The Endocrine System
The Endocrine System

Introduction
The endocrine system is a complex network containing a symphony of hormonal interactions crucial for maintaining physiological equilibrium. Comprising glands, organs, and tissues dispersed throughout the body, its influence allows various bodily functions, spanning from metabolism to reproduction and beyond. This topic endeavors to provide an in-depth exploration of the endocrine system, encompassing its anatomy, physiological functions, associated conditions, and strategies for proactive care. By indulging into this indispensable regulatory system, we aim to equip readers with a comprehensive understanding to prioritize their hormonal health effectively.
Anatomy of the Endocrine System
The anatomy of the endocrine system is contained by an array of specialized glands, organs, and tissues, each endowed with the capacity to synthesize and dispatch hormones into the bloodstream. Principal among these are:
Endocrine Glands: These specialized tissues, including the pituitary gland, thyroid gland, and adrenal glands, secrete hormones directly into circulation, exerting systemic effects.
Endocrine Organs: Organs such as the hypothalamus, pancreas, and reproductive glands contribute to hormonal regulation, interfacing closely with the nervous system to modulate physiological responses.
Endocrine-Related Tissues: Adjunct to traditional endocrine structures, adipose tissue, kidneys, and even the heart harbor the capability to produce hormones, further augmenting the system’s complexity and regulatory capacity.
Functions of the Endocrine System
The cardinal function of the endocrine system is hormone secretion, holding up varied network of intercellular communication. Hormones, acting as molecular messengers, traverse the bloodstream to target cells, eliciting diverse physiological responses.
Key functions include:
Metabolism Regulation: Hormonal content govern metabolic processes, dictating energy expenditure, glucose homeostasis, and lipid metabolism.
Homeostatic Control: Endocrine signaling regulates internal threshold, modulating blood pressure, fluid balance, and body temperature.
Development and Growth: Hormonal interplay underpins growth trajectories and developmental milestones, steering embryonic stages and pubertal maturation.
Sexual Function and Reproduction: Hormonal modulation governs reproductive physiology, controlling fertility, libido, and secondary sexual characteristics.
Neuroendocrine Integration: The endocrine system reveals intimately with the nervous system, harmonizing behavioral and physiological responses, including mood regulation and sleep-wake cycles.
Conditions and Disorders
A spectrum of endocrine-related ailments afflicts individuals, stemming from hormonal imbalances, glandular dysfunctions, or neoplastic proliferations. Noteworthy conditions encompass:
Diabetes and Metabolic Disorders: Spanning type 1 and type 2 diabetes, metabolic syndrome, and obesity, these conditions disrupt glucose homeostasis and metabolic equilibrium.
Endocrine Cancers and Tumors: Malignancies affecting endocrine tissues, including adrenal tumors, pituitary adenomas, and thyroid malignancies, necessitate specialized oncological management.
Thyroid Dysfunction: Hypo- and hyperthyroidism, thyroid nodules, and autoimmune thyroiditis typify prevalent thyroid disorders, precipitating diverse clinical manifestations.
Reproductive and Sexual Health Disorders: From polycystic ovary syndrome (PCOS) to erectile dysfunction, disruptions in reproductive hormone signaling manifest as infertility, menstrual irregularities, and sexual dysfunction.
Proactive Care and Health Maintenance
In fostering endocrine wellness, a holistic approach integrating lifestyle modifications and environmental awareness is imperative. Strategies for promoting endocrine health encompass:
Lifestyle Optimization: Embracing a balanced diet, regular exercise regimen, and adequate sleep hygiene fosters metabolic resilience and hormonal equilibrium.
Environmental Vigilance: Mitigating exposure to endocrine-disrupting chemicals pervasive in everyday products, such as plastics, pesticides, and personal care items, reduces the risk of hormonal perturbations.
Health Surveillance: Individuals with familial predispositions to endocrine disorders benefit from proactive screening and vigilant symptom monitoring, facilitating early intervention and optimal disease management.
Conclusion
The endocrine entails physiological regulation, producing hormonal interactions essential for vitality and well-being. By looking at anatomy, physiological functions, associated conditions, and avenues for proactive care, this discourse endeavors to foster a comprehensive understanding of the endocrine system Empowered with knowledge, individuals can prioritize their hormonal health, embracing proactive measures to optimize their overall well-being and quality of life.
For medical students navigating the study of endocrinology and seeking guidance and academic support during their study period, Expert Academic Assignment Help offers invaluable assistance. With our expertise and resources, we provide tailored solutions to aid in comprehension, research, and academic success. Don’t hesitate to reach out to us for personalized assistance and elevate your understanding of this vital field. Your academic journey awaits, and we’re here to help you excel.
Contact us at expertassignment46@gmail.com for professional assistance,
More Posts from Expertacademicassignmenthelp and Others
Digestive System

The digestive system is a marvel of biological engineering, orchestrating the journey of food through the body, from the moment it enters the mouth to its exit through the anus. This complex process involves a network of organs, each playing a crucial role in breaking down food, absorbing nutrients, and eliminating waste. In this detailed exploration, we delve into the anatomy, functions, common conditions, care practices, and the importance of seeking medical attention for digestive system issues.
Anatomy of the Digestive System

Gastrointestinal (GI) Tract:
1.Mouth:
Initiating Digestion: Salivary glands activate as the sight and scent of food trigger the digestive process.
Chewing and Mixing: Food is chewed into digestible pieces, mixed with saliva to facilitate breakdown.
Swallowing: The tongue propels the food into the throat and esophagus.
2. Esophagus:
Transportation: A muscular tube conducting food to the stomach through peristalsis.
Sphincter Function: The lower esophageal sphincter relaxes to allow food entry and contracts to prevent stomach content reflux.
3.Stomach:
Container and Mixer: A hollow organ holding and mixing food with stomach enzymes for further breakdown.
Acid Secretion: Cells in the stomach lining secrete powerful acids and enzymes crucial for digestion.
Release to Small Intestine: Processed stomach contents move to the small intestine for further digestion.
4.Small Intestine:
Segments and Functions: Comprising the duodenum, jejunum, and ileum, each segment has distinct roles in digestion and nutrient absorption.
Enzymatic Breakdown: Pancreatic enzymes and bile from the liver aid in breaking down food.
Nutrient Absorption: The jejunum and ileum absorb nutrients into the bloodstream.
Consistency Changes: Contents transition from semi-solid to liquid as water, bile, enzymes, and mucus contribute to the process.
Biliary System

