10 Tips On How To Study For Medical School
10 Tips on How to Study for Medical School

Mastering Time Management
Embarking on the journey of medical school introduces a myriad of challenges, chief among them being the effective management of time. Recognizing the seemingly limited hours in a day, the key lies in adopting a day-by-day approach and establishing a routine that fosters success. Prioritizing tasks, meticulous planning, and incorporating strategic breaks are integral components that enhance both confidence and efficacy in the demanding role of a medical student.
Thorough preparation before the commencement of each class is an impactful strategy. Engaging in pre-class reading enables students to gain a deeper grasp of the lecture’s organization, allowing them to focus on pivotal concepts. This not only facilitates active participation but also positions students to ask informed questions, showcasing a genuine interest and mastery of the subject matter.
2. The Power of Note-Taking
In the intricate landscape of medical school, note-taking emerges as a linchpin for success. Beyond the lecture hall, effective note-taking during readings serves as a powerful tool for managing the deluge of information. Organizing this wealth of material systematically, capturing the essence of each concept, transforms these notes into a potent study guide.
Taking notes not only aids in the recording of information but also serves as an invaluable aid in understanding complex material. The act of transcribing information in one’s own words, essentially explaining concepts to oneself, deepens comprehension and acts as a reinforcing mechanism for challenging subjects.
3. Continuous Learning
Unlike the strategies that sufficed during undergraduate studies, medical school demands a paradigm shift toward continuous learning. The vast curriculum and extensive memorization requirements necessitate a commitment to ongoing, consistent learning. Regular self-testing, routine revisiting of material, and the cultivation of ‘clinical pearls’ — succinct, significant pieces of information — become daily habits that fortify a student’s knowledge base.
The concept of ‘clinical pearls’ transcends the classroom, extending into the professional realm of practicing physicians. As future doctors, adopting these daily learning practices positions students on the trajectory of lifelong learning, a cornerstone of the medical profession.
4. Memory Tricks and Mnemonics
Navigating the labyrinthine landscape of medical knowledge requires innovative memory aids, and mnemonic devices emerge as indispensable allies. Acronyms, memorization phrases, and even the melodic arrangement of information to music serve as effective tools for enhancing memory retention.
Physicians themselves often rely on these mnemonic devices, creating a lexicon of memorable acronyms and phrases that enable them to recall critical information effortlessly. From recalling the signs of a stroke to understanding what passes through the placenta, these memory tricks transform the daunting task of memorization into an engaging and effective learning experience.
5. Know Your Study Sweet Zone
Understanding one’s individual learning strengths is a cornerstone of effective study strategies. Every student possesses a unique learning style, whether through auditory, visual, or other methods. Tailoring study techniques to align with these strengths enhances the overall learning experience and optimizes the absorption of complex medical concepts.
For auditory learners, exploring options such as recording lectures for later review over headphones can be particularly beneficial. On the other hand, visual learners may find sketching and diagramming organ systems to be powerful aids for comprehension. The key to success lies in identifying one’s strengths and leveraging them in the pursuit of medical knowledge.
6. Create Your Study Sanctuary
Amidst the bustling demands of medical school, the creation of a dedicated study space, a ‘study palace,’ becomes imperative. This sanctuary, a space entirely under your control, serves as an oasis of concentration free from distractions. Whether it’s a private room at home or a cubicle in the library, this designated study space becomes the canvas for focused and uninterrupted learning.
Minimizing electronic distractions within this study sanctuary is crucial. In an era of constant connectivity, silencing notifications and carving out dedicated time for focused learning contributes significantly to concentration and overall academic success.
7. Seek Help When Needed
Navigating the complexities of medical school inevitably brings moments of challenge and confusion. During these times, the importance of seeking help cannot be overstated. Whether turning to peers, instructors, or professors, recognizing the need for assistance is a strength, not a weakness.
Approaching professors with questions or seeking clarification on unclear concepts is a proactive step toward academic success. Instructors are not only well-equipped to provide guidance but also appreciate students who show initiative in their learning journey. Additionally, post-exam meetings with professors offer invaluable opportunities for deeper insights, clarification, and personalized study techniques.
8. Form Study Groups
The friendships forged in medical school extend beyond mere camaraderie; they become a cornerstone of academic support. The intensity of studying in medical school is a shared experience among peers. Forming study groups not only provides mutual support but also enhances collaborative learning.
Teaching concepts to fellow students within these study groups serves a dual purpose. Not only does it enhance your own understanding of a concept, but it also creates a dynamic and engaging learning environment. As you collectively navigate the challenges of medical school, the bonds formed in these study groups can last a lifetime.
9. Get Quality Sleep
Pulling an all-nighter to study at the last minute is only going to hurt you in the long run. Your brain needs sleep to retain all the information you’re reviewing. Getting enough sleep each night and keeping a fairly regular schedule is vital to feeling and performing your best.
10. Stay Encouraged
You may be accustomed to school success coming easily, but medical school challenges even the brightest students. No matter how challenging the courses, don’t give up. Remember why you started this journey in the first place!
For Instant Health Science Assignment Help Email: williamsliason@outlook.com
More Posts from Expertacademicassignmenthelp and Others
10 Common Dental Problems

Introduction
Maintaining optimal dental health is crucial not only for a winning smile but also for overall well-being. However, numerous individuals encounter common dental issues that can affect their quality of life. From tooth decay to gum disease, understanding these problems and their treatments is essential for preventing complications and preserving oral health. This comprehensive guide explores ten prevalent dental problems and outlines effective treatment options for each, empowering individuals to make informed decisions about their dental care.
1.Tooth Decay

Tooth decay, also known as dental caries, is a pervasive dental issue caused by the accumulation of plaque and the subsequent erosion of tooth enamel. This section delves into the causes, symptoms, and treatment options for tooth decay, emphasizing the importance of preventive measures such as regular brushing, flossing, and dental check-ups.
2. Gum Disease

Gingivitis and periodontitis are two stages of gum disease characterized by inflammation and bacterial infection of the gums. Exploring the risk factors, symptoms, and management strategies for gum disease sheds light on the importance of proper oral hygiene practices and professional dental interventions in preserving gum health.
3.Bad Breath

Halitosis, or bad breath, can stem from various underlying factors such as poor oral hygiene, dry mouth, and underlying medical conditions. This segment examines the causes of bad breath and highlights the significance of comprehensive dental assessments and tailored treatment plans to address this common concern effectively.
4.Sensitive Teeth

Tooth sensitivity, characterized by discomfort in response to hot, cold, or sweet stimuli, often results from enamel erosion or underlying dental issues. Delving into the potential causes and management options for sensitive teeth underscores the role of personalized dental care in alleviating discomfort and enhancing oral comfort.
5.Cracked or Broken Teeth

Cracks or fractures in teeth can result from trauma, bruxism (teeth grinding), or other factors, leading to pain and functional impairment. This section explores the diagnostic procedures and treatment modalities available for repairing cracked or broken teeth, emphasizing the importance of prompt intervention to prevent further damage.
6.Receding Gums

Receding gums, characterized by the exposure of tooth roots due to gum tissue loss, can result from various factors, including poor oral hygiene and genetic predispositions. Analyzing the causes, consequences, and treatment approaches for receding gums underscores the significance of preventive measures and professional interventions in preserving gum health.
7. Root Infection

Root infections, often resulting from untreated cavities or trauma, can lead to severe pain and dental abscesses if left untreated. This segment elucidates the diagnostic techniques and treatment options for root infections, highlighting the role of root canal therapy in alleviating symptoms and preserving tooth structure.
8. Enamel Erosion

Enamel erosion, characterized by the gradual loss of tooth enamel due to acidic and sugary dietary habits, poses significant challenges to dental health. Exploring preventive strategies and restorative treatments for enamel erosion underscores the importance of dietary modifications and proactive dental care in preserving tooth structure and function.
9. Dry Mouth

