Gastroesophageal Reflux Disease
Gastroesophageal reflux disease

Introduction
Gastroesophageal Reflux Disease (GERD) is a chronic condition that affects the gastrointestinal system, leading to the regurgitation of the stomach contents into the esophagus. This discussion aims to explore the aspects of GERD, consisting its causes, symptoms, diagnostic methods, treatment modalities, potential complications, and preventative measures.
I. Causes and Risk Factors
GERD’s pathogenesis primarily generates from the malfunction of the lower esophageal sphincter, a muscular ring separating the esophagus from the stomach. When the lower esophageal sphincter muscle fails to close adequately, stomach contents, including corrosive acids, reflux into the esophagus. Various factors contribute to the development of GERD, ranging from lifestyle choices like alcohol consumption and smoking to physiological factors such as hiatal hernia, obesity, and pregnancy.
II. Symptoms and Manifestations
The symptoms associated with GERD present a spectrum of severity. The main symptom is heartburn, characterized by a burning sensation in the chest. Other prevalent manifestations include the feeling of food stuck behind the breastbone, regurgitation, cough, wheezing, difficulty swallowing, hiccups, hoarseness, and sore throat. Symptom acceleration often occurs during specific activities, such as bending over, lying down, or postprandial periods, with night time symptoms being particularly manifested.
III. Diagnostic Approaches
In cases where symptoms are mild, diagnostic tests may not be immediately necessary. However, persistent or recurrent symptoms may prompt healthcare providers to recommend an upper endoscopy for a detailed examination of the esophagus, stomach, and the initial segment of the small intestine. Additional diagnostic tools include tests measuring the frequency of stomach acid entry into the esophagus, esophageal manometry to assess pressure, and stool occult blood tests to identify potential bleeding.
IV. Treatment Strategies
Managing GERD involves various approaches, beginning with lifestyle modifications. Weight loss, raising up or tilting up the head of the bed, and refraining from lying down post meals constitute fundamental changes. Medications, including antacids, proton pump inhibitors (PPIs), and H2 blockers, are commonly prescribed for symptom relief. In cases resistant to conservative measures, anti-reflux surgery may be considered. Novel endoscopic therapies are emerging as additional options, backing up the evolving landscape of GERD treatment.
V. Prognosis and Potential Complications
While many individuals respond positively to lifestyle changes and medication, a subset may derail the ongoing treatment. Untreated or severe GERD can lead to complications, including exacerbation of asthma, Barrett’s esophagus with an increased risk of cancer, bronchospasm, chronic cough, dental issues, esophageal ulcers, and strictures. Understanding the potential complications emphasizes the importance of proactive management.
VI. When to Seek Medical Attention
Persistent or worsening symptoms despite lifestyle modifications or medication call for prompt medical attention. Warning signs such as bleeding, choking, rapid satiety, frequent vomiting, hoarseness, weight loss, and swallowing difficulties warrant immediate evaluation by healthcare professionals.
VII. Prevention Strategies
Preventing GERD involves a strict approach to lifestyle choices and recognizing potential risks. Maintaining a healthy body weight, adopting dietary modifications, and avoiding specific medications known to exacerbate GERD contribute to prevention. Educating individuals on lifestyle choices and risk factors empowers them to take preventive measures.
Conclusion
Gastroesophageal Reflux Disease is a complex and dynamic condition that demands a broad understanding of its manifestation for effective management. By revealing the various dimensions of GERD, from its underlying causes to treatment modalities and preventative strategies, healthcare professionals and individuals alike can collaboratively explore this challenging condition. A holistic and multidisciplinary approach ensures not only symptom relief but also addresses the long-term implications, promoting a better quality of life for those affected by GERD.
For Health Sciences Assignment Help,
Email us at,
williamsliason@outlook.com
More Posts from Expertacademicassignmenthelp and Others
Brain Tumor

Introduction
Brain tumors represent a complex and diverse group of neoplasms that arise from abnormal growth of cells within the brain or its surrounding structures. These tumors can vary widely in terms of their location, size, aggressiveness, and clinical presentation. Understanding the intricacies of brain tumors, including their diagnosis, treatment, and prognosis, requires a comprehensive approach that integrates medical expertise, advanced imaging modalities, and personalized therapeutic interventions.
Diagnosis of Brain Tumor