a. pancreas:
Enzyme Secretion: Releases digestive enzymes into the duodenum to break down proteins, fats, and carbohydrates.
Insulin Production: The pancreas produces insulin, a key hormone for sugar metabolism.
b. Liver:
Nutrient Processing: Processes nutrients absorbed by the small intestine.
Bile Production: Secretes bile into the small intestine, aiding in fat digestion and vitamin absorption.
Detoxification: Acts as the body’s chemical “factory,” detoxifying harmful substances.
c. Gallbladder:
Bile Storage: Stores and concentrates bile from the liver.
Release into Duodenum: Releases bile into the duodenum to assist in fat absorption.
Large Intestine (Colon):
Colon:
Waste Processing: Responsible for transforming waste into a convenient form for bowel movements.
Peristalsis: Propels stool through the colon, removing water and transitioning it from a liquid to a solid state.
Storage and Elimination: Stool is stored in the sigmoid colon until mass movements propel it into the rectum for elimination.
Rectum:
Chamber Function: A straight chamber connecting the colon to the anus.
Signaling and Holding: Signals the brain about stool presence and holds stool until evacuation.
Anus:
Final Elimination: The last part of the digestive tract, consisting of pelvic floor muscles and sphincters.
Sphincter Control: Surrounding sphincter muscles control stool release, preventing involuntary bowel movements.
Conditions and Disorders
Digestive system health can be affected by a spectrum of conditions, ranging from temporary issues to chronic diseases:
Temporary Conditions:
Constipation:
Frequency and Characteristics: Reduced bowel movements with dry and hard stool.
Difficulty and Pain: Straining during bowel movements, leading to discomfort.
2.Diarrhea:
Loose and Watery Stool: Abnormal stool consistency often caused by various factors.
Potential Causes: Bacterial infections, dietary issues, or unknown triggers.
3.Heartburn:
Misleading Name: Despite the name, heartburn is a digestive issue.
Acidic Backflow: Occurs when stomach acids move up the esophagus, causing discomfort in the chest.
4.Hemorrhoids:
Swollen Veins: Enlarged veins inside and outside the anus and rectum.
Symptoms: Pain, discomfort, and rectal bleeding.
5.Stomach Flu (Gastroenteritis):
Viral Infection: Infection of the stomach and upper part of the small intestine.
Duration: Typically lasts less than a week.
6.Ulcers:
Sore Development: Sores on the lining of the esophagus, stomach, or small intestine.
Causes: Helicobacter pylori infection and prolonged use of anti-inflammatory drugs.
7.Gallstones:
Solid Material Formation: Small pieces formed from digestive fluid in the gallbladder.
Chronic Diseases:
GERD (Chronic Acid Reflux):
Frequent Acid Backflow: Acid-containing contents in the stomach frequently leak into the esophagus.
Symptoms: Persistent heartburn and regurgitation.
2,Irritable Bowel Syndrome (IBS):
Colon Muscle Dysfunction: Irregular contractions leading to excessive gas, abdominal pain, and cramps.
Chronic Nature: A long-term condition affecting bowel function.
3.Lactose Intolerance:
Inability to Digest Lactose: Results in digestive discomfort after consuming milk and dairy products.
Common Symptoms: Bloating, gas, and diarrhea.
4.Diverticulosis and Diverticulitis:
Colon Pockets Formation: Diverticula (pockets) in the wall of the colon.
Complications: Inflammation (diverticulitis) can occur, causing pain and infection.
5.Gastrointestinal (GI) Cancers:
Tissue and Organ Affliction: Cancers affecting the digestive system, including esophageal, gastric, colorectal, pancreatic, and liver cancers.
6.Crohn’s Disease:
Inflammatory Bowel Disease (IBD): A lifelong condition causing inflammation in the digestive tract.
7.Celiac Disease:
Autoimmune Disorder: Gluten consumption damages the small intestine.
Trigger: Found in wheat, barley, and rye.
Care Practices for Digestive Health

Maintaining a healthy digestive system involves adopting proactive lifestyle and dietary habits:
1.Hydration:
Importance of Water: Drinking water facilitates smooth food flow, preventing dehydration-related constipation.
Dehydration Consequences: Insufficient water intake can lead to dry and hard stool.
2.Fiber-Rich Diet:
Benefits of Fiber: Supports digestion and regular bowel movements.
Soluble and Insoluble Fiber: Both types contribute to digestive health.
3.Balanced Nutrition:
Fruits and Vegetables: Multiple servings daily for essential vitamins and minerals.
Whole Grains: Choosing whole grains over processed grains.
Limiting Processed Foods: Reducing intake of processed and sugary foods.
4.Probiotics:
Role of Probiotics: Supporting a healthy gut microbiome.
Post-Antibiotic Use: Especially beneficial after antibiotic treatments.
5.Mindful Eating:
Chewing and Digestion: Thorough chewing aids in proper digestion.
Eating Pace: Slower eating allows the body to signal fullness.
6.Physical Activity:
Exercise and Digestion: Physical activity and gravity aid in moving food through the digestive system.
Post-Meal Walks: Taking a walk after meals can enhance digestion.
7.Avoiding Harmful Habits:
Alcohol and Smoking: Limiting alcohol intake to prevent acid-related issues.
Smoking Cessation: Quitting smoking improves digestive symptoms.
8.Stress Management:
Stress and Digestive Issues: Association between stress and conditions like constipation, diarrhea, and IBS.
Stress Reduction Techniques: Incorporating stress-relief practices into daily life.
Seeking Medical Attention
While occasional digestive issues are common, persistent symptoms warrant attention:
When to Contact a Healthcare Provider:
Frequent Symptoms: Constipation, diarrhea, vomiting, stomach pain, excessive gas, or heartburn.
Potential Underlying Issues: Frequent occurrences may indicate a more serious digestive system problem.
2.Importance of Medical Evaluation:
Diagnostic Assessment: Identifying the cause of persistent symptoms.
Early Intervention: Timely treatment prevents potential complications.
3.Collaborative Approach:
Healthcare Professional Guidance: Seeking advice on managing and preventing digestive issues.
Individualized Care: Tailoring interventions based on the individual’s health status and conditions.
Conclusion
In conclusion, understanding the details of the digestive system provides a foundation for promoting digestive health. The collaboration of organs in the GI tract and the biliary system highlights the complexity of the digestive process. Awareness of common conditions, care practices, and the significance of seeking medical attention empowers individuals to prioritize their digestive well-being. Adopting a holistic approach that combines a healthy lifestyle, balanced nutrition, and regular medical check-ups ensures a resilient and well-functioning digestive system, contributing to overall health and vitality.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for professional assistance.
H. pylori Infection

Introduction
Helicobacter pylori (H. pylori) infection is a significant global health concern, affecting a substantial portion of the world’s population. The discussion aims to provide an in-depth exploration of various aspects of H. pylori infection, including its prevalence, transmission, symptoms, diagnosis, treatment, complications, prevention strategies, and future research directions.
Prevalence and Transmission

H. pylori infection is widespread, with approximately two-thirds of the world’s population harboring the bacterium in their gastrointestinal tract. Various factors contribute to its prevalence, including socioeconomic status, living conditions, hygiene practices, and geographic location. The discussion indulges into the epidemiological trends of H. pylori infection across different populations and regions, highlighting disparities in prevalence rates and associated risk factors.
Transmission of H. pylori occurs primarily through interpersonal contact and ingestion of contaminated food or water. Saliva, fecal-oral transmission, and oral-oral transmission, including through kissing, are significant modes of spread. Poor sanitation and overcrowded living conditions facilitate the transmission of the bacterium, particularly in resource-limited settings. The discussion explores the mechanisms of H. pylori transmission and the implications for public health interventions aimed at reducing its spread.
Symptoms and Diagnosis

While many individuals with H. pylori infection remain asymptomatic, others experience a range of gastrointestinal symptoms, including stomach pain, bloating, nausea, and weight loss. The discussion elucidates the spectrum of clinical manifestations associated with H. pylori infection, emphasizing the importance of recognizing atypical presentations and considering differential diagnoses.
Diagnosing H. pylori infection presents several challenges due to the variability of symptoms and the limitations of available diagnostic tests. We critically evaluates the utility of different diagnostic modalities, including stool antigen tests, urea breath tests, and upper gastrointestinal endoscopy, in detecting H. pylori infection. It also examines the role of serological tests and molecular techniques in enhancing diagnostic accuracy and guiding clinical management decisions.
Treatment Options