Xerostomia, or dry mouth, can result from various factors, including medication side effects and underlying medical conditions. This section examines the causes, symptoms, and management strategies for dry mouth, emphasizing the importance of hydration and lifestyle modifications in alleviating discomfort and preventing oral complications.
10. Teeth Grinding
Bruxism, characterized by involuntary teeth grinding or clenching, can lead to tooth wear, jaw pain, and headaches. Exploring the underlying causes and treatment options for bruxism underscores the importance of stress management and protective dental appliances in mitigating symptoms and preserving dental health.
Conclusion
In conclusion, understanding and addressing common dental problems are essential steps toward maintaining optimal oral health and overall well-being. By recognizing the signs and symptoms of tooth decay, gum disease, and other dental issues, individuals can seek timely intervention and preventive care to mitigate risks and preserve their smiles. Through a combination of proper oral hygiene practices, regular dental check-ups, and personalized treatment plans, individuals can navigate common dental challenges with confidence and achieve lasting oral health. Embracing proactive dental care and seeking professional assistance when needed are crucial components of a comprehensive approach to dental wellness.
In exploring and pursuing your dental studies, we wish you all the best in becoming a dentist. In case you encounter challenges or need guidance during this study period, do not hesitate to contact us.
Email at;williamsassignmenthelpfredrick@gmail.com
14 Common Lung Diseases

Introduction
Lung diseases represent some of the most severe health threats globally. The rise of industrialization, environmental pollution, and tobacco usage significantly contribute to the prevalence of these diseases. This article, outlines the most common lung diseases, their symptoms, causes, and treatments.
1. Pneumonia

Pneumonia is an inflammation of the lung parenchyma caused by bacteria, viruses, fungi, or other pathogens. It poses a significant risk to the elderly, immunocompromised individuals, and those with chronic conditions but can also affect healthy individuals. Pneumonia can be classified based on the causative agent, such as bacterial pneumonia (e.g., Streptococcus pneumoniae), viral pneumonia (e.g., influenza virus), or fungal pneumonia (e.g., Pneumocystis jirovecii).
Symptoms
Fever
Cough with sputum
Chest pain
Shortness of breath
Fatigue
Sweating and shaking chills
Nausea, vomiting, or diarrhea (less common)
Diagnosis Diagnosis of pneumonia typically involves a combination of patient history, physical examination, chest X-rays, and sputum cultures. Blood tests may also be conducted to identify the causative agent.
Treatment Depending on the cause, treatments may include:
Antibiotics for bacterial pneumonia.
Antiviral medications for viral pneumonia.
Antifungal therapies for fungal pneumonia. Supportive care such as rest, fluids, and over-the-counter medications to reduce fever and manage pain can also alleviate symptoms. In severe cases, hospitalization may be required to provide intravenous antibiotics, oxygen therapy, or mechanical ventilation.
2. Bronchitis

Bronchitis involves the inflammation of the bronchial tubes, which carry air to and from the lungs. It can be acute, often following colds or the flu, or chronic, usually resulting from smoking or long-term exposure to irritants like pollution or dust.
Symptoms
Persistent cough (productive or dry)
Sputum production (clear, white, yellowish-gray, or green)
Fatigue
Shortness of breath
Slight fever and chills
Chest discomfort
Diagnosis Diagnosis typically involves a physical examination, where a doctor listens to the patient’s lungs with a stethoscope. Additional tests, such as a chest X-ray, sputum tests, or pulmonary function tests, may be conducted to rule out other conditions like pneumonia or asthma.
Treatment
Acute bronchitis: Symptomatic treatment includes rest, fluids, and over-the-counter pain relievers and cough medications. Inhalers or nebulizers may be prescribed to ease breathing.
Chronic bronchitis: Management may involve bronchodilators, steroids, and pulmonary rehabilitation. Smoking cessation and avoiding lung irritants are crucial for treatment.
3. Chronic Obstructive Pulmonary Disease (COPD)

COPD is a progressive, irreversible disease characterized by chronic inflammation of the airways, primarily due to smoking, environmental pollutants, or long-term exposure to respiratory irritants. COPD includes chronic bronchitis and emphysema, conditions that often coexist and lead to airflow obstruction.
Symptoms
Chronic cough
Sputum production
Shortness of breath, especially during physical activities
Wheezing
Chest tightness
Frequent respiratory infections
Fatigue
Unintended weight loss (in advanced stages)
Diagnosis COPD is diagnosed through a combination of patient history, physical examination, and spirometry, a test that measures the amount of air a person can exhale and how quickly they can do so. Chest X-rays, CT scans, and arterial blood gas analysis may also be used.
Prevention and Treatment Preventive measures include:
Smoking cessation
Vaccinations (influenza and pneumococcal vaccines)
Reducing exposure to lung irritants
Treatments involves;
Bronchodilators to relax the muscles around the airways
Inhaled steroids to reduce airway inflammation
Pulmonary rehabilitation programs
Oxygen therapy for severe cases
Surgery (e.g., lung volume reduction surgery or lung transplant) in advanced cases
4. Lung Cancer

Lung cancer involves the uncontrolled growth of malignant cells in the lung tissues. Major risk factors include smoking, exposure to secondhand smoke, exposure to carcinogens (e.g., asbestos, radon), and genetic predisposition.
Types
Small cell lung cancer (SCLC): Often linked to heavy smoking, SCLC is aggressive and spreads quickly.
Non-small cell lung cancer (NSCLC): More common and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Symptoms
Persistent cough
Chest pain
Weight loss
Hemoptysis (coughing up blood)
Shortness of breath
Hoarseness
Bone pain (in advanced stages)
Headache (if cancer spreads to the brain)
Diagnosis Diagnosis involves imaging tests (chest X-rays, CT scans, PET scans), sputum cytology, and tissue biopsy. Molecular testing may be done to identify specific genetic mutations that can be targeted with specific treatments.
Treatment
Surgery to remove the tumor or part of the lung
Chemotherapy to kill cancer cells
Radiation therapy to destroy cancer cells or shrink tumors
Targeted drug therapies to attack specific genetic changes in cancer cells
Immunotherapy to help the immune system fight cancer
5. Pleurisy
Pleurisy, or pleuritis, is the inflammation of the pleura, the tissue lining the lungs and chest cavity. It can be caused by infections (viral, bacterial, or fungal), injuries, autoimmune diseases (e.g., lupus, rheumatoid arthritis), or other underlying conditions.
Symptoms
Sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing
Shortness of breath
Cough
Fever (if infection is present)
Diagnosis Diagnosis involves a physical examination, chest X-rays, ultrasound, CT scans, and blood tests to identify the underlying cause. Thoracentesis, a procedure to remove and analyze pleural fluid, may be performed.
Treatment Treatment depends on the underlying cause and may include:
Antibiotics for bacterial infections
Antiviral medications for viral infections
Anti-inflammatory medications (e.g., NSAIDs) to reduce pain and inflammation
Pain management with medications
Thoracentesis to drain excess fluid from the pleural space
6. Pulmonary Embolism

A pulmonary embolism (PE) occurs when a blood clot, usually originating in the legs (deep vein thrombosis), travels to the lungs, blocking blood flow and causing tissue damage. Risk factors include prolonged immobility, surgery, cancer, and certain genetic conditions.
Symptoms
Sudden shortness of breath
Chest pain (may be sharp and worsen with deep breathing or coughing)
Cough (sometimes with bloody sputum)
Rapid or irregular heartbeat
Lightheadedness or dizziness
Leg pain or swelling (if DVT is present)
Diagnosis: Diagnosis involves imaging tests such as chest X-rays, CT pulmonary angiography, and ventilation-perfusion (V/Q) scans. D-dimer blood tests and ultrasound of the legs may also be conducted.
Treatment Immediate treatment includes:
Anticoagulants (blood thinners) to prevent further clotting
Thrombolytics (clot-dissolving medications) for severe cases
Surgical or catheter-based procedures to remove the clot
Long-term anticoagulation therapy to prevent recurrence
7. Pulmonary Edema

Pulmonary edema is the accumulation of fluid in the lung alveoli, making breathing difficult. It can result from heart failure (cardiogenic pulmonary edema), acute respiratory distress syndrome (ARDS), or exposure to high altitudes (non-cardiogenic pulmonary edema).
Symptoms
Difficulty breathing (dyspnea), especially when lying down
Rapid heartbeat (tachycardia)
Wheezing or gasping for breath
Coughing up frothy, pink-tinged sputum
Excessive sweating
Cyanosis (bluish skin or lips)
Diagnosis Diagnosis involves physical examination, chest X-rays, and blood tests. Echocardiography and pulmonary artery catheterization may be used to determine the underlying cause and severity.
Treatment Treatment involves addressing the underlying cause and may include:
Diuretics to remove excess fluid
Medications to improve heart function (for cardiogenic pulmonary edema)
Supplemental oxygen or mechanical ventilation
Treating underlying conditions such as infections or high altitude exposure
8. Pulmonary Fibrosis

