10 Easy Ways To Tackle Homework
10 Easy Ways To Tackle Homework

1) Get Organized
Organization is the cornerstone of effective homework management. Invest in a comprehensive planner or digital calendar to meticulously document all upcoming tests, quizzes, and assignments. This proactive approach ensures you stay ahead of deadlines and fosters a sense of control over your academic responsibilities. Break down tasks further within your planner, creating a roadmap that transforms daunting assignments into manageable steps.
2) Set Aside a Specific Time for Homework

Time management is pivotal for academic success. Instead of relying on post-school fatigue to magically complete homework, establish a dedicated time slot. Whether it’s immediately after school or later in the evening, adhering to a consistent schedule fosters discipline and minimizes procrastination. This intentional approach transforms homework from a vague obligation into a structured routine, enhancing productivity and reducing stress.
3) Create a Study Space

Crafting an optimal study environment is crucial. Identify a quiet, distraction-free space conducive to focused work. If the home environment lacks tranquility, consider alternatives such as the library or a coffee shop. This deliberate selection of a study space sets the stage for effective learning, minimizing disruptions and maximizing concentration.
4) Break Up Your Work
The strategy of breaking down assignments into smaller, more manageable components is a cognitive game-changer. When faced with a complex task, such as writing an essay or preparing for a test, dissect it into distinct phases. Begin with brainstorming, progress to outlining, and conclude with the execution of the task. This method not only enhances efficiency but also promotes a systematic understanding of the subject matter.
5) Take Breaks

Recognizing the importance of mental rejuvenation, incorporate regular breaks into your study routine. Prolonged study sessions are not only counter productive but also mentally exhausting. Incorporate short breaks every 20 minutes to engage in mindless activities like scrolling through social media or enjoying a snack. This strategic pause boost your mental activities, contributing to sustained focus and overall well-being.
6) Get Rid of Distractions

A focused study environment demands the elimination of potential distractions. Beyond choosing a quiet space, actively remove devices and stimuli that may divert your attention. Put away your phone, turn off the television, and, if necessary, employ noise-canceling headphones. This intentional decluttering of your study space enhances concentration, allowing for a more immersive and efficient study experience.
7) Find a Study mate

Collaborative learning is a powerful tool in mastering challenging subjects. If you encounter difficulties in a particular class, seek out a study buddy. Choose a friend who shares the same class and is willing to engage in joint study sessions. This collaborative effort fosters an exchange of ideas, clarification of concepts, and mutual support. Don’t hesitate to consult your tutor if additional guidance is needed.
8) Make Use of Technology
Leverage the wealth of technological resources available to streamline your homework experience. Applications of technology provide organizational support, helping you keep track of assignments and due dates. Online platforms offer interactive learning tools, including practice problems and flashcards. Integrating technology into your study routine enhances efficiency and facilitates a dynamic approach to learning.
9) Reward Yourself

The psychology of reward plays a significant role in maintaining motivation. Upon completing your daily tasks, implement a system of rewards. These need not be extravagant; simple indulgences like watching an episode of your favorite TV show or enjoying a tasty treat can serve as effective incentives. This positive reinforcement not only makes the homework process more enjoyable but also cultivates a sense of accomplishment.
10) Get Enough Sleep

Undoubtedly, the foundation of cognitive well-being lies in adequate sleep. Prioritize a consistent sleep schedule, aiming for at least 8 hours each night. Sufficient sleep contributes to enhanced concentration, improved focus, and heightened energy levels. By valuing your sleep, you not only optimize your academic performance but also promote overall physical and mental health. Your homework endeavors, as well as your grades, will undoubtedly reflect the benefits of a well-rested mind.
Conclusion
Concluding the discourse on tackling homework emphasizes the transformative power of proactive and disciplined study habits. Acknowledging that homework need not be a source of stress, the conclusion underscores the importance of approaching assignments systematically. By starting early, maintaining consistency, and adopting these strategies, students can not only navigate homework efficiently but may even find a sense of enjoyment in the learning process. The message emphasizes that practice, routine, and a positive mindset are integral to mastering the art of homework.
In essence, the journey of tackling homework transcends the immediate completion of assignments; it becomes a holistic approach to academic growth and personal development. Each tip serves as a building block, constructing a foundation upon which students can handle the academic landscape with confidence and competence. Through these strategies, the once formidable task of homework is not merely conquered but transformed into a constructive and fulfilling endeavor.
For Homework or Assignments;
Email us at;
williamsassignmentheplfredrick@gmail.com
More Posts from Expertacademicassignmenthelp and Others
ORGANS OF EXCRETION