The standard treatment regimens for H. pylori infection typically involve a combination of antibiotics and proton pump inhibitors (PPIs). However, rising rates of antibiotic resistance pose significant challenges to effective eradication therapy. It explores the mechanisms of antibiotic resistance in H. pylori and the implications for treatment outcomes.
Alternative treatment approaches, such as sequential therapy, concomitant therapy, and bismuth-based quadruple therapy, are also examined in the context of their efficacy and tolerability. Highlighting the importance of individualizing treatment regimens based on antibiotic susceptibility testing and patient-specific factors to optimize therapeutic outcomes.
Complications

Peptic ulcers are a common complication of H. pylori infection, resulting from the bacterium’s ability to disrupt the gastric mucosal barrier and induce inflammation. The discussion elucidates the pathophysiology of peptic ulcer formation and the factors contributing to ulcer recurrence and complications.
In addition to peptic ulcers, H. pylori infection is associated with an increased risk of more serious complications, such as gastric cancer and mucosa-associated lymphoid tissue (MALT) lymphoma. The discussion explores the molecular mechanisms underlying H. pylori-induced carcinogenesis and the strategies for early detection and management of gastric neoplasms.
Prevention

Preventive measures play a crucial role in reducing the burden of H. pylori infection and its associated complications. The discussion emphasizes the importance of promoting good hygiene practices, including handwashing and sanitation, to minimize the risk of transmission.
Furthermore, dietary factors may influence the risk of H. pylori infection and its clinical outcomes. The discussion evaluates the evidence regarding the impact of dietary habits, such as consumption of fruits, vegetables, and probiotics, on H. pylori colonization and disease progression. It also addresses the potential role of vaccination in preventing H. pylori infection and its complications, highlighting ongoing research efforts in vaccine development.
Research and Future Directions
Ongoing research efforts are focused on advancing our understanding of H. pylori pathogenesis, identifying novel therapeutic targets, and developing effective preventive strategies. The discussion highlights recent advancements in H. pylori research, including insights into bacterial virulence factors, host immune responses, and microbial interactions within the gastric microbiota.
Future directions in H. pylori research encompass a multidisciplinary approach, integrating molecular biology, epidemiology, immunology, and clinical medicine. The discussion outlines key areas for future investigation, such as the development of targeted antimicrobial agents, the role of host genetics in H. pylori susceptibility, and the impact of microbial dysbiosis on disease outcomes.
Conclusion
In conclusion, H. pylori infection remains a significant public health challenge, with implications for gastrointestinal health and disease worldwide. A comprehensive understanding of the epidemiology, pathogenesis, diagnosis, treatment, and prevention of H. pylori infection is essential for guiding clinical practice and informing public health policies. By addressing the complexities of H. pylori infection through interdisciplinary research and collaborative efforts, we can strive towards reducing its global burden and improving patient outcomes.
In managing H. pylori infection, compassion, empathy, and a holistic approach are crucial alongside clinical expertise. Striving for excellence in knowledge and practice enables us to advance gastroenterology and improve patient outcomes.
As we address H. pylori infection and its broader implications on gastrointestinal health, let’s remain dedicated to providing optimal patient care. By working collaboratively and embracing interdisciplinary approaches, we can positively impact lives and contribute to a healthier future.
Email expertassignment46@gmail.com to explore how we can assist you in achieving your academic and professional aspirations. Wishing you continued success in your medical journey.
10 Research Methods in Psychology

Psychology is a complex field that indulges into the realms of human behavior and mental processes. In the pursuit of understanding these aspects, psychologists employ a myriad of research methods, each tailored to unravel specific dimensions of the human psyche. Whether engaged in experimental investigations or qualitative explorations, these methodologies serve as invaluable tools for therapists, clinicians, and researchers aiming to decipher the complexities of the human mind.
Surveys
Surveys stand as stalwart instruments in the psychologist’s toolkit, facilitating the study of mental health disorders’ prevalence and causative factors. Offering both quantitative and qualitative insights, these inquiries employ random selection techniques to ensure a representative sample. The resultant data not only aids in comprehending human behavior but also serves as a cornerstone for crafting effective treatment strategies.
Tip: Craft well-structured questions and employ random sampling for robust and reliable results.

In the core of qualitative exploration, case studies emerge as profound investigations into the lives of individuals, groups, or communities. By immersing themselves in the core of a subject, psychologists gain miles perspectives on behavior and mental health. Beyond clinical applications, case studies find relevance in diverse fields such as finance, sales, and advertising, offering insights into consumer behavior and decision-making.
Tip: Combine multiple case studies for a comprehensive understanding and ensure triangulation for heightened reliability.
3. Experimental Study
Quantitative in essence, experimental studies play a main role in establishing causal relationships between variables. By manipulating independent variables and observing resultant changes in dependent variables, psychologists gain valuable insights into the external causes of behaviors, both in communities and broader societal contexts.
Tip: Prioritize random assignment for internal validity, strengthening the credibility of causal relationships.
4. Content Analysis:
Involving into the realm of text-based data, content analysis emerges as a powerful method for extracting patterns and themes from patient communication. Whether analyzing interview transcripts or business emails, this technique aids in the development of targeted psychological treatments and proves instrumental in forensic psychology when solving complex behavioral issues.
Tip: Ensure intercoder reliability to enhance the validity of your content analysis.

In the pursuit of synthesizing knowledge, psychologists turn to meta-analysis, a quantitative approach that combines findings from diverse studies. By consolidating information on a specific topic, meta-analysis serves as a comprehensive resource, offering recommendations for future research endeavors and advancing the frontiers of psychology.
Tip: Encompass studies with diverse methodologies for a robust and holistic analysis.
6. Correlational Research
Navigating the unknown landscape of nonexperimental methods, correlational research illuminates relationships between two variables. While not establishing causation, this approach is instrumental in identifying connections, prompting researchers to complement it with causal studies for more nuanced conclusions.
Tip: Clearly communicate the distinction between correlation and causation in research findings.
7. Quasi-Experiment
Akin to traditional experiments but devoid of random participant assignment, quasi-experiments find their niche in studying non-random traits. Particularly valuable when exploring innate qualities, this method enables psychologists to delve into traits that cannot be randomly assigned.
Tip: Transparently acknowledge the limitations associated with quasi-experiments, especially in terms of establishing causal relationships.

Capturing the essence of behavior in its natural habitat, naturalistic observation, a qualitative method, provides a nuanced understanding of how individuals behave in their accustomed settings. Beyond psychology, this method’s applications extend to diverse fields, including technology, sales, and business, offering insights for innovation.
Tip: Integrate naturalistic observation with other methods for a comprehensive grasp of human behavior.
9. Structured Observation
In the controlled environs of a laboratory, structured observation unfolds as a qualitative method to evaluate human behavior systematically. Applied extensively in clinical and medical research, this method aids in understanding how new therapies or medications influence patient behaviors.
Tip: Ensure the relevance of the structured setting to the behavior under scrutiny for heightened external validity.