Pulmonary fibrosis is the thickening and scarring of lung tissue, leading to reduced oxygen absorption. Causes include chronic exposure to environmental pollutants, infections, genetic factors, and autoimmune diseases (e.g., scleroderma).
Symptoms
Shortness of breath (dyspnea)
Persistent dry cough
Fatigue
Unexplained weight loss
Aching muscles and joints
Clubbing (widening and rounding) of the fingertips or toes
Diagnosis Diagnosis involves a combination of patient history, physical examination, imaging tests (chest X-rays, high-resolution CT scans), pulmonary function tests, and sometimes lung biopsy. Blood tests may be used to identify underlying autoimmune diseases.
Treatment While there is no cure for pulmonary fibrosis, treatments focus on symptom management and slowing progression:
Medications such as pirfenidone and nintedanib to slow disease progression
Oxygen therapy
Pulmonary rehabilitation
Lung transplant in severe cases
9. Pneumoconiosis
Pneumoconiosis is a lung disease caused by inhaling dust particles, such as asbestos, silica, or coal dust, leading to lung scarring. It is a type of occupational lung disease commonly seen in miners, construction workers, and industrial workers.
Symptoms:
Chronic cough
Shortness of breath
Chest tightness
Progressive loss of lung function
Diagnosis: Diagnosis involves a detailed occupational history, physical examination, chest X-rays, and CT scans. Pulmonary function tests may also be conducted to assess the extent of lung damage.
Treatment Treatment includes:
Avoiding further exposure to dust
Medications to manage symptoms, such as bronchodilators and corticosteroids
Respiratory therapies
Pulmonary rehabilitation
10. Pulmonary Arterial Hypertension (PAH)
PAH is a form of high blood pressure affecting the arteries in the lungs and the right side of the heart. It can be idiopathic, familial, or associated with other conditions such as connective tissue diseases, congenital heart disease, or chronic liver disease.
Symptoms
Breathing difficulties (dyspnea), especially during physical activities
Dizziness or fainting (syncope)
Chest pain
Fatigue
Swelling in the ankles, legs, and abdomen (edema)
Cyanosis (bluish lips and skin)
Diagnosis Diagnosis involves echocardiography, right heart catheterization, chest X-rays, and CT scans. Blood tests and pulmonary function tests may also be conducted to assess lung and heart function.
Treatment Treatment strategies include:
Medications to relax blood vessels and improve blood flow, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs
Diuretics to reduce fluid retention
Oxygen therapy
Anticoagulants to prevent blood clots
In severe cases, surgical procedures such as atrial septostomy or lung transplant
11. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene, leading to thick, sticky mucus buildup in the lungs and other organs. This results in frequent infections, respiratory issues, and digestive problems.
Symptoms
Persistent cough with thick mucus
Recurrent lung infections
Wheezing or shortness of breath
Poor growth and weight gain in children
Salty-tasting skin
Severe constipation
Frequent greasy, bulky stools
Diagnosis Diagnosis involves genetic testing, sweat chloride tests, and newborn screening. Pulmonary function tests, chest X-rays, and sputum cultures may also be conducted to assess lung health.
Treatment Management includes:
Medications to thin mucus, antibiotics to treat infections, and bronchodilators to open airways
Chest physiotherapy to clear mucus
Enzyme supplements and high-calorie diets to manage digestive issues
Newer therapies targeting the underlying genetic defect, such as CFTR modulators
12. Respiratory Distress Syndrome (RDS)
RDS primarily affects premature infants due to a lack of surfactant, a substance necessary to keep the lungs open and facilitate gas exchange. Risk factors include premature birth, maternal diabetes, and multiple births.
Symptoms
Rapid, shallow breathing
Grunting sounds while breathing
Nasal flaring
Chest retractions (pulling in of the chest muscles)
Cyanosis (bluish color of the skin and mucous membranes)
Diagnosis Diagnosis involves clinical assessment, chest X-rays, and blood gas analysis to measure oxygen and carbon dioxide levels. Prenatal tests can also help identify at-risk pregnancies.
Treatment Treatment includes:
Surfactant replacement therapy to improve lung function
Mechanical ventilation or continuous positive airway pressure (CPAP) to support breathing
Oxygen therapy
Supportive care such as fluids and nutrition
13. Sarcoidosis
Sarcoidosis is characterized by the growth of granulomas (small clusters of inflammatory cells) in the lungs and other organs, likely as an immune response to unknown triggers. The exact cause remains unclear, but genetic and environmental factors are believed to play a role.
Symptoms
Dry cough
Shortness of breath
Chest pain
Fatigue
Fever
Swollen lymph nodes
Skin lesions (e.g., erythema nodosum)
Diagnosis Diagnosis involves a combination of patient history, physical examination, chest X-rays, CT scans, and pulmonary function tests. Biopsy of affected tissues may be performed to confirm the presence of granulomas.
Treatment While sarcoidosis is often self-limiting and may resolve without treatment, severe cases may require:
Corticosteroids to reduce inflammation
Immunosuppressive medications (e.g., methotrexate, azathioprine)
Antimalarial drugs (e.g., hydroxychloroquine) for skin lesions
Regular monitoring and follow-up care to manage chronic cases
14. Asthma
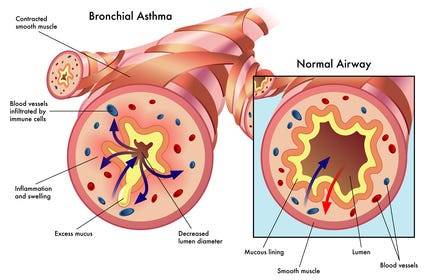
Definition and Causes: Asthma is a chronic inflammatory condition of the airways, causing episodes of wheezing, coughing, and chest tightness, often triggered by allergens, exercise, cold air, or respiratory infections. Genetic and environmental factors contribute to its development.
Symptoms
Wheezing
Shortness of breath
Chest tightness
Coughing, especially at night or early morning
Increased mucus production
Diagnosis: Diagnosis involves a detailed medical history, physical examination, and lung function tests (spirometry, peak flow measurement). Allergy testing and chest X-rays may also be conducted to identify triggers and rule out other conditions.
Treatment Management includes:
Avoiding known triggers
Inhalers (bronchodilators for quick relief, corticosteroids for long-term control)
Long-term control medications (e.g., leukotriene modifiers, long-acting beta agonists)
Immunotherapy (allergy shots) for severe allergies
Asthma action plans to manage symptoms and prevent attacks
Conclusion
Lung diseases encompass a wide range of conditions, each with distinct causes, symptoms, and treatments. Preventive measures such as avoiding smoking, reducing exposure to environmental pollutants, and timely vaccinations can significantly reduce the risk of developing many of these diseases. Early diagnosis and appropriate management are crucial in improving outcomes and quality of life for individuals affected by lung diseases. For personalized medical advice and treatment, consult with healthcare professionals.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: expertassignment46@gmail.com for professional guidance.
The Endocrine System