The diagnosis of a brain tumor typically begins with a thorough clinical evaluation, including a detailed medical history and neurological examination. Symptoms suggestive of a brain tumor may include persistent headaches, seizures, cognitive deficits, changes in behavior or personality, and focal neurological deficits such as weakness or sensory disturbances. However, it’s essential to recognize that many of these symptoms are nonspecific and can be caused by various other conditions.
To confirm the presence of a brain tumor and characterize its specific features, a variety of imaging studies and laboratory tests may be employed. These include computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET) scans. CT scans provide detailed cross-sectional images of the brain and are often the initial imaging modality used to assess patients with suspected brain tumors due to their widespread availability and rapid results. MRI, on the other hand, offers superior soft tissue contrast and is particularly useful for delineating the precise location and extent of brain tumors. In some cases, contrast-enhanced MRI with gadolinium-based contrast agents may be performed to enhance visualization of tumor tissue and surrounding structures.
Advanced MRI techniques, such as functional MRI (fMRI), magnetic resonance spectroscopy (MRS), and perfusion-weighted imaging (PWI), can provide additional information about the functional characteristics and metabolic activity of brain tumors. These modalities play a crucial role in treatment planning and assessing tumor response to therapy.
In select cases, a PET scan may be utilized to evaluate the metabolic activity of brain tumors and differentiate between benign and malignant lesions. PET imaging with radiopharmaceutical tracers such as fluorodeoxyglucose (FDG) can help identify areas of increased glucose metabolism, which are typically indicative of rapidly growing tumor cells. Additionally, molecular imaging techniques targeting specific biomarkers may offer insights into the molecular profile and biological behavior of brain tumors, facilitating personalized treatment strategies.
Tissue Sampling and Histopathological Evaluation: While imaging studies provide valuable information about the radiographic characteristics of brain tumors, definitive diagnosis often requires histopathological analysis of tissue samples obtained via biopsy or surgical resection. Tissue sampling allows for detailed microscopic examination of tumor cells, assessment of histological features, and determination of tumor grade, which plays a crucial role in prognostication and treatment planning.
Brain tumor grading is based on the World Health Organization (WHO) classification system, which stratifies tumors into different grades (I-IV) based on their histological features and biological behavior. Grade I tumors are typically slow-growing and well-differentiated, while grade IV tumors are highly aggressive and rapidly proliferating. Intermediate grades (II-III) exhibit varying degrees of aggressiveness and cellular atypia.
Prognostic Factors and Treatment Consideration

The prognosis of patients with brain tumors is influenced by various factors, including tumor type, grade, location, extent of resection, molecular characteristics, and patient-specific factors such as age and overall health status. High-grade tumors, such as glioblastoma multiforme, are associated with poorer outcomes compared to low-grade tumors, necessitating more aggressive treatment approaches.
Treatment strategies for brain tumors are highly individualized and may encompass a combination of surgical resection, radiation therapy, chemotherapy, targeted therapy, and supportive care measures. The goals of treatment are to achieve maximal tumor control while preserving neurological function and quality of life. Surgical resection is often the initial step in the management of operable brain tumors, with the aim of achieving gross total resection whenever feasible. However, the proximity of tumors to critical brain structures and eloquent areas may limit the extent of surgical resection and necessitate adjuvant therapies.
Surgical Management of Brain Tumor

Surgical approaches to brain tumor resection have evolved significantly with advances in neuroimaging, neurosurgical techniques, and intraoperative navigation systems. Traditional open craniotomy remains the standard approach for many brain tumors, allowing for direct access to the intracranial lesion. Microsurgical techniques, including the use of operating microscopes and intraoperative neuro navigation systems, enable precise tumor localization and maximal safe resection while minimizing damage to adjacent healthy brain tissue.
In recent years, minimally invasive approaches such as endoscopic endonasal surgery and keyhole craniotomy have gained popularity for select brain tumors, offering advantages such as smaller incisions, reduced surgical morbidity, and faster recovery times. Endoscopic techniques, in particular, allow for access to deep-seated lesions through natural orifices, such as the nasal cavity, thereby avoiding the need for extensive craniotomies and brain retraction.
Radiation Therapy for Brain Tumors