Harnessing cutting-edge technology, neuroimaging serves as a quantitative method, unveiling the intricacies of the human brain. Techniques like CT scans and MRI enable psychologists to map brain functions, offering profound insights into the interplay between neural processes, thoughts, emotions, and behavior.
Tip: Stay abreast of technological advancements in neuroimaging for continually refined insights into brain activity.
Tips for Conducting Effective Research
Maintain Research Ethics: Uphold ethical standards, ensuring that both research teams and participants are well-versed in procedures, policies, and confidentiality agreements.
Apply the Scientific Method: Consistently adhere to the scientific method, facilitating organized data collection and analysis to enhance result accuracy.
Report Findings: Disseminate research, theories, and analysis within the scientific community. This not only fosters collaboration but also establishes professional authority in the field.
This comprehensive guide encapsulates the diverse array of research methods in psychology, illustrating their applications, nuances, and tips for effective execution. Whether through quantitative experiments or qualitative explorations, psychologists navigate the terrain of human behavior, contributing to the continual evolution of the field.
Wishing you all the best in your Psychology Research and related studies,
For any Challenges or Guidance during the education journey,
Email us at;williamsassignmenthelpfredrick@gmail.com
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science
The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work
Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader
A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
For Health Sciences Assignment Help,
Email us at,
williamsliason@outlook.com
What Are The Steps to Writing a Book Summary?

Writing a book summary is a valuable skill that enables you to convey the essence of a book concisely and effectively. Whether for academic purposes, book reviews, or personal use, a well-crafted summary captures the main ideas and key details without unnecessary elaboration. This comprehensive guide indulges into the detailed steps and provides examples for writing a book summary. It also integrates keywords to demonstrate how these resources can enhance the summary-writing process.
Step 1: Read the Book Carefully
Reading the book carefully is the foundation of writing a good summary. This step involves:
Active Reading: Engage with the text by asking questions and making connections to other readings or real-life situations.
Note-Taking: Highlight important passages and take notes on key events, character developments, and significant quotes.
Understanding the Context: Research the historical, cultural, and biographical context of the book to gain a deeper understanding of its themes and messages.
Step 2: Identify the Main Themes and Ideas
Identifying the main themes and ideas requires:
Theme Analysis: Look for recurring subjects or concepts throughout the book. Themes are often explored through the actions and experiences of the characters.
Character Analysis: Understand the motivations, growth, and conflicts of the main characters. How do they contribute to the overall themes?
Plot Analysis: Break down the plot into its essential components (exposition, rising action, climax, falling action, resolution) and see how each part contributes to the overall message.
Step 3: Create an Outline
Creating an outline helps organize your thoughts and ensures a logical flow in your summary. The outline should include:
Introduction: Briefly introduce the book’s setting, main characters, and initial situation.
Body: Divide the body into sections corresponding to the book’s major plot points. Include the rising action, climax, and falling action.
Conclusion: Summarize the resolution of the story and restate the main themes.
Step 4: Write the Summary
Writing the summary involves:
Conciseness: Avoid unnecessary details and focus on the main points. Each sentence should add value to the summary.
Clarity: Use clear and straightforward language. Ensure that your summary is easy to read and understand.
Accuracy: Make sure your summary accurately reflects the book’s content and the author’s intentions.
Step 5: Review and Revise
Reviewing and revising your summary ensures its quality. This process includes:
Checking for Errors: Correct any grammatical, spelling, or punctuation errors.
Improving Coherence: Ensure that your summary flows logically from one point to the next.
Enhancing Clarity: Rewrite any ambiguous or confusing sentences. Make sure that each point is clearly explained.
Conclusion
Writing a book summary is a multi-step process that involves careful reading, theme identification, outlining, writing, and revising. Utilizing tools and services like “summary maker Assignment Help,” “write my essay online,” “Write My Essay service,” “my assignment help,” and “online assignment help” can greatly enhance your ability to produce high-quality summaries. By following these steps and leveraging available resources, you can effectively convey the essence of any book. This skill not only contributes to academic success but also enhances your ability to critically engage with and communicate about various texts, making it an invaluable asset in both educational and professional contexts.
Expert Academic Assignment Help offers top-tier support for university students. Our services include expert assistance with essays, dissertations, assignments, research projects, and writing book summaries. Enhance your academic performance with our professional guidance and support.
For help and guidance, email us at: expertassignment46@gmail.com
The 12 Most Interesting Facts about Nursing

The nursing profession is a cornerstone of the healthcare system, rich in history, filled with unique facts, and bolstered by surprising statistics that highlight its evolution and impact. Whether you’re a registered nurse, nurse practitioner, nurse’s assistant, or involved in nurse staffing, there is always more to learn about this vital field. Here, we indulge into 12 intriguing facts about nursing that might surprise even those within the industry.
1. Nursing’s Ancient Origins

The earliest records of nursing date back to 300 A.D. in the Roman Empire, where nurses operated in what were considered hospitals at the time. These early healthcare institutions, known as valetudinaria, provided care primarily to soldiers and slaves. Nursing during this period was rudimentary and primarily focused on basic care and comfort.
The practice of nursing evolved significantly during the Middle Ages. Monastic orders, particularly in Europe, took on the role of caregivers. Monks and nuns provided care in hospices and infirmaries, laying the groundwork for modern nursing. The evolution continued with the establishment of more structured medical and nursing practices in response to the Black Death in the 14th century. These historical roots underscore the longstanding tradition of compassion and care in nursing.
2. Florence Nightingale’s Pioneering Influence