Introduction
The endocrine system is a complex network containing a symphony of hormonal interactions crucial for maintaining physiological equilibrium. Comprising glands, organs, and tissues dispersed throughout the body, its influence allows various bodily functions, spanning from metabolism to reproduction and beyond. This topic endeavors to provide an in-depth exploration of the endocrine system, encompassing its anatomy, physiological functions, associated conditions, and strategies for proactive care. By indulging into this indispensable regulatory system, we aim to equip readers with a comprehensive understanding to prioritize their hormonal health effectively.
Anatomy of the Endocrine System
The anatomy of the endocrine system is contained by an array of specialized glands, organs, and tissues, each endowed with the capacity to synthesize and dispatch hormones into the bloodstream. Principal among these are:
Endocrine Glands: These specialized tissues, including the pituitary gland, thyroid gland, and adrenal glands, secrete hormones directly into circulation, exerting systemic effects.
Endocrine Organs: Organs such as the hypothalamus, pancreas, and reproductive glands contribute to hormonal regulation, interfacing closely with the nervous system to modulate physiological responses.
Endocrine-Related Tissues: Adjunct to traditional endocrine structures, adipose tissue, kidneys, and even the heart harbor the capability to produce hormones, further augmenting the system’s complexity and regulatory capacity.
Functions of the Endocrine System
The cardinal function of the endocrine system is hormone secretion, holding up varied network of intercellular communication. Hormones, acting as molecular messengers, traverse the bloodstream to target cells, eliciting diverse physiological responses.
Key functions include:
Metabolism Regulation: Hormonal content govern metabolic processes, dictating energy expenditure, glucose homeostasis, and lipid metabolism.
Homeostatic Control: Endocrine signaling regulates internal threshold, modulating blood pressure, fluid balance, and body temperature.
Development and Growth: Hormonal interplay underpins growth trajectories and developmental milestones, steering embryonic stages and pubertal maturation.
Sexual Function and Reproduction: Hormonal modulation governs reproductive physiology, controlling fertility, libido, and secondary sexual characteristics.
Neuroendocrine Integration: The endocrine system reveals intimately with the nervous system, harmonizing behavioral and physiological responses, including mood regulation and sleep-wake cycles.
Conditions and Disorders
A spectrum of endocrine-related ailments afflicts individuals, stemming from hormonal imbalances, glandular dysfunctions, or neoplastic proliferations. Noteworthy conditions encompass:
Diabetes and Metabolic Disorders: Spanning type 1 and type 2 diabetes, metabolic syndrome, and obesity, these conditions disrupt glucose homeostasis and metabolic equilibrium.
Endocrine Cancers and Tumors: Malignancies affecting endocrine tissues, including adrenal tumors, pituitary adenomas, and thyroid malignancies, necessitate specialized oncological management.
Thyroid Dysfunction: Hypo- and hyperthyroidism, thyroid nodules, and autoimmune thyroiditis typify prevalent thyroid disorders, precipitating diverse clinical manifestations.
Reproductive and Sexual Health Disorders: From polycystic ovary syndrome (PCOS) to erectile dysfunction, disruptions in reproductive hormone signaling manifest as infertility, menstrual irregularities, and sexual dysfunction.
Proactive Care and Health Maintenance
In fostering endocrine wellness, a holistic approach integrating lifestyle modifications and environmental awareness is imperative. Strategies for promoting endocrine health encompass:
Lifestyle Optimization: Embracing a balanced diet, regular exercise regimen, and adequate sleep hygiene fosters metabolic resilience and hormonal equilibrium.
Environmental Vigilance: Mitigating exposure to endocrine-disrupting chemicals pervasive in everyday products, such as plastics, pesticides, and personal care items, reduces the risk of hormonal perturbations.
Health Surveillance: Individuals with familial predispositions to endocrine disorders benefit from proactive screening and vigilant symptom monitoring, facilitating early intervention and optimal disease management.
Conclusion
The endocrine entails physiological regulation, producing hormonal interactions essential for vitality and well-being. By looking at anatomy, physiological functions, associated conditions, and avenues for proactive care, this discourse endeavors to foster a comprehensive understanding of the endocrine system Empowered with knowledge, individuals can prioritize their hormonal health, embracing proactive measures to optimize their overall well-being and quality of life.
For medical students navigating the study of endocrinology and seeking guidance and academic support during their study period, Expert Academic Assignment Help offers invaluable assistance. With our expertise and resources, we provide tailored solutions to aid in comprehension, research, and academic success. Don’t hesitate to reach out to us for personalized assistance and elevate your understanding of this vital field. Your academic journey awaits, and we’re here to help you excel.
Contact us at expertassignment46@gmail.com for professional assistance,
Atherosclerosis

Introduction
Atherosclerosis is a chronic and progressive condition characterized by the accumulation of plaque within the walls of arteries, leading to their hardening and narrowing. Despite being often asymptomatic in its early stages, atherosclerosis poses significant risks to cardiovascular health and can result in severe complications such as heart attacks, strokes, and peripheral artery disease (PAD). Therefore, comprehensive knowledge of its symptoms, causes, prevention strategies, diagnosis methods, and treatment options is imperative for effectively managing its impact on individuals’ well-being.
Symptoms of Atherosclerosis

Atherosclerosis typically advances silently, with symptoms only becoming apparent as arteries become significantly obstructed or when a cardiovascular event occurs. The manifestation of symptoms varies depending on the affected arteries, each presenting distinct clinical presentations:
Coronary Arteries: The narrowing of coronary arteries due to atherosclerosis can lead to symptoms such as arrhythmia (irregular heartbeat), angina (chest pain or pressure), and shortness of breath, especially during physical exertion.
Cerebral Arteries: Atherosclerosis affecting cerebral arteries may manifest as numbness or weakness in the limbs, difficulty speaking or understanding speech, drooping facial muscles, paralysis, severe headache, or vision problems, indicating a heightened risk of stroke.
3. Peripheral Arteries: Individuals with atherosclerosis in peripheral arteries may experience symptoms such as leg pain when walking (intermittent claudication), numbness, cold extremities, aching or burning sensations in the feet, and slow-healing wounds or infections, reflecting compromised blood flow to the extremities
4. Renal Arteries: Atherosclerosis affecting renal arteries can result in elevated blood pressure (hypertension) and eventual kidney failure, highlighting the systemic impact of arterial narrowing on vital organ function.
Causes and Stages of Atherosclerosis

The development and progression of atherosclerosis involve a series of intricate biological processes initiated by damage to the endothelium, the delicate inner lining of arteries. As plaque composed of cholesterol, fat, calcium, and inflammatory substances accumulates within arterial walls, the disease progresses through distinct stages:
Damage to the Endothelium: The initial stage of atherosclerosis is characterized by injury to the endothelial cells lining the arteries, often attributed to risk factors such as high cholesterol, hypertension, inflammation, obesity, diabetes, and smoking.
2. Formation of Fatty Streaks: Following endothelial damage, the infiltration of low-density lipoprotein (LDL) cholesterol into the arterial wall triggers an inflammatory response, leading to the formation of fatty streaks — the earliest visible signs of atherosclerosis.
3 . Development of Fibrous Plaques: Over time, the accumulation of cholesterol-laden foam cells and the proliferation of smooth muscle cells contribute to the formation of fibrous plaques, which protrude into the arterial lumen and impede blood flow.
4 . Formation of Complicated Lesions: Advanced atherosclerosis is characterized by the formation of complicated lesions, where unstable plaques prone to rupture expose thrombogenic components, leading to the formation of blood clots and subsequent cardiovascular events such as myocardial infarction or ischemic stroke.
Risk Factors for Atherosclerosis
Numerous modifiable and non-modifiable risk factors influence the development and progression of atherosclerosis, underscoring the multifactorial nature of the disease. These risk factors include:
High Cholesterol: Elevated levels of LDL cholesterol, commonly referred to as “bad” cholesterol, promote the deposition of cholesterol within arterial walls, contributing to plaque formation and atherosclerosis progression.
2. High Blood Pressure: Hypertension exerts mechanical stress on arterial walls, accelerating endothelial damage and promoting atherosclerosis development
3. Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis or systemic lupus erythematosus, exacerbate endothelial dysfunction and foster plaque formation within arteries.
4. Obesity: Excess adiposity predisposes individuals to metabolic abnormalities, including dyslipidemia and insulin resistance, which fuel atherosclerosis progression.
5. Diabetes: Both type 1 and type 2 diabetes mellitus increase the risk of atherosclerosis by inducing endothelial dysfunction, promoting inflammation, and accelerating the formation of advanced glycation end-products (AGEs) implicated in vascular
6. Smoking: Tobacco smoke contains toxic compounds that promote endothelial injury, oxidative stress, and inflammation, exacerbating the progression of atherosclerosis and increasing the risk of cardiovascular events.
7.Sedentary Lifestyle: Physical inactivity contributes to metabolic derangements, including obesity, dyslipidemia, and insulin resistance, fostering atherosclerosis development and cardiovascular risk.
8. Family History of Heart Disease: Genetic predisposition plays a significant role in atherosclerosis susceptibility, with familial clustering of cardiovascular risk factors amplifying the likelihood of disease manifestation.
9. Poor Diet: Diets rich in saturated fats, trans fats, refined carbohydrates, and excess sodium promote dyslipidemia, hypertension, and endothelial dysfunction, fueling atherosclerosis progression.
9 .Stress: Chronic stress triggers sympathetic nervous system activation and cortisol release, contributing to hypertension, inflammation, and atherosclerosis development
10. Sleep Apnea: Obstructive sleep apnea, characterized by recurrent episodes of upper airway obstruction during sleep, disrupts normal cardiovascular function and exacerbates atherosclerosis progression.
Identifying and addressing these risk factors through targeted interventions and lifestyle modifications are essential for mitigating the burden of atherosclerosis and reducing the risk of cardiovascular events.
Diagnosis and Treatment of Atherosclerosis