Radiation therapy plays a critical role in the management of both primary and metastatic brain tumors, offering precise and localized delivery of ionizing radiation to target tumor cells while sparing adjacent normal brain tissue. External beam radiation therapy (EBRT) is the most commonly utilized modality, utilizing high-energy X-rays or protons to deliver radiation to the tumor site over multiple treatment sessions. Techniques such as intensity-modulated radiation therapy (IMRT) and stereotactic radiosurgery (SRS) allow for highly conformal dose delivery, enabling escalation of radiation doses to the tumor while minimizing toxicity to surrounding critical structures.
In addition to conventional EBRT, brachytherapy techniques may be employed for selected cases, involving the placement of radioactive sources directly into or adjacent to the tumor cavity during surgical resection. This allows for localized delivery of high-dose radiation while minimizing exposure to healthy tissues. Proton therapy, a form of particle therapy, offers the advantage of improved dose conformity and reduced integral dose to surrounding tissues compared to conventional photon-based radiation therapy. Proton therapy is particularly beneficial for treating pediatric brain tumors and tumors located near critical structures, such as the optic nerves and brainstem.
Chemotherapy and Targeted Therapy: Chemotherapy plays a crucial role in the management of certain brain tumors, particularly high-grade gliomas and metastatic lesions. Chemotherapeutic agents may be administered orally, intravenously, or intracranially, either as monotherapy or in combination with other treatment modalities. The choice of chemotherapy regimen depends on factors such as tumor type, molecular characteristics, and patient-specific considerations.
Targeted therapy has emerged as a promising treatment approach for select brain tumors, leveraging the identification of specific molecular targets or pathways implicated in tumor growth and progression. Targeted agents may include small molecule inhibitors, monoclonal antibodies, or immunotherapeutic agents designed to selectively target tumor cells while sparing normal tissues. Biomarker-driven approaches, such as molecular profiling and genetic testing, help identify patients who are most likely to benefit from targeted therapies, enabling a personalized approach to treatment selection.
Recovery and Rehabilitation

Recovery following treatment for brain tumors often requires comprehensive rehabilitation efforts aimed at optimizing functional outcomes and quality of life. Physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation play important roles in addressing deficits related to motor function, activities of daily living, communication, and cognition. Additionally, psychosocial support services and caregiver education are essential components of the multidisciplinary care team, providing emotional support and practical assistance to patients and their families throughout the treatment and recovery process.
Conclusion
In conclusion, the management of brain tumors necessitates a multidisciplinary and individualized approach that integrates advances in diagnostic imaging, surgical techniques, radiation therapy, chemotherapy, targeted therapy, and supportive care interventions. Collaborative decision-making between patients, healthcare providers, and allied health professionals is paramount in optimizing treatment outcomes and enhancing quality of life for individuals affected by brain tumors. Ongoing research efforts aimed at elucidating the molecular mechanisms underlying tumorigenesis, identifying novel therapeutic targets, and refining treatment strategies offer hope for continued advancements in the field of neuro-oncology and improved outcomes for patients with brain tumors.
We wish you all the best in your medical education journey. In case you need any guidance or assistance during the learning process, do not hesitate to reach out to us.
Email at;
williamsassignmenthelpfredrick@gmail.com
How To Write A Dissertation Or Thesis

Writing a dissertation or thesis involves a structured process that requires careful planning and execution. Here’s a detailed discussion, covering the key steps in the dissertation writing process.
Step 1: Understand what a dissertation is.

A dissertation is a formal piece of research that follows the standard research process, involving four key steps:
Ask a specific, well-articulated research question(s): Clearly define the focus of your study.
Review existing literature: Explore what other researchers have said about your question.
Undertake your own research: Collect and analyze data in a scientifically rigorous fashion.
Answer your original question(s): Base your conclusions on your analysis findings.
Ensure that your dissertation is a formal piece of research, avoiding personal opinions or preconceived ideas.
Step 2: Find a unique, valuable research topic

Select a research topic that possesses three key attributes:
Clear: Clearly articulate what you plan to research, the questions you want to answer, and the context of your study.
Unique: Address questions that haven’t been answered before, or explore them in a specific context.
Important: Ensure that your research creates value, contributing to the field of research or industry.
Conduct thorough research to identify a topic that is both unique and valuable.
Step 3: Write a convincing research proposal

Craft a research proposal that convinces your university or committee of the worthiness of your research. Your proposal should include:
Clearly articulated, unique, and important topic: Justify why your research is significant.
Review of existing literature: Demonstrate that you’ve done enough reading to identify a clear gap for original research.
Provisional plan: Outline how you will collect and analyze data (methodology).
Show that you’ve done your homework and that your research is worthy of approval.
Step 4: Craft a strong introduction chapter

Use your approved proposal as the basis for your introduction chapter, which should include:
Brief background to the study: Explain the overall area of research.
Problem statement: Identify the problem with the current state of research.
Research questions: Outline the specific questions your study will seek to answer.
Significance of your study: Explain why your research is important and how its findings will be useful.
The introduction sets the scene for your research and justifies your research topic.
Step 5: Undertake an in-depth literature review