Florence Nightingale, often referred to as the founder of modern nursing, played a major role in transforming the profession. Born into a wealthy British family, Nightingale defied societal expectations to pursue a career in nursing. Her work during the Crimean War (1853–1856) brought her international acclaim. She was appalled by the unsanitary conditions and high mortality rates in military hospitals and implemented rigorous hygiene practices, significantly reducing the death rate.
Nightingale’s contributions extended beyond the battlefield. She established the Nightingale Training School for Nurses in 1860 at St. Thomas’ Hospital in London, emphasizing the importance of formal education and training for nurses. Her book, “Notes on Nursing: What It Is and What It Is Not,” became a seminal text in nursing education. Nightingale’s legacy includes her pioneering use of statistical analysis to advocate for healthcare reform, showcasing the impact of evidence-based practice.
3. The First Nursing School
The establishment of the Bellevue Hospital School of Nursing in New York City in 1873 marked a significant milestone in American nursing history. Inspired by Florence Nightingale’s principles, the school offered a one-year program that combined theoretical instruction with practical experience. This model set the standard for future nursing education.
Bellevue’s success prompted the establishment of other nursing schools, such as the New England Hospital for Women and Children (now part of the Boston Medical Center) and Massachusetts General Hospital’s nursing school. These institutions played a crucial role in professionalizing nursing and raising the standards of patient care. The emphasis on rigorous training and education helped transform nursing into a respected and essential profession.
4. The Physical Demands of Nursing
Nurses are known for their dedication and hard work, but the physical demands of the profession are often underestimated. On average, nurses walk four to five miles during a typical 12-hour shift, which is double the daily walking distance of most people. This constant movement is necessary to provide timely and effective care to patients, but it also highlights the physical challenges nurses face.
The demanding nature of nursing underscores the importance of proper footwear and ergonomics in the workplace. Comfortable, supportive shoes can help prevent injuries and reduce fatigue, enabling nurses to perform their duties effectively. Additionally, the physical activity associated with nursing contributes to overall health, but it also necessitates a focus on self-care and occupational health strategies to mitigate the risk of long-term musculoskeletal issues.
5. Dominance in Healthcare Education
Nursing is a dominant field within healthcare education, with approximately 50% of students in healthcare-related programs pursuing nursing degrees. This significant representation reflects the critical role nurses play in the healthcare system. The demand for nursing education has led to the development of numerous undergraduate and graduate programs, offering specialized training in various areas such as pediatric nursing, geriatric nursing, and critical care.
The strong support network among nursing students and professionals fosters a collaborative learning environment. Nursing programs emphasize not only clinical skills but also the development of critical thinking, communication, and leadership abilities. This comprehensive approach ensures that nursing graduates are well-prepared to meet the diverse and complex needs of patients.
6. Top Nursing Jobs
Nursing offers a wide range of career opportunities, and several nursing roles are consistently ranked among the top jobs in the United States. According to U.S. News & World Report, three nursing roles were among the top 40 jobs in 2021: registered nurses (ranked 37th), nurse anesthetists (ranked 39th), and nurse practitioners (ranked 3rd).
These rankings highlight the diverse and lucrative opportunities within the nursing profession. Registered nurses (RNs) are the backbone of healthcare, providing essential care and coordination in various settings. Nurse anesthetists, who administer anesthesia and monitor patients during surgical procedures, are highly specialized and command competitive salaries. Nurse practitioners (NPs) have advanced training that allows them to diagnose and treat medical conditions, often serving as primary care providers. The high ranking of NPs reflects the growing recognition of their critical role in expanding access to healthcare.
7. Mary Eliza Mahoney’s Legacy
Mary Eliza Mahoney, the first African American registered nurse in the United States, broke significant barriers in the field of nursing. Born in 1845 in Boston, Mahoney worked at the New England Hospital for Women and Children for 15 years before enrolling in its nursing program. She graduated in 1879, becoming one of only three graduates out of a class of 42.
Mahoney’s accomplishments extend beyond her personal achievements. She co-founded the National Association of Colored Graduate Nurses (NACGN) in 1908, advocating for the inclusion and recognition of African American nurses. The NACGN played a crucial role in supporting black nurses and promoting racial equality in the profession. Mahoney’s legacy is a testament to her resilience, dedication, and pioneering spirit, which continue to inspire nurses today.
8. The U.S. Nursing Workforce
As of 2020, there were approximately three million nurses in the United States, comparable to the population of Jamaica. This vast workforce is essential to the functioning of the healthcare system. Nurses work in a variety of settings, including hospitals, clinics, long-term care facilities, schools, and community health centers.
Globally, there are over 28 million nurses, accounting for 59% of healthcare professionals worldwide. This significant presence underscores the critical role nurses play in delivering healthcare services. However, the global nursing workforce faces challenges such as shortages, particularly in low- and middle-income countries. Efforts to address these shortages include increasing educational opportunities, improving working conditions, and supporting international collaboration.
9. Projected Growth in Nursing
The nursing field is not only large but also poised for continued growth. According to the U.S. Bureau of Labor Statistics, the employment of registered nurses is projected to increase by 7% from 2019 to 2029. This growth is driven by several factors, including an aging population, increased prevalence of chronic diseases, and expanded access to healthcare services.
The projected growth in nursing offers substantial opportunities for those entering the profession. It also underscores the importance of supporting nursing education and training programs to meet the demand for skilled nurses. Healthcare organizations and policymakers must invest in initiatives that attract and retain nurses, ensuring a robust workforce to provide high-quality care.
10. Diverse Work Environments
While hospitals remain the largest employer of nurses, the nursing profession offers diverse work environments. According to data from the U.S. Bureau of Labor Statistics, the distribution of nurses across various settings is as follows:
Hospitals: 60%
Ambulatory healthcare services: 18%
Nursing and residential care facilities: 7%
Government: 5%
Educational services: 3%
This diversity allows nurses to work in a range of settings, each with its unique challenges and opportunities. Ambulatory healthcare services include outpatient clinics, surgical centers, and primary care practices, where nurses play a vital role in patient care and health promotion. Nursing and residential care facilities provide long-term care for individuals with chronic illnesses or disabilities, emphasizing the importance of compassionate, ongoing support. Government and educational services offer roles in public health, policy, research, and academia, contributing to the advancement of the profession and the improvement of public health.
11. National Nurses Week
National Nurses Week, celebrated annually from May 6 to May 12, honors the challenging work and dedication of nurses. Established over 40 years ago, this week-long celebration culminates on May 12, the birthday of Florence Nightingale. The week recognizes the significant contributions of nurses to healthcare and society.
National Nurses Week includes various events and activities to celebrate and appreciate nurses. These may include educational seminars, award ceremonies, community outreach programs, and public awareness campaigns. The celebration provides an opportunity to highlight the vital role of nurses, advocate for their needs, and inspire the next generation of nursing professionals.
12. Staffing Agencies and Nursing Employment
Nurse staffing agencies play a crucial role in addressing the fluctuating demand for nursing services. Many nurses find employment through staffing agencies, which help them secure jobs and new opportunities. These agencies match nurses with healthcare facilities that need additional staff, ensuring that patient care remains uninterrupted.
For staffing agencies, keeping pace with the rising demand for nurses is crucial. Solutions like invoice factoring can provide the necessary funding to grow and support their operations effectively. Invoice factoring allows agencies to sell their accounts receivable at a discount in exchange for immediate cash, helping them manage cash flow and invest in recruiting and retaining qualified nurses.
Conclusion
These facts not only highlight the rich history and essential role of nursing but also underscore the profession’s ongoing evolution and the increasing opportunities within the field. Whether you’re a nurse or involved in nursing services, staying informed about these developments is key to advancing in this vital industry. The nursing profession continues to grow and adapt, driven by a commitment to providing high-quality care and improving patient outcomes.
For those involved in nurse staffing, understanding the dynamics of the nursing workforce and exploring financial solutions like invoice factoring can help meet the rising demand and ensure continued success. By recognizing the historical significance, current trends, and future prospects of nursing, we can better support and celebrate this indispensable profession.
For medical students and nurses of all categories, navigating assignments, homework, case studies, research, online classes, and challenging medical units can be daunting. Seeking professional guidance and assistance can make a significant difference in your academic and professional journey. For expert help with these challenges, consider reaching out to Expert Academic Assignment Help at expertassignment46@gmail.com Our professional support can help you excel in your studies and career.
What Is Pulmonary Embolism?