Accurate diagnosis and effective management of atherosclerosis require a multidisciplinary approach involving clinical evaluation, imaging studies, and laboratory testing. Diagnostic modalities utilized in the assessment of atherosclerosis include:
Physical Examination: Healthcare providers perform a comprehensive physical examination, assessing vital signs, auscultating for abnormal heart sounds or bruits, and palpating for peripheral pulses to evaluate cardiovascular health.
Imaging Tests: Various imaging modalities are employed to visualize arterial anatomy, assess plaque burden, and identify areas of stenosis or occlusion. These includes;
Angiography: Intravascular contrast dye is utilized to visualize arterial lumens and detect areas of stenosis or occlusion via X-ray imaging.
Ultrasound: Non-invasive ultrasound techniques, such as carotid ultrasound or abdominal ultrasound, enable the assessment of arterial wall thickness, plaque morphology, and blood flow characteristics.
Computed Tomography (CT) Angiography: CT angiography provides detailed anatomical imaging of arterial structures, facilitating the identification of atherosclerotic lesions and assessing their severity.
Magnetic Resonance Angiography (MRA): MRA employs magnetic resonance imaging (MRI) techniques to generate high-resolution images of blood vessels, aiding in the evaluation of arterial stenosis, plaque composition, and hemodynamic parameters.
3. Laboratory Evaluations: Blood tests are conducted to assess lipid profiles, inflammatory markers, and other biochemical parameters associated with cardiovascular risk. These include
Lipid Profile: Measurement of serum lipid levels, including total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides, provides insight into atherosclerosis risk and treatment efficacy.
Inflammatory Markers: Assessment of inflammatory biomarkers, such as C-reactive protein (CRP) or interleukin-6 (IL-6), aids in risk stratification and monitoring disease activity in individuals with atherosclerosis.
Blood Glucose: Screening for abnormal glucose metabolism, including fasting blood glucose and hemoglobin A1c (HbA1c) levels, helps identify individuals at risk of diabetes-associated atherosclerosis complications
4. Functional Tests: Functional assessments, such as stress testing or ankle-brachial index (ABI) measurement, are performed to evaluate cardiovascular function and assess the impact of atherosclerosis on tissue perfusion.
Once diagnosed, the management of atherosclerosis encompasses various approach targeting risk factor modification, pharmacological intervention, and, when indicated, invasive procedures to alleviate arterial obstruction and prevent cardiovascular events.
Treatment strategies for atherosclerosis include:
Lifestyle Modifications: Lifestyle interventions form the cornerstone of atherosclerosis management, emphasizing dietary modifications, regular physical activity, smoking cessation, stress reduction, and weight management to optimize cardiovascular health and mitigate disease progression.
Medication Management: Pharmacological therapy plays a pivotal role in atherosclerosis treatment, targeting modifiable risk factors such as dyslipidemia, hypertension, and inflammation. Commonly prescribed medications include
Statins: HMG-CoA reductase inhibitors, such as atorvastatin or simvastatin, reduce LDL cholesterol levels and stabilize atherosclerotic plaques, lowering the risk of cardiovascular events.
Antihypertensive Agents: Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and calcium channel blockers are utilized to control blood pressure and mitigate endothelial dysfunction in individuals with hypertension-associated atherosclerosis.
Antiplatelet Therapy: Aspirin and other antiplatelet agents, such as clopidogrel or ticagrelor, inhibit platelet aggregation and reduce the risk of thrombotic events in individuals with established atherosclerosis or high cardiovascular risk.
Antidiabetic Medications: Oral hypoglycemic agents, insulin, or glucagon-like peptide-1 (GLP-1) receptor agonists are prescribed to achieve glycemic control and minimize the risk of diabetes-related atherosclerosis complications.
3. Invasive Procedures: In cases of severe arterial stenosis or symptomatic atherosclerotic disease refractory to medical therapy, invasive interventions may be warranted to restore arterial patency and alleviate ischemic symptoms. These include:
Percutaneous Coronary Intervention (PCI): Angioplasty with or without stent placement is performed to widen narrowed coronary arteries and improve myocardial perfusion in individuals with coronary artery disease (CAD).
Coronary Artery Bypass Grafting (CABG): Surgical revascularization using autologous or synthetic conduits bypasses obstructed coronary vessels, restoring blood flow to ischemic myocardial territories in patients with multivessel CAD or left main coronary artery disease.
Carotid Endarterectomy: Surgical removal of atherosclerotic plaque from carotid arteries reduces the risk of stroke in individuals with significant carotid stenosis and a history of transient ischemic attacks (TIAs) or cerebrovascular events.
Peripheral Arterial Interventions: Endovascular procedures, such as angioplasty, stenting, or atherectomy, are performed to treat lower extremity arterial disease and alleviate claudication symptoms in patients with peripheral artery disease (PAD).
Secondary Prevention Strategies: Beyond acute management, secondary prevention measures aim to prevent recurrent cardiovascular events and minimize disease progression through comprehensive risk factor modification, medication adherence, and ongoing surveillance of disease activity
Prevention of Atherosclerosis

Preventive strategies for atherosclerosis focus on addressing modifiable risk factors and promoting cardiovascular health through lifestyle modifications, health education, and targeted interventions. Key components of atherosclerosis prevention include:
Healthy Lifestyle: Encouraging individuals to adopt a healthy lifestyle characterized by balanced nutrition, regular physical activity, adequate sleep, stress management, and avoidance of harmful habits such as smoking or excessive alcohol consumption is paramount for reducing atherosclerosis risk
2. Dietary Modifications: Emphasizing a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and unsaturated fats while limiting intake of saturated fats, trans fats, cholesterol, sodium, and added sugars helps optimize lipid profiles, blood pressure, and overall cardiovascular health.
3. Physical Activity: Promoting regular exercise and physical activity is essential for maintaining cardiovascular fitness, weight management, insulin sensitivity, and endothelial function, thereby reducing the risk of atherosclerosis and its complications.
4. Tobacco Cessation: Implementing tobacco cessation programs and providing support for smoking cessation initiatives are critical for reducing atherosclerosis risk and improving overall cardiovascular outcomes.
5. Stress Management: Teaching stress reduction techniques such as mindfulness meditation, yoga, deep breathing exercises, or cognitive-behavioral therapy empowers individuals to cope with stressors effectively and mitigate their detrimental effects on cardiovascular health.
5 . Health Education: Educating individuals about the risks associated with atherosclerosis, the importance of early detection, and the benefits of preventive measures fosters informed decision-making and empowers individuals to take proactive steps towards cardiovascular wellness.
6. Regular Screening: Encouraging regular medical checkups and health screenings enables early detection of cardiovascular risk factors, facilitating timely intervention and personalized risk stratification for individuals at heightened risk of atherosclerosis.
Conclusion
In conclusion, atherosclerosis represents a significant public health challenge with far-reaching implications for cardiovascular morbidity and mortality. By majoring on the pathophysiology of atherosclerosis, identifying modifiable risk factors, and implementing evidence-based preventive strategies, healthcare providers can effectively mitigate the burden of atherosclerotic disease and promote cardiovascular health across diverse populations. Empowering individuals with knowledge, facilitating lifestyle modifications, and fostering a collaborative approach to atherosclerosis prevention and management are essential steps towards achieving optimal cardiovascular outcomes and enhancing quality of life for individuals affected by this pervasive condition.
As you navigate the complexities of cardiovascular health, remember that support and guidance are always available. Seek assistance from Expert Academic Assignment Help whenever needed.
Your journey in medicine is about more than just acquiring knowledge — it’s about embodying compassion, empathy, and continuous learning. Together, let’s strive for optimal cardiovascular health for all.
Email us at expertassignment46@gmail.com
Wishing you success and fulfillment in your medical journey.
How Does The Drug Got Excreted / Eliminated From The Body?

Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: expertassignment46@gmail.com
Your excellence our pride.
Strategies to Writing a Perfect College Essay

1. Be Authentic
Authenticity is crucial in college essays. It involves selecting a topic or perspective that genuinely reflects who you are. Readers can often discern when a writer is not being authentic, whether it’s through overly embellished language or choosing a topic solely for its perceived impressiveness. Embrace your own voice, use humor naturally, and opt for subjects that hold genuine importance to you, providing a deeper insight into your character.
2. Grab the Reader From the Start
The opening of your essay is a critical opportunity to capture the reader’s attention. A bold statement, a thoughtful quote, an engaging question, or a vivid descriptive scene can set the tone for the entire piece. A clear and compelling thesis statement early on helps guide the reader and establishes the purpose of your essay. This initial impact is essential when competing with numerous other applicants for the admission officer’s attention.
3. Focus on Deeper Themes

Facts and achievements are important, college proffesers are interested in understanding who you are as a person. Delve into deeper themes by connecting your experiences, successes, and adversities to your personal growth. It’s not just about listing accomplishments but demonstrating how those experiences shaped you. This provides a more comprehensive view of your character and journey.
4. Show Don’t Tell

Instead of presenting a mere list of accomplishments, engage the reader by showing scenes and sharing anecdotes. The most captivating essays draw readers into the writer’s world, allowing them to experience the emotional journey. Highlighting the lessons learned and personal insights gained creates a more impactful narrative.
5. Try Doing Something Different
To make your essay stand out, consider approaching your subject from a unique perspective. While common themes like sports-related obstacles or volunteer stories are popular for a reason, exploring a different angle can set you apart. For instance, writing about lessons learned from losses rather than wins can demonstrate resilience and self-awareness.
6. Write With the Reader in Mind

Craft your essay with a clear and logical structure, ensuring that one idea flows naturally into the next. Effective use of transitions between paragraphs enhances the readability of your essay. Anticipate questions the reader might have, and provide the necessary background information. Ensure that the essay is well-organized, avoiding unnecessary wordiness.
7. Write Several Drafts
The importance of multiple drafts cannot be overstated. Setting your essay aside for a few days and returning to it with a fresh perspective often reveals new insights. Starting the writing process early allows sufficient time for revisions. Each draft provides an opportunity to refine your narrative, strengthen arguments, and enhance overall clarity.
8. Read It Aloud

Reading your essay aloud is a valuable editing technique. It helps identify awkward or unnatural-sounding passages. This method allows you to assess the flow of your writing and ensures that your voice remains consistent throughout the essay. It’s an effective way to catch any discrepancies that might be missed during silent reading.
9. Don’t Repeat
Avoid redundancy by not rehashing information already present in other parts of your application. Your essay should contribute new insights, providing a fresh perspective on who you are. Ensure that your essay aligns with the overall theme of your application and directly addresses any questions or prompts given.
10. Ask Others to Read Your Essay

Diverse perspectives are valuable in the editing process. Seek feedback from different individuals, such as teachers, parents, or siblings, to gain varied insights. Pay attention to their interpretations and revise the essay based on their feedback. If any confusion arises among readers, address it through revisions to ensure clarity.
11. Pay Attention to Form
While there might not be strict word limits for college essays, maintaining a balance is crucial. The Common App suggests around 650 words, and adhering to such guidelines is advisable. Additionally, pay attention to formatting details such as readable fonts, proper spacing, and correct dialogue presentation. A visually appealing essay contributes to a positive reader experience.
12. End Your Essay With a “Kicker”

The conclusion is as crucial as the introduction. A “kicker” provides a strong, memorable closing that leaves a lasting impression. It should effectively tie together the key points of your essay, leaving the reader satisfied. Aim for conciseness, coherence, and use vivid details to reinforce the overall message of your essay.
Incorporating these strategies into your college essay writing process can significantly enhance its impact and increase your chances of making a positive impression on admissions officers. Remember, a well-crafted essay can be a powerful tool in differentiating yourself from other applicants
We wish you all the best in your essay writing and studies.
For guidance and and Assistance in all your assignment Help;
Email us at; williamsassignmenthelpfredrick@gmail.com
What is mental health?

Mental health is a state of well-being that enables individuals to cope with life stresses, realize their abilities, learn and work effectively, and contribute to their community.
It goes beyond the absence of mental disorders, emphasizing the importance of ongoing wellness and happiness.
Mental health issues affect daily life, relationships, and physical health.
Almost 1 in 5 adults in the U.S. experience mental health problems each year.
Risk Factors for Mental Health Conditions
Socioeconomic factors such as poverty and marginalization increase the risk.
2. Adverse childhood experiences, biological factors, and underlying medical conditions contribute to mental health issues.
3. Chronic stress, depression, and anxiety may result from physical health problems.
Types of Mental Health Disorders
1.Anxiety Disorders:
. Generalized Anxiety Disorder
. Panic Disorder
. Phobias
. Obsessive-Compulsive Disorder
. Post-Traumatic Stress Disorder
2. Mood Disorders:
Major Depression
Bipolar Disorder
Seasonal Affective Disorder
3. Schizophrenia Disorders:
Schizophrenia involves psychotic features, both positive (delusions, hallucinations) and negative (withdrawal, lack of motivation).
Early Signs of Mental Health Disorders
Withdrawal from social activities
Changes in sleep and eating patterns
Persistent feelings of hopelessness
Difficulty completing daily tasks
Thoughts of self-harm or harm to others
Diagnosis
Diagnosing mental health disorders involves a thorough medical history, physical exam, and psychological evaluation.
The American Psychiatric Association’s Diagnostic and Statistical Manual is often used for diagnosis.
Treatment
a. Psychotherapy
Cognitive Behavioral Therapy
Exposure Therapy
Dialectical Behavior Therapy
b. Medication
Antidepressants
Antipsychotics
Anxiolytics
c. Self-help
Lifestyle changes
Relaxation techniques
Support networks
Myths vs. Facts about Mental Health
Intelligence, age, and social status don’t determine mental health.
Teenagers can experience mental health issues.
People with mental health conditions are not necessarily dangerous or violent.
Psychiatric medications are not harmful; they are essential for managing symptoms.
Maintaining Mental Health
Regular exercise, balanced diet, and hydration contribute to mental well-being.
Quality sleep is crucial for mental health.
Relaxing activities, mindfulness, and gratitude practices help manage stress.
Suicide Prevention
Ask direct questions if someone is at immediate risk.
Listen without judgment.
Seek professional help and remove potential harmful objects.
Outlook
Most people can manage mental health symptoms with proper treatment and support.
Recovery may involve learning new coping mechanisms.
Mental health issues are associated with chronic health conditions.
Prevalence of mental disorders peaks in ages 18–25.
Conclusion
Mental health Consists of cognitive, behavioral, and emotional well-being. It involves managing existing conditions while maintaining ongoing wellness. Stress, depression, and anxiety can disrupt mental health, but various treatments, including psychotherapy and medication, are available. Myths about mental health abound, and maintaining mental well-being involves self-care practices and a support network. While mental health disorders are common, proper treatment and support can help individuals lead fulfilling lives.
For Health Sciences Assignment Help,
Email us at;
williamsliason@outlook.com
What Are The Stages of Fetal Growth During Pregnancy?

The development of a fetus during pregnancy is a complex and remarkable process, marked by significant changes and growth each month. This journey is typically divided into three stages known as trimesters, each lasting approximately three months. For Healthcare professionals we discuss fetal development in terms of weeks. Here’s a detailed overview of what entails during each month of pregnancy.
a) First Trimester

The first trimester of pregnancy encompasses weeks 1 through 12 and is characterized by the initial formation and rapid development of the embryo. This period is critical for establishing the foundation of the future baby’s organs and body systems. The first trimester is often associated with the onset of pregnancy symptoms, such as nausea, fatigue, and hormonal changes.
Month 1 (Weeks 1–4)
Weeks 1–2: The first two weeks of pregnancy are technically considered a preparatory period. During this time, the body releases hormones and prepares the uterus for a potential pregnancy. This period includes ovulation, where an egg is released from the ovary. If fertilization occurs, the zygote forms and marks the beginning of pregnancy.
Week 3: Fertilization occurs when a sperm cell meets the egg, creating a zygote. This single-celled entity undergoes rapid cell division as it travels down the fallopian tube towards the uterus.
Week 4: The zygote becomes a blastocyst, which is a cluster of cells that implants itself into the uterine lining. The amniotic sac and placenta begin to form, playing crucial roles in protecting and nourishing the developing embryo. By the end of this month, the blastocyst is about 2 millimeters long, roughly the size of a poppy seed.
Month 2 (Weeks 5–8)
The second month of pregnancy marks significant developmental milestones as the embryo transitions into more complex forms.
Week 5: The neural tube, which will become the brain and spinal cord, begins to form. The heart, initially a simple tube, starts to pulse, setting the stage for the development of the circulatory system.
Week 6: Limb buds appear, which will eventually become arms and legs. Structures for the ears, eyes, and mouth start to take shape. Blood cells begin to form, and circulation starts within the embryo.
Week 7: The process of ossification starts as bones begin replacing the soft cartilage, and the formation of the genitals commences. The embryo now resembles a tadpole due to its prominent tail.
Week 8: Major organs and body systems continue to develop. The hands and feet start to form web-like structures, and the umbilical cord, which provides nutrients and oxygen to the embryo, is fully developed. By the end of this month, the embryo, now referred to as a fetus, is about 0.5 to 1 inch long, similar to a black bean.
Month 3 (Weeks 9–12)
The third month of pregnancy is marked by significant growth and maturation of the embryo, transitioning into a more recognizable human form.
Week 9: Teeth and taste buds begin to form. The fetus starts developing muscles, and its body takes on a more human appearance, although the head remains disproportionately large.
Week 10: Limbs and digits are fully formed, and the external genitals start to develop, although they are not yet visible on an ultrasound. The placenta continues to grow, providing essential nutrients to the fetus.
Week 11: The fetus begins to move spontaneously, exploring its surroundings by opening and closing its fists and mouth. The bones harden, though the skin remains translucent. Facial features such as the nose and lips become more defined.
Week 12: All essential organs, limbs, bones, and muscles are present and will continue to mature and develop. The fetus is about 2.5 to 3 inches long, roughly the size of a plum. At this stage, the risk of miscarriage decreases significantly, and many women begin to feel relief from early pregnancy symptoms like morning sickness.
Second Trimester

