in fat digestion and vitamin absorption.
Detoxification: Acts as the body’s chemical “factory,” detoxifying harmful substances.
c. Gallbladder:
Bile Storage: Stores and concentrates bile from the liver.
Release into Duodenum: Releases bile into the duodenum to assist in fat absorption.
Large Intestine (Colon):
Colon:
Waste Processing: Responsible for transforming waste into a convenient form for bowel movements.
Peristalsis: Propels stool through the colon, removing water and transitioning it from a liquid to a solid state.
Storage and Elimination: Stool is stored in the sigmoid colon until mass movements propel it into the rectum for elimination.
Rectum:
Chamber Function: A straight chamber connecting the colon to the anus.
Signaling and Holding: Signals the brain about stool presence and holds stool until evacuation.
Anus:
Final Elimination: The last part of the digestive tract, consisting of pelvic floor muscles and sphincters.
Sphincter Control: Surrounding sphincter muscles control stool release, preventing involuntary bowel movements.
Conditions and Disorders
Digestive system health can be affected by a spectrum of conditions, ranging from temporary issues to chronic diseases:
Temporary Conditions:
Constipation:
Frequency and Characteristics: Reduced bowel movements with dry and hard stool.
Difficulty and Pain: Straining during bowel movements, leading to discomfort.
2.Diarrhea:
Loose and Watery Stool: Abnormal stool consistency often caused by various factors.
Potential Causes: Bacterial infections, dietary issues, or unknown triggers.
3.Heartburn:
Misleading Name: Despite the name, heartburn is a digestive issue.
Acidic Backflow: Occurs when stomach acids move up the esophagus, causing discomfort in the chest.
4.Hemorrhoids:
Swollen Veins: Enlarged veins inside and outside the anus and rectum.
Symptoms: Pain, discomfort, and rectal bleeding.
5.Stomach Flu (Gastroenteritis):
Viral Infection: Infection of the stomach and upper part of the small intestine.
Duration: Typically lasts less than a week.
6.Ulcers:
Sore Development: Sores on the lining of the esophagus, stomach, or small intestine.
Causes: Helicobacter pylori infection and prolonged use of anti-inflammatory drugs.
7.Gallstones:
Solid Material Formation: Small pieces formed from digestive fluid in the gallbladder.
Chronic Diseases:
GERD (Chronic Acid Reflux):
Frequent Acid Backflow: Acid-containing contents in the stomach frequently leak into the esophagus.
Symptoms: Persistent heartburn and regurgitation.
2,Irritable Bowel Syndrome (IBS):
Colon Muscle Dysfunction: Irregular contractions leading to excessive gas, abdominal pain, and cramps.
Chronic Nature: A long-term condition affecting bowel function.
3.Lactose Intolerance:
Inability to Digest Lactose: Results in digestive discomfort after consuming milk and dairy products.
Common Symptoms: Bloating, gas, and diarrhea.
4.Diverticulosis and Diverticulitis:
Colon Pockets Formation: Diverticula (pockets) in the wall of the colon.
Complications: Inflammation (diverticulitis) can occur, causing pain and infection.
5.Gastrointestinal (GI) Cancers:
Tissue and Organ Affliction: Cancers affecting the digestive system, including esophageal, gastric, colorectal, pancreatic, and liver cancers.
6.Crohn’s Disease:
Inflammatory Bowel Disease (IBD): A lifelong condition causing inflammation in the digestive tract.
7.Celiac Disease:
Autoimmune Disorder: Gluten consumption damages the small intestine.
Trigger: Found in wheat, barley, and rye.
Care Practices for Digestive Health
Maintaining a healthy digestive system involves adopting proactive lifestyle and dietary habits:
1.Hydration:
Importance of Water: Drinking water facilitates smooth food flow, preventing dehydration-related constipation.
Dehydration Consequences: Insufficient water intake can lead to dry and hard stool.
2.Fiber-Rich Diet:
Benefits of Fiber: Supports digestion and regular bowel movements.
Soluble and Insoluble Fiber: Both types contribute to digestive health.
3.Balanced Nutrition:
Fruits and Vegetables: Multiple servings daily for essential vitamins and minerals.
Whole Grains: Choosing whole grains over processed grains.
Limiting Processed Foods: Reducing intake of processed and sugary foods.
4.Probiotics:
Role of Probiotics: Supporting a healthy gut microbiome.
Post-Antibiotic Use: Especially beneficial after antibiotic treatments.
5.Mindful Eating:
Chewing and Digestion: Thorough chewing aids in proper digestion.
Eating Pace: Slower eating allows the body to signal fullness.
6.Physical Activity:
Exercise and Digestion: Physical activity and gravity aid in moving food through the digestive system.
Post-Meal Walks: Taking a walk after meals can enhance digestion.
7.Avoiding Harmful Habits:
Alcohol and Smoking: Limiting alcohol intake to prevent acid-related issues.
Smoking Cessation: Quitting smoking improves digestive symptoms.
8.Stress Management:
Stress and Digestive Issues: Association between stress and conditions like constipation, diarrhea, and IBS.
Stress Reduction Techniques: Incorporating stress-relief practices into daily life.
Seeking Medical Attention
While occasional digestive issues are common, persistent symptoms warrant attention:
When to Contact a Healthcare Provider:
Frequent Symptoms: Constipation, diarrhea, vomiting, stomach pain, excessive gas, or heartburn.
Potential Underlying Issues: Frequent occurrences may indicate a more serious digestive system problem.
2.Importance of Medical Evaluation:
Diagnostic Assessment: Identifying the cause of persistent symptoms.
Early Intervention: Timely treatment prevents potential complications.
3.Collaborative Approach:
Healthcare Professional Guidance: Seeking advice on managing and preventing digestive issues.
Individualized Care: Tailoring interventions based on the individual’s health status and conditions.
Conclusion
In conclusion, understanding the details of the digestive system provides a foundation for promoting digestive health. The collaboration of organs in the GI tract and the biliary system highlights the complexity of the digestive process. Awareness of common conditions, care practices, and the significance of seeking medical attention empowers individuals to prioritize their digestive well-being. Adopting a holistic approach that combines a healthy lifestyle, balanced nutrition, and regular medical check-ups ensures a resilient and well-functioning digestive system, contributing to overall health and vitality.
For Health Sciences Assignment Help;
Email us on;
williamsliason@outlook.com
-
 kitteena reblogged this · 1 year ago
kitteena reblogged this · 1 year ago -
 kitteena liked this · 1 year ago
kitteena liked this · 1 year ago -
 expertacademicassignmenthelp reblogged this · 1 year ago
expertacademicassignmenthelp reblogged this · 1 year ago