Introduction
Pulmonary embolism (PE) stands as a formidable medical concern, defined by the sudden obstruction of pulmonary arteries by blood clots or other substances. This obstruction poses a grave threat to life if not promptly addressed. In this comprehensive journey , we indulge into the technicality of PE, exploring its profound origins, clinical manifestations, predisposing factors, potential complications, and avenues for prevention.
A. Definition Pulmonary Embolism

Pulmonary embolism manifests when a blood clot, typically originating from deep vein thrombosis (DVT) in the lower extremities, migrates to the lungs, precipitating arterial blockage.
B. Significance
PE emerges as a critical condition, triggering significant impairment of pulmonary function and predisposing individuals to severe complications, including mortality, in the absence of timely intervention.
Symptoms of Pulmonary Embolism

A. Common Symptoms encompass acute dyspnea, chest pain, and syncope, often manifesting abruptly and varying in intensity.
B. Additional Symptoms: Patients may also present with hemoptysis, tachycardia, dizziness, diaphoresis, pyrexia, lower limb edema, and cyanosis, reflective of diverse physiological perturbation.
Causes and Risk Factors

a. Venous Thromboembolism
Predominantly, PE ensues from embolic occlusion secondary to thrombi originating in the deep venous system of the lower extremities.
b. Diverse Etiologies
PE may arise from fat emboli, tumor emboli, or air emboli, presenting a spectrum of etiological paradigms.
C. Predisposing Factors:
Notable risk factors encompass antecedent , underlying medical conditions (e.g., cardiovascular diseases, malignancies), surgical interventions, coagulopathies, prolonged immobility, and the prothrombotic milieu associated with COVID-19 infection
Complications of Pulmonary Embolism

a). Mortality:
Untreated PE poses a grave threat to life, with mortality rates approximating one-third of cases, underscoring the exigency of timely intervention.
b). Pulmonary Hypertension
Chronic embolic burden culminates in pulmonary hypertension, engendering elevated pulmonary arterial pressures and consequent cardiac strain.
C. Chronic Thromboembolic Pulmonary Hypertension
Persistent emboli precipitate vascular remodeling, culminating in a debilitating condition marked by enduring pulmonary hypertension and associated morbidities.
Prevention of Pulmonary Embolism
A. Pharmacological Prophylaxis
Anticoagulant prophylaxis stands as a cornerstone intervention in high-risk cohorts, mitigating thrombotic propensity perioperatively and during hospitalization.
B. Mechanical Modalities
Mechanical prophylaxis modalities encompass compression stockings, limb elevation, early mobilization, and pneumatic compression devices, fostering venous return and thwarting stasis-induced thrombogenesis.
C. Travel Recommendations
Travelers predisposed to thromboembolic events are counselled on hydration maintenance, periodic ambulation during prolonged periods of immobility, and the judicious utilization of compression garments to mitigate venous stasis during protracted journeys.
Conclusion
Pulmonary embolism emerges as a formidable adversary, demanding expeditious recognition and intervention to forestall catastrophic signal .A comprehensive grasp of its pathophysiological under happenings, clinical hallmarks, predisposing factors, complications, and preventive strategies is paramount for optimal management. Through concerted efforts encompassing risk mitigation and vigilant surveillance, individuals can navigate the perilous terrain of PE with greater resilience, minimizing morbidity and mortality associated with this grave condition.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for professional assistance.
14 Common Lung Diseases

Introduction
Lung diseases represent some of the most severe health threats globally. The rise of industrialization, environmental pollution, and tobacco usage significantly contribute to the prevalence of these diseases. This article, outlines the most common lung diseases, their symptoms, causes, and treatments.
1. Pneumonia

Pneumonia is an inflammation of the lung parenchyma caused by bacteria, viruses, fungi, or other pathogens. It poses a significant risk to the elderly, immunocompromised individuals, and those with chronic conditions but can also affect healthy individuals. Pneumonia can be classified based on the causative agent, such as bacterial pneumonia (e.g., Streptococcus pneumoniae), viral pneumonia (e.g., influenza virus), or fungal pneumonia (e.g., Pneumocystis jirovecii).
Symptoms
Fever
Cough with sputum
Chest pain
Shortness of breath
Fatigue
Sweating and shaking chills
Nausea, vomiting, or diarrhea (less common)
Diagnosis Diagnosis of pneumonia typically involves a combination of patient history, physical examination, chest X-rays, and sputum cultures. Blood tests may also be conducted to identify the causative agent.
Treatment Depending on the cause, treatments may include:
Antibiotics for bacterial pneumonia.
Antiviral medications for viral pneumonia.
Antifungal therapies for fungal pneumonia. Supportive care such as rest, fluids, and over-the-counter medications to reduce fever and manage pain can also alleviate symptoms. In severe cases, hospitalization may be required to provide intravenous antibiotics, oxygen therapy, or mechanical ventilation.
2. Bronchitis

Bronchitis involves the inflammation of the bronchial tubes, which carry air to and from the lungs. It can be acute, often following colds or the flu, or chronic, usually resulting from smoking or long-term exposure to irritants like pollution or dust.
Symptoms
Persistent cough (productive or dry)
Sputum production (clear, white, yellowish-gray, or green)
Fatigue
Shortness of breath
Slight fever and chills
Chest discomfort
Diagnosis Diagnosis typically involves a physical examination, where a doctor listens to the patient’s lungs with a stethoscope. Additional tests, such as a chest X-ray, sputum tests, or pulmonary function tests, may be conducted to rule out other conditions like pneumonia or asthma.
Treatment
Acute bronchitis: Symptomatic treatment includes rest, fluids, and over-the-counter pain relievers and cough medications. Inhalers or nebulizers may be prescribed to ease breathing.
Chronic bronchitis: Management may involve bronchodilators, steroids, and pulmonary rehabilitation. Smoking cessation and avoiding lung irritants are crucial for treatment.
3. Chronic Obstructive Pulmonary Disease (COPD)

COPD is a progressive, irreversible disease characterized by chronic inflammation of the airways, primarily due to smoking, environmental pollutants, or long-term exposure to respiratory irritants. COPD includes chronic bronchitis and emphysema, conditions that often coexist and lead to airflow obstruction.
Symptoms
Chronic cough
Sputum production
Shortness of breath, especially during physical activities
Wheezing
Chest tightness
Frequent respiratory infections
Fatigue
Unintended weight loss (in advanced stages)
Diagnosis COPD is diagnosed through a combination of patient history, physical examination, and spirometry, a test that measures the amount of air a person can exhale and how quickly they can do so. Chest X-rays, CT scans, and arterial blood gas analysis may also be used.
Prevention and Treatment Preventive measures include:
Smoking cessation
Vaccinations (influenza and pneumococcal vaccines)
Reducing exposure to lung irritants
Treatments involves;
Bronchodilators to relax the muscles around the airways
Inhaled steroids to reduce airway inflammation
Pulmonary rehabilitation programs
Oxygen therapy for severe cases
Surgery (e.g., lung volume reduction surgery or lung transplant) in advanced cases
4. Lung Cancer