The second trimester of pregnancy spans from weeks 13 to 26. This period is often considered the most comfortable phase of pregnancy as many early symptoms subside, and the risk of miscarriage decreases. The fetus undergoes significant growth and development, and the mother begins to feel fetal movements, known as quickening.
Month 4 (Weeks 13–16)
During the fourth month, the fetus continues to develop rapidly, and its features become more distinct.
Week 13: Vocal cords form, and the fetus’s head starts to grow proportionally to the rest of the body. The fetus begins to practice breathing movements by inhaling and exhaling amniotic fluid, which helps develop the lungs.
Week 14: The skin starts to thicken and fine hair, known as lanugo, begins to grow. The fetus can bring its fingers to its mouth and may start sucking its thumb. External genitals are fully formed, and fingerprints start to develop.
Week 15: The intestines and ears move to their final positions. The fetus practices more purposeful movements, such as thumb-sucking and smiling. The developing nervous system allows the fetus to respond to external stimuli, such as light and sound.
Week 16: The fetus can hear and respond to external sounds. Its eyes, although still closed, can perceive light. By the end of this month, the fetus is about 5 inches long and weighs around 4 ounces, comparable to an avocado.
Month 5 (Weeks 17–20)
The fifth month of pregnancy is marked by increased fetal activity and continued growth.
Week 17: Fat begins to accumulate under the skin, providing insulation and energy reserves. The fetus’s skin is covered with a protective coating called vernix, which prevents it from becoming chapped by the amniotic fluid.
Week 18: The fetus is covered in lanugo, which helps keep it warm and provides an additional layer of protection. The fetus starts to establish a sleep-wake cycle, and its movements become more noticeable to the mother.
Week 19: The fetus’s movements, including kicks and punches, become more frequent and noticeable. Unique fingerprints are fully formed, and the fetus may start to experience hiccups.
Week 20: Nails develop fully, and the sensory areas of the brain mature, allowing the fetus to respond more actively to its environment. By the end of this month, the fetus is about 9 to 10 inches long and weighs around 1 pound.
Month 6 (Weeks 21–24)
The sixth month of pregnancy is a period of significant development, particularly in the nervous and respiratory systems.
Week 21: Coordinated limb movements become more frequent, and the fetus’s bone marrow begins producing blood cells.
Week 22: The fetus’s grasping reflex strengthens, and it can touch its surroundings, including its own body and the umbilical cord. It can hear internal sounds, such as the mother’s heartbeat and external sounds, such as voices and music.
Week 23: The fetus’s viability outside the womb increases, though intensive medical care would be necessary if it were born prematurely. The fetus starts rapidly accumulating fat, which is essential for temperature regulation after birth.
Week 24: Lung development progresses, although the lungs are not yet mature enough for the fetus to breathe independently. The fetus is about 12 inches long and weighs around 2 pounds.
Third Trimester

The third trimester of pregnancy spans from weeks 27 to 40 and is characterized by rapid growth and final preparations for birth. During this period, the fetus gains weight quickly and undergoes the final stages of development necessary for survival outside the womb.
Month 7 (Weeks 25–28)
During the seventh month, the fetus continues to grow and develop reserves of body fat.
Week 25: Increased body fat makes the fetus’s skin less wrinkled and more plump. The nervous system matures rapidly, enhancing the fetus’s ability to respond to stimuli.
Week 26: Melanin production begins, contributing to the skin and eye color. The lungs start producing surfactant, a substance that helps the lungs function properly after birth.
Week 27: The fetus’s eyes open, and it develops eyelashes. The fetus begins to develop regular sleep and wake patterns, and its movements become more coordinated.
Week 28: The fetus may begin to position itself head-down in preparation for birth. By the end of this month, the fetus is about 14 to 15 inches long and weighs between 2 to 3 pounds.
Month 8 (Weeks 29–32)
The eighth month of pregnancy involves continued maturation and growth of the fetus, with a focus on brain development.
Week 29: The fetus’s movements become more distinct as space in the uterus becomes cramped. The brain develops rapidly, allowing the fetus to control its body temperature more effectively.
Week 30: The fetus’s brain continues to grow, and it can process information and respond to stimuli. The fetus begins to establish more distinct patterns of activity and rest.
Week 31: The fetus’s skin loses its translucency as fat accumulates beneath it. Most organs, except for the brain and lungs, are fully developed and ready for birth.
Week 32: The fetus is about 17 to 18 inches long and weighs up to 5 pounds. The brain continues to develop rapidly, and the fetus can hear and respond to a variety of sounds.
Month 9 (Weeks 33–36)
During the ninth month, the fetus continues to grow and mature, preparing for birth.
Week 33: The fetus’s bones harden, although the skull remains soft and flexible to facilitate passage through the birth canal.
Week 34: The protective vernix coating thickens, providing additional protection to the fetus’s skin.
Week 35: Brain growth continues, and the fetus’s brain is now capable of regulating essential body functions.
Week 36: The lanugo covering the fetus’s body begins to disappear, and hair growth occurs on the head. The fetus is about 17 to 19 inches long and weighs 6 to 7 pounds.
Month 10 (Weeks 37–40)
The final month of pregnancy is a period of final preparations for birth, with the fetus reaching full maturity.
Week 37: The fetus’s toenails reach the tips of its toes. It continues to gain weight rapidly, preparing for the energy demands of life outside the womb.
Week 38: The fetus’s weight gain continues, and it starts to shed the vernix coating. The fetus moves lower into the pelvis in preparation for birth.
Week 39: The fetus is considered full-term and continues to develop and gain weight. It measures about 18 to 20 inches long and weighs between 7 to 9 pounds.
Week 40: The fetus is ready for birth. Its organs are fully developed and capable of functioning independently. The fetus positions itself head-down in the pelvis, preparing for delivery.
Throughout pregnancy, the fetus undergoes substantial growth and development, preparing for the transition to life outside the womb. Regular monitoring and care by healthcare providers are crucial to ensure the health and well-being of both the mother and the fetus. This comprehensive journey from a single cell to a fully developed baby highlights the incredible complexity of human development.
Expert Academic Assignment Help specializes in supporting medical students to study fetal growth during pregnancy. Our assistance includes study materials, tutoring, assignment help, and exam preparation, ensuring students understand fetal development. We provide mentorship, empowering students to excel academically and become competent healthcare professionals. Email: expertassignment46@gmail.comac
Nursing Essay