Go beyond initial literature review steps and create a comprehensive literature review chapter by:
Reading up: Deep dive into existing literature to understand the current state of research.
Writing up: Synthesize existing research, highlight a research gap, and use the literature to inform your methodology.
The literature review is the foundation on which your research is built.
Step 6: Carry out your own research

Design a research strategy and craft a methodology chapter that explains the “how” of your research:
Design your research strategy: Decide on your research philosophy, methodology, data collection, and analysis strategy.
Execute: Collect and analyze your data based on your research design.
Ensure your research design aligns with your topic, research questions, and data.
Step 7: Present your findings

Present your findings in two chapters — results and discussion. The results chapter should present processed data, while the discussion chapter provides your interpretation of the results:
Results chapter: Present processed data without interpretation.
Discussion chapter: Explain the story the data are telling and interpret the results in relation to your research questions.
Link your discussion back to your research questions outlined in the introduction.
Step 8: Draw a conclusion and discuss the implications

In the conclusion chapter, summarize key findings and discuss their implications:
Key findings: Highlight results directly related to your research questions.
Implications: Explain what your findings mean for industry or research in your area.
Bring your research full circle by answering the “what” and “so what?” questions.
Remember to check your university’s requirements for additional elements like the abstract, reference list, and appendices. Writing a dissertation is a detailed process, but by following these steps, you can craft a high-quality, well-structured document.
Wishing you all the best in writing your Dissertation, we hope this discussion will help.
Incase of any challenges or in need of Guidance during the academic journey;
Email us at;williamsassignmenthelpfredrick@gmail.com
How Does The Drug Got Excreted / Eliminated From The Body?

Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: expertassignment46@gmail.com
Your excellence our pride.
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science
The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work
Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader
A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
For Health Sciences Assignment Help,
Email us at,
williamsliason@outlook.com
Blood cell

The blood cells serves as a comprehensive guide to understanding the intricacies of hematopoiesis, the process through which various blood cell types are formed and function in the human body. This detailed discussion aims to unravel the key aspects presented in the article, delving into the structure, functions, and disorders associated with;
Red blood cells (erythrocytes),
2.White blood cells (leukocytes), and
platelets (thrombocytes).
Blood Cell Types and Composition
At the core of the circulatory system lie three major types of blood cells: red blood cells, white blood cells, and platelets. These cellular components collectively contribute to 45% of blood tissue by volume, with the remaining 55% being plasma. This delicate balance underscores the dynamic nature of blood, serving as a conduit for various vital functions within the body.
1.Red Blood Cells (Erythrocytes)
The discussion commences with a focus on red blood cells, the primary carriers of oxygen in the bloodstream. Erythrocytes, characterized by their unique biconcave shape and lack of a nucleus, play a crucial role in gas exchange facilitated by the iron-containing protein hemoglobin. The intricate details of erythropoiesis, the process of RBC formation in the red bone marrow, offer a glimpse into the remarkable physiological mechanisms that ensure a constant supply of oxygen carriers. The staggering production rate of 2.4 million RBCs per second in adults highlights the body’s continuous demand for these essential cells. The information regarding the lifespan of RBCs (100–120 days) and their subsequent removal by the spleen adds another layer to our understanding of the life cycle of these vital cells. The absence of a nucleus in mature red blood cells, a unique characteristic among human cells, is highlighted. The pathological conditions of anemia and polycythemia are thoroughly explored, shedding light on the consequences of an imbalance in red blood cell count. Additionally, the erythrocyte sedimentation rate (ESR) provides valuable insights into the diagnostic tools used in assessing the health of red blood cells.
2.White Blood Cells (Leukocytes)
The immune system, our body’s defense mechanism, relies on white blood cells to combat infectious diseases and foreign materials. These leukocytes, originating from multipotent cells in the bone marrow, are categorized into granulocytes (basophils, eosinophils, neutrophils, mast cells) and agranulocytes (lymphocytes and monocytes). The discussion delves into the roles these distinct white blood cell types play in the human immune system, offering a nuanced understanding of their functions. The conditions of leukopenia and leukocytosis, indicating low and high white blood cell counts, respectively, are explored, emphasizing the diagnostic significance of monitoring these counts. The increased white blood cell count during infections and its association with hematological cancers underscore the pivotal role leukocytes play in our overall health.
3.Platelets (Thrombocytes)
The section on platelets elucidates their role in hemostasis, the process of preventing and stopping bleeding. These small, irregularly shaped cell fragments, derived from megakaryocytes, circulate in the blood and are essential for the formation of blood clots. The average lifespan of platelets, a mere 5 to 9 days, emphasizes the continuous production required for maintaining hemostatic balance. The normal range of platelet counts and the potential consequences of low or high platelet numbers provide valuable insights into the delicate equilibrium necessary for preventing excessive bleeding or the formation of thrombosis. Thrombocytopathy, a broad term encompassing disorders related to platelets, is discussed, including thrombocytopenia, thrombasthenia, and thrombocytosis. The intricate relationship between platelets and growth factors, as well as their role in wound healing, showcases the multifaceted contributions of these small but crucial cellular fragments.
Complete Blood Count (CBC): The article introduces the Complete Blood Count (CBC) as a vital diagnostic tool providing a comprehensive analysis of blood cell composition. The historical transition from manual counting to automated analyzers reflects the evolving landscape of medical technology, enhancing the efficiency and accuracy of blood cell analysis. The significance of CBC in offering an overview of a patient’s general health status is underscored, emphasizing its widespread use in medical diagnostics.
Historical Discoveries.
The historical perspective woven into the article traces the evolution of our understanding of blood cells. From Jan Swammerdam’s pioneering observation of red blood cells in 1658 to Paul Ehrlich’s techniques in staining blood films and differential blood cell counting in 1879, the narrative highlights key milestones in the establishment of hematology as a distinct field of medicine. The contributions of various scientists, including Antoni van Leeuwenhoek, Alfred Donne, and Gabriel Andal, collectively shaped our current knowledge of blood cells.
Conclusion
The blood cells provides a rich tapestry of information encompassing their structure, functions, and associated disorders. It serves as a comprehensive resource for understanding the dynamic nature of blood and the pivotal roles played by red blood cells, white blood cells, and platelets in maintaining homeostasis within the human body. The integration of historical discoveries adds depth to the narrative, highlighting the continuous quest for knowledge that has defined the field of hematology. This article not only serves as an educational tool but also showcases the remarkable advancements in medical science and technology that have propelled our understanding of blood cells to new heights. As we unravel the mysteries of hematopoiesis, we gain valuable insights into the machinery that sustains life within our veins.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance.
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
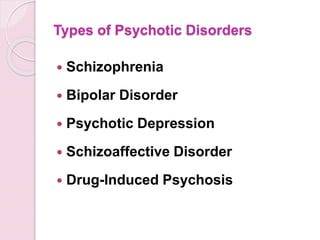
Types of Psychotic Disorders
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
The Pathophysiology and Therapeutic Intervention of Migraine