Lung cancer involves the uncontrolled growth of malignant cells in the lung tissues. Major risk factors include smoking, exposure to secondhand smoke, exposure to carcinogens (e.g., asbestos, radon), and genetic predisposition.
Types
Small cell lung cancer (SCLC): Often linked to heavy smoking, SCLC is aggressive and spreads quickly.
Non-small cell lung cancer (NSCLC): More common and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Symptoms
Persistent cough
Chest pain
Weight loss
Hemoptysis (coughing up blood)
Shortness of breath
Hoarseness
Bone pain (in advanced stages)
Headache (if cancer spreads to the brain)
Diagnosis Diagnosis involves imaging tests (chest X-rays, CT scans, PET scans), sputum cytology, and tissue biopsy. Molecular testing may be done to identify specific genetic mutations that can be targeted with specific treatments.
Treatment
Surgery to remove the tumor or part of the lung
Chemotherapy to kill cancer cells
Radiation therapy to destroy cancer cells or shrink tumors
Targeted drug therapies to attack specific genetic changes in cancer cells
Immunotherapy to help the immune system fight cancer
5. Pleurisy
Pleurisy, or pleuritis, is the inflammation of the pleura, the tissue lining the lungs and chest cavity. It can be caused by infections (viral, bacterial, or fungal), injuries, autoimmune diseases (e.g., lupus, rheumatoid arthritis), or other underlying conditions.
Symptoms
Sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing
Shortness of breath
Cough
Fever (if infection is present)
Diagnosis Diagnosis involves a physical examination, chest X-rays, ultrasound, CT scans, and blood tests to identify the underlying cause. Thoracentesis, a procedure to remove and analyze pleural fluid, may be performed.
Treatment Treatment depends on the underlying cause and may include:
Antibiotics for bacterial infections
Antiviral medications for viral infections
Anti-inflammatory medications (e.g., NSAIDs) to reduce pain and inflammation
Pain management with medications
Thoracentesis to drain excess fluid from the pleural space
6. Pulmonary Embolism

A pulmonary embolism (PE) occurs when a blood clot, usually originating in the legs (deep vein thrombosis), travels to the lungs, blocking blood flow and causing tissue damage. Risk factors include prolonged immobility, surgery, cancer, and certain genetic conditions.
Symptoms
Sudden shortness of breath
Chest pain (may be sharp and worsen with deep breathing or coughing)
Cough (sometimes with bloody sputum)
Rapid or irregular heartbeat
Lightheadedness or dizziness
Leg pain or swelling (if DVT is present)
Diagnosis: Diagnosis involves imaging tests such as chest X-rays, CT pulmonary angiography, and ventilation-perfusion (V/Q) scans. D-dimer blood tests and ultrasound of the legs may also be conducted.
Treatment Immediate treatment includes:
Anticoagulants (blood thinners) to prevent further clotting
Thrombolytics (clot-dissolving medications) for severe cases
Surgical or catheter-based procedures to remove the clot
Long-term anticoagulation therapy to prevent recurrence
7. Pulmonary Edema

Pulmonary edema is the accumulation of fluid in the lung alveoli, making breathing difficult. It can result from heart failure (cardiogenic pulmonary edema), acute respiratory distress syndrome (ARDS), or exposure to high altitudes (non-cardiogenic pulmonary edema).
Symptoms
Difficulty breathing (dyspnea), especially when lying down
Rapid heartbeat (tachycardia)
Wheezing or gasping for breath
Coughing up frothy, pink-tinged sputum
Excessive sweating
Cyanosis (bluish skin or lips)
Diagnosis Diagnosis involves physical examination, chest X-rays, and blood tests. Echocardiography and pulmonary artery catheterization may be used to determine the underlying cause and severity.
Treatment Treatment involves addressing the underlying cause and may include:
Diuretics to remove excess fluid
Medications to improve heart function (for cardiogenic pulmonary edema)
Supplemental oxygen or mechanical ventilation
Treating underlying conditions such as infections or high altitude exposure
8. Pulmonary Fibrosis

Pulmonary fibrosis is the thickening and scarring of lung tissue, leading to reduced oxygen absorption. Causes include chronic exposure to environmental pollutants, infections, genetic factors, and autoimmune diseases (e.g., scleroderma).
Symptoms
Shortness of breath (dyspnea)
Persistent dry cough
Fatigue
Unexplained weight loss
Aching muscles and joints
Clubbing (widening and rounding) of the fingertips or toes
Diagnosis Diagnosis involves a combination of patient history, physical examination, imaging tests (chest X-rays, high-resolution CT scans), pulmonary function tests, and sometimes lung biopsy. Blood tests may be used to identify underlying autoimmune diseases.
Treatment While there is no cure for pulmonary fibrosis, treatments focus on symptom management and slowing progression:
Medications such as pirfenidone and nintedanib to slow disease progression
Oxygen therapy
Pulmonary rehabilitation
Lung transplant in severe cases
9. Pneumoconiosis
Pneumoconiosis is a lung disease caused by inhaling dust particles, such as asbestos, silica, or coal dust, leading to lung scarring. It is a type of occupational lung disease commonly seen in miners, construction workers, and industrial workers.
Symptoms:
Chronic cough
Shortness of breath
Chest tightness
Progressive loss of lung function
Diagnosis: Diagnosis involves a detailed occupational history, physical examination, chest X-rays, and CT scans. Pulmonary function tests may also be conducted to assess the extent of lung damage.
Treatment Treatment includes:
Avoiding further exposure to dust
Medications to manage symptoms, such as bronchodilators and corticosteroids
Respiratory therapies
Pulmonary rehabilitation
10. Pulmonary Arterial Hypertension (PAH)
PAH is a form of high blood pressure affecting the arteries in the lungs and the right side of the heart. It can be idiopathic, familial, or associated with other conditions such as connective tissue diseases, congenital heart disease, or chronic liver disease.
Symptoms
Breathing difficulties (dyspnea), especially during physical activities
Dizziness or fainting (syncope)
Chest pain
Fatigue
Swelling in the ankles, legs, and abdomen (edema)
Cyanosis (bluish lips and skin)
Diagnosis Diagnosis involves echocardiography, right heart catheterization, chest X-rays, and CT scans. Blood tests and pulmonary function tests may also be conducted to assess lung and heart function.
Treatment Treatment strategies include:
Medications to relax blood vessels and improve blood flow, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs
Diuretics to reduce fluid retention
Oxygen therapy
Anticoagulants to prevent blood clots
In severe cases, surgical procedures such as atrial septostomy or lung transplant
11. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene, leading to thick, sticky mucus buildup in the lungs and other organs. This results in frequent infections, respiratory issues, and digestive problems.
Symptoms
Persistent cough with thick mucus
Recurrent lung infections
Wheezing or shortness of breath
Poor growth and weight gain in children
Salty-tasting skin
Severe constipation
Frequent greasy, bulky stools
Diagnosis Diagnosis involves genetic testing, sweat chloride tests, and newborn screening. Pulmonary function tests, chest X-rays, and sputum cultures may also be conducted to assess lung health.
Treatment Management includes:
Medications to thin mucus, antibiotics to treat infections, and bronchodilators to open airways
Chest physiotherapy to clear mucus
Enzyme supplements and high-calorie diets to manage digestive issues
Newer therapies targeting the underlying genetic defect, such as CFTR modulators
12. Respiratory Distress Syndrome (RDS)
RDS primarily affects premature infants due to a lack of surfactant, a substance necessary to keep the lungs open and facilitate gas exchange. Risk factors include premature birth, maternal diabetes, and multiple births.
Symptoms
Rapid, shallow breathing
Grunting sounds while breathing
Nasal flaring
Chest retractions (pulling in of the chest muscles)
Cyanosis (bluish color of the skin and mucous membranes)
Diagnosis Diagnosis involves clinical assessment, chest X-rays, and blood gas analysis to measure oxygen and carbon dioxide levels. Prenatal tests can also help identify at-risk pregnancies.
Treatment Treatment includes:
Surfactant replacement therapy to improve lung function
Mechanical ventilation or continuous positive airway pressure (CPAP) to support breathing
Oxygen therapy
Supportive care such as fluids and nutrition
13. Sarcoidosis
Sarcoidosis is characterized by the growth of granulomas (small clusters of inflammatory cells) in the lungs and other organs, likely as an immune response to unknown triggers. The exact cause remains unclear, but genetic and environmental factors are believed to play a role.
Symptoms
Dry cough
Shortness of breath
Chest pain
Fatigue
Fever
Swollen lymph nodes
Skin lesions (e.g., erythema nodosum)
Diagnosis Diagnosis involves a combination of patient history, physical examination, chest X-rays, CT scans, and pulmonary function tests. Biopsy of affected tissues may be performed to confirm the presence of granulomas.
Treatment While sarcoidosis is often self-limiting and may resolve without treatment, severe cases may require:
Corticosteroids to reduce inflammation
Immunosuppressive medications (e.g., methotrexate, azathioprine)
Antimalarial drugs (e.g., hydroxychloroquine) for skin lesions
Regular monitoring and follow-up care to manage chronic cases
14. Asthma
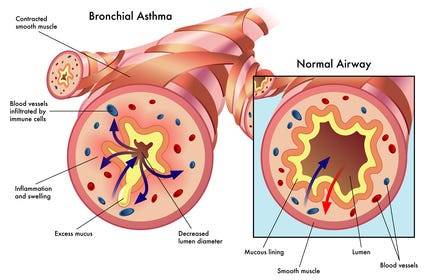
Definition and Causes: Asthma is a chronic inflammatory condition of the airways, causing episodes of wheezing, coughing, and chest tightness, often triggered by allergens, exercise, cold air, or respiratory infections. Genetic and environmental factors contribute to its development.
Symptoms
Wheezing
Shortness of breath
Chest tightness
Coughing, especially at night or early morning
Increased mucus production
Diagnosis: Diagnosis involves a detailed medical history, physical examination, and lung function tests (spirometry, peak flow measurement). Allergy testing and chest X-rays may also be conducted to identify triggers and rule out other conditions.
Treatment Management includes:
Avoiding known triggers
Inhalers (bronchodilators for quick relief, corticosteroids for long-term control)
Long-term control medications (e.g., leukotriene modifiers, long-acting beta agonists)
Immunotherapy (allergy shots) for severe allergies
Asthma action plans to manage symptoms and prevent attacks
Conclusion
Lung diseases encompass a wide range of conditions, each with distinct causes, symptoms, and treatments. Preventive measures such as avoiding smoking, reducing exposure to environmental pollutants, and timely vaccinations can significantly reduce the risk of developing many of these diseases. Early diagnosis and appropriate management are crucial in improving outcomes and quality of life for individuals affected by lung diseases. For personalized medical advice and treatment, consult with healthcare professionals.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: expertassignment46@gmail.com for professional guidance.
How Does The Brain Work?