Introduction
Nursing, widely regarded as a challenging academic discipline, demands not only practical skills but also a profound ability to articulate one’s understanding through essays. Despite its predominantly practical nature, nursing essays serve as a critical medium for students to demonstrate their theoretical comprehension of nursing practice. This comprehensive guide aims to provide detailed recommendations, spanning from the methods of choosing a suitable topic to crafting a meticulously structured essay. By adhering to the guidance provided herein, nursing students can significantly enhance their writing skills, expand their knowledge base, and gain invaluable practical experience.
1. The Importance of Nursing

a. Understanding the Role of Nursing Essays
Nursing essays play a major role in assessing a student’s grasp of theoretical aspects of nursing practice. This section delves into the significance of essays in demonstrating clarity of thought, the ability to express arguments, and the implications for academic success.
b. The Link Between Writing Skills and Academic Achievement
Examining how proficient writing contributes to academic success, this subsection explores how essays serve as a direct reflection of a student’s ability to articulate complex ideas and arguments in a coherent manner.
2. Choosing a Suitable Topic

a. The Complexity of Nursing Practice
An in-depth analysis of the broad nature of nursing practice, discussing its various dimensions, functions, and roles. Understanding the complexity of the field is crucial in selecting an engaging and relevant essay topic.
b. Criteria for Choosing a Nursing Essay Topic
This subsection introduces specific criteria for selecting an appropriate essay topic. Emphasizing critical thinking, open-mindedness, and cultural competence, it provides practical advice on avoiding personal biases and ensuring a broad perspective.
c. Examples of Engaging Nursing Essay Topics
Offering a range of potential topics, this section provides concrete examples to inspire nursing students. Topics such as “Cultural Sensitivity in the Context of Advanced Nursing Practice” and “The Role of Informed Consent in Quantitative Research” are explored
3. Evaluating Evidence

a. The Importance of Evidence in Nursing Essays
An exploration of the main role evidence plays in substantiating arguments in nursing essays. This section emphasizes the need for practice-based evidence and the importance of critical evaluation.
b. Distinguishing Types of Evidence
A comprehensive breakdown of different types of evidence, including research-based and experiential evidence. Understanding these distinctions is essential in choosing evidence that aligns with the essay’s objectives.
c. Evaluating the Merits of Evidence
Indulging into the process of evaluating evidence, this subsection discusses the criteria for assessing the authority, reliability, and validity of research designs. Practical tips on making informed judgments about evidence are provided.
Section 4: Understanding Types of Evidence
4. Categorizing Evidence in Nursing Essay

Examining the different types of evidence used in nursing essays and their specific roles. A detailed discussion on how various research designs impact the nature and relevance of evidence.
a. The Significance of Experiential Evidence
Highlighting the importance of experiential evidence in nursing essays, particularly in the analysis of case studies and risk management. Practical insights into incorporating experiential evidence effectively.
b. The Reliability of Research-Based Evidence
Exploring the reliability of evidence derived from research, with an emphasis on the meticulous design of studies to ensure objectivity and validity. A critical discussion on the role of authentic data in supporting claims.
5.The Ultimate Structure of a Nursing Essay

a. Setting the Stage
A comprehensive exploration of the introduction’s role in capturing the reader’s attention, presenting the essay topic, and establishing the rationale for the paper. Practical advice on incorporating hooks, such as questions, statistical data, or quotes, is provided.
b. Crafting a Powerful Thesis Statement
An in-depth examination of the thesis statement, exploring its role as the linchpin of the essay. Examples of strong thesis statements are dissected to illustrate effective positioning and claim formulation.
c. The Main Body: Developing Coherent Arguments
A thorough analysis of the main body’s structure, emphasizing the importance of organizing ideas into clear paragraphs. Practical guidelines on presenting topic sentences, evidence, discussions, and concluding statements are provided.
d. Conclusion: Reinforcing Key Points
A detailed discussion on the conclusion’s role in summarizing key arguments, restating the thesis, and offering recommendations. Practical insights on framing a compelling conclusion that reinforces the essay’s significance.
e. Proofreading and Editing Tips
6. The Importance of Proofreading in Nursing Essays

A critical examination of the proofreading process, highlighting its significance in identifying and rectifying common mistakes. Practical insights into maintaining a scholarly tone and avoiding first-person expression
a. Avoiding Plagiarism Through Proper Citation
An exploration of the importance of proper citation to prevent plagiarism. Guidelines on citing information that is not common knowledge, ensuring academic integrity in nursing essa
b. Evaluating Readability and Coherence
Practical tips on assessing the overall readability and coherence of a nursing essay. Guidance on examining figures, tables, and graphs to enhance visual appeal and effectiveness.
d. Ensuring Consistency in Writing
An exploration of the need for consistency in nursing essays. Practical advice on evaluating the consistency of arguments, statements, and overall presentation
7.Recapitulation of the key points

A concise recapitulation of the key points discussed throughout the guide, reinforcing the critical elements of successful nursing essay writing.
a. Empowering Nursing Students Through Effective Writing
A concluding reflection on how mastering the art of nursing essay writing empowers students to excel academically, contribute meaningfully to the field, and become articulate advocates for healthcare.
Conclusion:
Mastering the art of nursing essay writing is a multifaceted journey that demands a nuanced understanding of the discipline, from choosing a relevant topic to evaluating evidence and crafting a well-structured essay. This comprehensive guide serves as a roadmap for nursing students, providing them with the tools and insights necessary to navigate the complexities of academic writing successfully. By following the detailed recommendations outlined herein, aspiring nurses can not only fulfill the requirements of their coursework but also make substantial contributions to the field through articulate and well-supported essays.
Wishing you all the best in Writing Nursing Essays.
Incase of any Enquiries, Guidance or Challenges faced during the process;
Email us at;
williamsassignmenthelpfredrick@gmail.com
10 Ways to Excel as a Nursing Student

Embarking on the journey of becoming a nursing student is a transformative experience marked by challenges and growth. In this dynamic and ever-evolving field, success requires more than just academic prowess; it demands resilience, adaptability, and a holistic approach to self-care. This guide presents essential tips for excelling as a nursing student, offering insights into the multifaceted aspects of academic, clinical, and personal development.
1.Be Flexible:
Nursing is a profession characterized by constant change and unexpected challenges. The ability to adapt is crucial, not only for academic success but also for preparing students for the dynamic realities of healthcare. This section explores the importance of flexibility in navigating clinical rotations, patient care, and unforeseen circumstances.
2.Join a Study Group: Collaboration is key to success in nursing school. Encouraging students to form study groups fosters a supportive environment where knowledge is shared, accountability is built, and lasting friendships are formed. The section emphasizes the benefits of collaborative learning and its long-term impact, especially during preparations for licensure exams.
3.Set Boundaries:
Nursing school demands a commitment that may require saying "no" to social engagements for the sake of study and rest. This section discusses the importance of setting boundaries, acknowledging the sacrifices needed, and reassures students that this phase is temporary, laying the foundation for a rewarding career.
4.Prioritize Attendance:
Attendance is non-negotiable in nursing school, particularly in clinical settings where unique learning opportunities may arise. This section underscores the significance of attending classes, labs, and clinical rotations, emphasizing the difficulty in making up for missed experiences and the impact on NCLEX exam eligibility.
5.Have a Consistent Self-Care Practice:
Managing stress is integral to a nursing student's well-being. This section advocates for self-care practices as non-negotiable, emphasizing that excellence extends beyond academic achievement to encompass overall personal thriving.
6.Rest Often:
Recognizing the limits of the human brain, this section advises students to schedule regular breaks during study sessions. Research-backed, purposeful breaks are highlighted for their positive impact on focus and productivity.
7.Reduce Your Work Hours:
Acknowledging the time-intensive nature of nursing studies, this section encourages students to assess their work commitments realistically. The importance of flexibility for clinical placements is emphasized, suggesting that sacrificing some work hours may be necessary for academic success.
8.Practice Your Note-Taking Skills:
Nursing education requires a shift from rote memorization to comprehensive understanding and critical thinking. This section delves into effective study habits, emphasizing active learning through diverse methods such as note-taking, participation in labs, and engaging in study groups.
9.Make Connections:
Building professional relationships during nursing education is crucial for future career prospects. This section stresses the value of getting to know instructors, clinical staff, and managers, emphasizing the potential benefits for job applications and recommendations.
10.Ask Questions:
Critical thinking is foundational to nursing practice, and asking questions is a key component of this skill. This section encourages students to question and understand the 'why' behind procedures and treatments, fostering a mindset of continuous learning and safe nursing practices.
In conclusion, excelling as a nursing student goes beyond academic achievements; it requires a holistic approach that integrates adaptability, collaboration, self-care, and critical thinking. By embracing these tips, nursing students can navigate the challenges of their education, setting the stage for a successful and fulfilling career in healthcare. As they embark on this transformative journey, the lessons learned will not only shape their academic success but also contribute to their growth as compassionate and competent healthcare professionals.
For Health Sciences Assignment Help, Contact Us at, williamsliason@outlook.com
-
 lazyphilosopherarbiter liked this · 6 months ago
lazyphilosopherarbiter liked this · 6 months ago -
 cheezbot liked this · 1 year ago
cheezbot liked this · 1 year ago -
 expertacademicassignmenthelp reblogged this · 1 year ago
expertacademicassignmenthelp reblogged this · 1 year ago