Introduction
Migraine, a prevalent neurological disorder characterized by recurrent headaches, sensory disturbances, and autonomic dysregulation, poses a significant global health burden. We are going to provide a comprehensive review citing out the unique pathophysiological mechanisms underlying migraine and discuss the evolving landscape of therapeutic interventions.
Understanding Migraine Pathophysiology

1. Genetic Predisposition
Migraine exhibits a strong familial aggregation, suggesting a genetic component in its etiology. Genome-wide association studies have identified numerous susceptibility loci implicated in migraine susceptibility, including genes involved in neuronal excitability, neurotransmitter release, and vascular regulation.
2.Environmental Factors
Environmental triggers such as stress, sleep disturbances, hormonal fluctuations, dietary factors, and sensory stimuli play a crucial role in migraine onset and exacerbation. These triggers interact with genetic predispositions to precipitate migraine attacks, underscoring the threshold nature of the disorder.
Sensory Processing Abnormalities
Migraine pathophysiology revolves around the concept of a cyclic sensory threshold model, wherein aberrant processing of sensory inputs leads to hypersensitivity and pain amplification. Dysregulation of cortical excitability, thalamocortical networks, and descending pain modulatory pathways contribute to the sensory manifestations of migraine.
Phases of Migraine

Migraine progression is characterized by distinct phases, including premonitory, aura, pain, and postdrome phase, each associated with specific neurophysiological changes. The premonitory phase, marked by various symptoms preceding the headache, reflects hypothalamic and brainstem activation. Aura, a transient neurological phenomenon, involves cortical spreading depression and cortical spreading depolarization, leading to visual, sensory, or motor disturbances. The pain phase, mediated by trigeminal vascular activation and central sensitization, culminates into headache and associated symptoms. The postdrome phase, characterized by residual symptoms following headache resolution, implicates persistent alterations in cortical and brainstem function.
a) Trigeminal vascular System