The brain stands as a marvel of biological engineering, Composing of a multitude of bodily functions ranging from cognition and memory to emotions and sensory perception. Together with the spinal cord, it constitutes the central nervous system (CNS), the command center of the human body.
Composition of the Brain

Weighing approximately 3 pounds in adults, the brain’s main structure comprises about 60% fat, interspersed with water, protein, carbohydrates, and salts. Unlike muscles, it houses a complex network of blood vessels and nerves, including neurons and glial cells.
a) Gray and White Matter
Within the central nervous system, gray matter and white matter occupies distinct regions. In the brain, gray matter forms the outer layer, rich in neuron somas, while white matter constitutes the inner section, primarily composed of axons unsheathed in myelin. Conversely, in the spinal cord, this arrangement is reversed.
b) Brain Functionality
The brain operates by transmitting and receiving chemical and electrical signals throughout the body. These signals regulate a myriad of processes, with the brain disseminating each input. Some signals remain confined within the brain, while others traverse the spinal cord and nerves, disseminating information across the body’s expanse. This composes neural network relies on billions of interconnected neurons.
Major Brain Regions and Their Functions

1.Cerebrum
Dominating the brain’s landscape, the cerebrum encompasses the cerebral cortex and underlying white matter. It governs a spectrum of functions, including motor coordination, temperature regulation, language processing, emotional regulation, and sensory perception.
2. Brainstem
Serving as the bridge between the cerebrum and spinal cord, the brainstem comprises the midbrain, pons, and medulla. It regulates vital autonomic functions such as heart rate, breathing, and reflexive responses.
3. Cerebellum
Nestled at the posterior aspect of the brain, the cerebellum coordinates voluntary muscle movements, posture, balance, and motor learning.
Brain Coverings

a) Meninges
Three layers of protective membranes, collectively known as meninges, enshroud the brain and spinal cord. These layers — dura mater, arachnoid mater, and pia mater — shield the delicate neural tissue from physical trauma and infection.
b) Lobes of the Brain
Each hemisphere of the brain comprises four lobes, each harboring distinct functional domains:
Frontal Lobe: Governing executive functions, motor control, and higher cognitive processes.
Parietal Lobe: Integrating sensory information, spatial awareness, and perception of pain and touch.
Occipital Lobe: Specialized for visual processing and perception.
Temporal Lobe: Involved in auditory processing, language comprehension, and memory consolidation.
Deeper Brain Structures
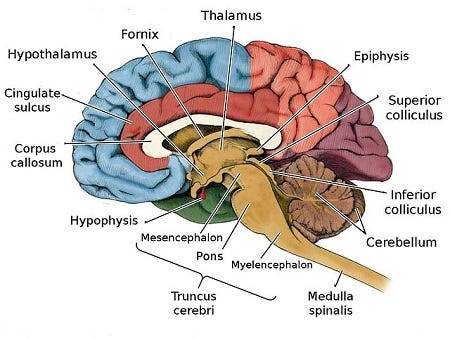
These encompass important structures such as the pituitary gland, hypothalamus, amygdala, hippocampus, and pineal gland, orchestrating hormone secretion, emotional regulation, memory consolidation, and circadian rhythms.
Blood Supply
The brain receives its oxygenated blood supply through the vertebral and carotid arteries, ensuring adequate perfusion of neural tissue. The main network of blood vessels, including the Circle of Willis, safeguards against ischemic insults and facilitates intraarterial communication.
Cranial Nerves

The twelve pairs of cranial nerves, originating from the brainstem, mediate a diverse array of sensory and motor functions, encompassing olfaction, vision, facial expression, and auditory perception.
Comprehending the anatomy and functionality of the brain fosters a deeper appreciation of its complexity and facilitates advances in neuroscientific research and therapeutic interventions aimed at diminishing neurological disorders.
Understanding the detailed anatomy and functionality of the brain is crucial for medical students embarking on their journey of study. Expert Academic Assignment Help offers invaluable assistance in navigating the complexities of neuroscience and related subjects. By leveraging expert guidance and support, students can excel in their medical education and contribute to advancements in the field of Medicine. Email us at expertassignment46@gmail.com to embark on your path to scholarly excellence and professional competency.
-
 infinite-dreamer520 liked this · 4 months ago
infinite-dreamer520 liked this · 4 months ago -
 jellybnzz liked this · 11 months ago
jellybnzz liked this · 11 months ago -
 expertacademicassignmenthelp reblogged this · 1 year ago
expertacademicassignmenthelp reblogged this · 1 year ago