Central to migraine pathophysiology is the trigeminal vascular system, comprising peripheral trigeminal afferents and central brain nuclei involved in pain processing. Activation of trigeminal vascular pathways, mediated by neuropeptides like Calcitonin gene-related peptide, substance P, and neurokinin A, initiates neurogenic inflammation and sensitization of meningeal nociceptors, contributing to headache generation.
b) Brainstem Nuclei
Brainstem regions, including the dorsolateral pons, periaqueductal gray, and locus coeruleus, serve as crucial modulators of trigeminal vascular transmission. Dysregulation of brainstem nuclei leads to unbearable pain processing and autonomic dysfunction, characteristic of migraine attacks.
c) Hypothalamic Involvement
The hypothalamus plays an important role in migraine initiation and progression, integrating nociceptive, autonomic, and circadian inputs. Dysregulation of hypothalamic neurotransmitters, including orexin, serotonin, and dopamine, contributes to migraine susceptibility and triggers stress-induced attacks.
d) Thalamic Dysfunction
The thalamus, a key relay station in sensory processing, exhibits structural and functional abnormalities in migraine. Altered thalamocortical connectivity, thalamic excitability, and neurotransmitter imbalance contribute to central sensitization, photophobia, and allodynia, hallmark features of migraine.
e) Cortical Alterations
Beyond aura generation, the cerebral cortex demonstrates widespread abnormalities in migraineurs, including changes in cortical thickness, gray matter volume, and functional connectivity. Genetic variants associated with glutamatergic neurotransmission and cortical excitability further implicate cortical dysfunction in migraine pathophysiology.
Therapeutic Approaches

a) Acute Treatments
Triptans, serotonin receptor agonists, have long been the mainstay of acute migraine therapy. However, emerging classes of medications, including ditans and gepants, offer alternative treatment options with improved tolerability and efficacy. Lasmiditan, a selective 5-HT1F receptor agonist, provides rapid relief without vasoconstrictive effects, making it suitable for patients with contraindications to triptans. Gepants, small-molecule CGRP receptor antagonists, block CGRP-mediated vasodilation and neurogenic inflammation, offering effective pain relief without cardiovascular risks.
b) Preventive Treatments
Monoclonal antibodies targeting CGRP or its receptors represent a breakthrough in migraine prevention, providing sustained efficacy with monthly or quarterly dosing regimens. Erenumab, fremanezumab, and galcanezumab have demonstrated superior efficacy compared to placebo in reducing migraine frequency and severity, with favorable safety profiles. Gepants such as atogepant and Rimegepant offer additional options for migraine prophylaxis, particularly in patients intolerant to traditional preventive therapies.
c) Neuromodulation Techniques
Non-invasive neuromodulation modalities, including transcranial magnetic stimulation and transcutaneous supraorbital nerve stimulation, offer adjunctive therapeutic options for acute migraine management. TMS delivers magnetic pulses to cortical regions implicated in migraine pathophysiology, modulating cortical excitability and pain perception. tSNS targets the supraorbital nerve, inhibiting nociceptive transmission and providing rapid pain relief without systemic side effects. Additionally, vagus nerve stimulation (VNS) offers a promising approach for both acute and preventive migraine treatment, modulating autonomic function and central pain processing.
Conclusion
In conclusion, migraine represents a complex neurological disorder with a diverse clinical manifestations. Advances in our understanding of migraine pathophysiology have paved the way for the development of novel therapeutic agents targeting key molecular and neural pathways. By understanding the interplay between genetic predisposition, sensory processing abnormalities, and central pain modulation, clinicians can tailor treatment strategies to individual patient needs, optimizing therapeutic outcomes and improving quality of life for migraine patients worldwide. Continued research efforts and clinical innovations hold the promise of further advancements in migraine management, underscoring the collective commitment to alleviating the global burden of this devastating condition.
Understanding the pathophysiology of migraine is crucial for effective management, and this comprehensive analysis sheds light on the complex mechanisms underlying this neurological disorder. For medical students facing challenges in studying migraine or any other medical topic, seeking professional help from Expert Academic Assignment Help can provide valuable guidance and support. With our expert assistance, students can overcome obstacles and excel in their academic endeavors. Contact us at expertassignment46@gmail.com to elevate your understanding and mastery of medical concepts.
Why do students look for law assignment help?

Law courses demand significant reading and learning to pass tests and complete assignments successfully. Students face immense pressure while mastering various laws and statutes across different law topics such as criminal law, civil law, property law, and constitutional law, among others. The teaching methods employed by law schools add to the challenge. The Case Method, for instance, requires students to analyze a wide array of case proceedings and appellate level judicial opinions. This involves hours of reading and analysis to grasp the minutest details of each case. Additionally, the Socratic Method, where teachers evaluate students’ understanding by asking specific case-related questions in class, adds further pressure.

At Expert Academic Assignment Help, we provide a comprehensive six-step process to ensure high-quality, well-researched assignments free from plagiarism. Our process begins with the initial contact, where students describe their assignment details and deadlines. Once we understand the requirements, we provide a quotation and assign an academic writing expert who is competent in the subject matter. The expert conducts thorough research and gathers all necessary information before writing the assignment. After completion, the assignment undergoes a quality check to ensure it meets all requirements before being delivered to the student.
Moreover, we prioritize addressing any feedback from professors promptly, ensuring that students receive revised assignments as needed. Our efficient process ensures that assignments are completed within a short timeframe, typically within a day, depending on the assignment’s length and complexity.
Our law assignment help covers various fields, including but not limited to:
Administrative Law: Regulating government administrative bodies’ operations.
Contract Law: Governing legally binding agreements between parties.
Environment and Planning Law: Addressing issues related to environmental regulations and land use planning.
Family Law: Dealing with family dynamics, such as divorce and child custody.
Intellectual Property Law: Protecting innovations, ideas, and ownership rights.
Taxation Law: Enforcing taxation laws and regulations.
Constitutional Law: Governing the fundamental principles of government.
Criminal Law: Addressing criminal offenses and penalties.
Business Law: Managing legal issues related to business operations.
Bankruptcy & Insolvency Law: Handling bankruptcy filings and insolvency proceedings.
Property Law: Resolving property ownership and real estate issues.
Tort Law: Addressing legal blunders that cause harm or injury.
Civil Law: Resolving legal complications involving civilians.
Additionally, we assist students with case studies, which serve as self-learning tools to understand legal proceedings and develop a better understanding of the rules used in court.
In conclusion, law assignment help services play a crucial role in supporting students throughout their legal education journey. By providing expert guidance and assistance with assignments, these services alleviate academic pressure and enable students to focus on learning and achieving their academic goals effectively.
During your journey in the school of law, I wish you all the best in the process.
If you encounter any challenges and require guidance or assistance, do not hesitate to contact us at;
williamsassignmenthelpfredrick@gmail.com
Drug metabolism

Drug metabolism is a complex and vital process within living organisms, involving the metabolic breakdown of pharmaceutical substances through specialized enzymatic systems. These enzymatic pathways, collectively known as xenobiotic metabolism, play a pivotal role in pharmacology and medicine. The modification of the chemical structure of xenobiotics, including drugs and poisons, occurs through a set of metabolic pathways. The study of drug metabolism, known as pharmacokinetics, is essential for comprehending the duration, intensity, and actions of pharmaceutical drugs.
Phases of Drug Metabolism
The metabolism of drugs is a multi-phase process.
In phase I
Enzymes such as cytochrome P450 oxidases introduce reactive or polar groups into xenobiotics, thereby facilitating subsequent modifications.
Phase II
Involves conjugation reactions, where activated xenobiotic metabolites are conjugated with charged species, making them less active and more readily excretable. The final phase,
phase III
Encompasses further modification and excretion of conjugates, crucial for eliminating these compounds from cells.
Factors Influencing Drug Metabolism
Diverse factors influence drug metabolism, ranging from
1.physiological variables
Like age and sex differences to genetic polymorphisms affecting enzyme activity. The Cytochrome P450 monooxygenase system, predominantly present in the liver, plays a crucial role in determining the rate of metabolism.
2 .Pathological factors
Including diseases affecting organs like the liver, kidney, or heart, can significantly impact drug metabolism.
Detoxification Mechanisms
Detoxification mechanisms within the body are sophisticated, utilizing physical barriers like cell membranes and low-specificity enzymatic systems. While physical barriers restrict the entry of hydrophilic molecules, enzymatic systems possess broad substrate specificities, metabolizing a wide array of non-polar compounds. The detoxification of endogenous reactive metabolites, such as peroxides and reactive aldehydes, often involves specific enzymatic systems that recognize and remove these potentially harmful substances.
Beyond Human Health
Drug metabolism extends beyond human health; it is essential in environmental science, influencing the fate of pollutants during bioremediation processes. Moreover, in agriculture, xenobiotic metabolism in microorganisms, particularly enzymes like glutathione S-transferases, contributes to resistance against pesticides and herbicides.
In conclusion, drug metabolism is a multifaceted and indispensable aspect of pharmacology, significantly influencing the effectiveness and safety of pharmaceutical drugs. Understanding the intricacies of xenobiotic metabolism is crucial not only for medical professionals but also for addressing environmental and agricultural challenges. As research continues to unravel the mysteries of drug metabolism, its impact on human health and the broader ecosystem becomes increasingly apparent. The continuous exploration of drug metabolism is vital for advancing medical knowledge, ensuring drug safety, and addressing environmental concerns in the ever-evolving field of pharmaceutical science.
For Health Sciences Assignment Help;
Email us on;
williamsliason@outlook.com
Human musculoskeletal system.

Human musculoskeletal system, often referred to as the locomotor system, is a complex and integral component of human anatomy, enabling movement and providing structural support to the body. Comprising bones, muscles, cartilage, tendons, ligaments, and other connective tissues, this intricate system plays a crucial role in maintaining form, stability, and mobility. This comprehensive article aims to explore the various components and functions of the musculoskeletal system, addressing the nuanced interplay between bones, muscles, and joints. Additionally, it delves into the classification of bones, the functions of the skeletal system, the role of muscles in movement, and the clinical significance of this system. Understanding the musculoskeletal system is fundamental to appreciating its profound significance in human anatomy and physiology.
The Skeletal System:
At the core of the musculoskeletal system lies the skeletal framework, serving as the foundation for the attachment of tissues and organs. This section provides an in-depth exploration of the skeletal system, elucidating its dynamic structure, classifications of bones, and the critical functions they perform. From supporting the body’s shape to acting as a storage site for essential minerals such as calcium and phosphorus, bones play a multifaceted role. The controversies surrounding the number of bones in the human skeleton are addressed, emphasizing the dynamic nature of the skeletal system, which evolves from birth to maturity.
2.The Muscular System:
The musculoskeletal system’s functionality is inherently intertwined with the muscular system, comprising skeletal, smooth, and cardiac muscles. This section delves into the characteristics and roles of each muscle type, with a particular focus on the conscious control exerted by skeletal muscles. A comprehensive exploration of muscle contraction processes, initiation mechanisms, and the role of tendons in transmitting forces during contractions enriches our understanding of the system’s biomechanics. Recognizing the distinct attributes of cardiac and smooth muscles contributes to a holistic grasp of the musculoskeletal system’s dynamic nature.
3.Joints, Ligaments, and Bursae:
Movement within the musculoskeletal system is facilitated by joints, which connect bones and allow for a diverse range of motions. This section categorizes joints into diarthroses, amphiarthrosis, and synarthroses, elucidating their specific functions. A detailed examination of synovial joints, lubricated by synovial fluid, and the role of ligaments in limiting dislocation and controlling movement enhances our comprehension of joint dynamics. The significance of bursae, fluid-filled sacs providing cushioning around joints, is explored, emphasizing their role in minimizing friction and supporting efficient movement.
Clinical Significance:
The musculoskeletal system’s clinical significance extends to its susceptibility to disorders, impacting overall health. Diseases affecting this system can manifest as functional disorders, motion discrepancies, or complications arising from disorders in other body systems. This section explores the intricacies of musculoskeletal disorders, acknowledging the interconnections with the vascular, nervous, and integumentary systems that contribute to diagnostic challenges. Articular disorders are prevalent, but the musculoskeletal system is also affected by muscular diseases, neurologic deficits, toxins, endocrine abnormalities, metabolic disorders, infectious diseases, blood and vascular disorders, and nutritional imbalances. An exploration of inpatient procedures involving musculoskeletal interventions underscores the clinical importance of this system.
Conclusion:
In conclusion, the human musculoskeletal system stands as a marvel of biological engineering, orchestrating movement, providing support, and safeguarding vital organs. This comprehensive exploration, spanning bones, muscles, joints, and clinical significance, highlights the intricate interplay of various components that contribute to the system’s overall functionality. Despite the challenges posed by disorders and diseases, advancements in medical science, particularly in fields like rheumatology and orthopedic surgery, continue to enhance our understanding and treatment of musculoskeletal issues. Recognizing the complexity and clinical significance of this system is crucial for healthcare professionals in providing comprehensive care. As we delve deeper into the intricacies of the human body, the musculoskeletal system stands as a testament to the harmonious coordination of various components for the fundamental purpose of movement and stability. This expansive exploration serves as a valuable resource for those seeking a profound understanding of the human musculoskeletal system.
For Health Sciences Assignment Help,
email us on, williamsliason@outlook.com