Excretion, a fundamental process in living organisms, plays a critical role in maintaining internal equilibrium and ensuring the efficient removal of waste products. This detailed discussion will involve deeper into the importance of excretion, the organs involved, their functions, and their contributions to overall health and homeostasis.
Importance of Excretion
Excretion is essential for the survival of all living organisms, from single-celled organisms to complex multicellular organisms like humans. It involves the elimination of metabolic waste products, toxins, and excess substances that accumulate within the body. By removing these waste materials, excretion helps regulate the internal environment, ensuring optimal conditions for cellular function and metabolic processes. Without effective excretory mechanisms, the buildup of waste products would lead to toxicity, impaired physiological function, and ultimately, organismal death.
Organs of Excretion
The human body employs a variety of organs for excretion, each with its own specialized functions and mechanisms for waste elimination. These organs include the skin, liver, large intestine, lungs, and kidneys. While some organs primarily eliminate specific types of waste products, others have multifunctional roles in metabolism, digestion, and detoxification, in addition to excretion.
1. Skin
The skin, the body’s largest organ, serves as a multifunctional barrier between the internal and external environments. In addition to its protective role, the skin participates in excretion through the production of sweat by sweat glands located in the dermis. Sweat, composed of water, salts, and urea, is released through sweat pores onto the skin’s surface, where it evaporates and helps regulate body temperature. Sweating also facilitates the elimination of metabolic wastes, toxins, and excess salts from the body, contributing to overall homeostasis.
2. Liver

The liver, a vital organ located in the upper right abdomen, is involved in numerous metabolic processes, including digestion, detoxification, and the synthesis of essential molecules. As part of its excretory function, the liver processes and eliminates various waste products and toxins from the bloodstream. It metabolizes ammonia, a toxic byproduct of protein metabolism, into urea, a less toxic compound that is excreted by the kidneys in urine. Additionally, the liver excretes bilirubin, a waste product of heme metabolism, into bile, which is then eliminated from the body through the feces.
3. Large Intestine

The large intestine, the final segment of the gastrointestinal tract, plays a crucial role in the absorption of water and electrolytes from undigested food residues. In addition to its role in digestion and water reabsorption, the large intestine serves as a site for the accumulation and elimination of solid waste materials. Bile pigments, such as bilirubin, are excreted into the gastrointestinal tract via bile and eventually eliminated in feces, contributing to the characteristic color of stool.
4. Lungs

The lungs, the primary organs of respiration, also play a role in excretion by removing gaseous waste products, such as carbon dioxide, from the bloodstream. During the process of cellular respiration, carbon dioxide is produced as a byproduct and transported via the bloodstream to the lungs for elimination. Through the process of gas exchange in the alveoli, carbon dioxide is expelled from the body during exhalation, helping to regulate blood pH and maintain acid-base balance.
5. Kidneys

The kidneys are often regarded as the primary organs of excretion in the human body, responsible for filtering waste products and excess substances from the bloodstream and producing urine for elimination. Each kidney contains millions of functional units called nephrons, which play a crucial role in the filtration, reabsorption, and secretion of various substances. Nephrons filter blood to remove waste products, such as urea, creatinine, and uric acid, while reabsorbing essential nutrients and maintaining electrolyte balance. The resulting urine is then transported from the kidneys to the urinary bladder via the ureters and excreted from the body through the urethra during urination.
6. Urinary System

The kidneys, along with the ureters, urinary bladder, and urethra, collectively form the urinary system, which functions to transport, store, and eliminate urine from the body. The ureters carry urine from the kidneys to the urinary bladder, where it is stored until it is expelled from the body through the urethra. The urinary system plays a crucial role in maintaining fluid balance, electrolyte concentration, and pH regulation within the body, thereby supporting overall homeostasis and physiological function.
Conclusion
In conclusion, excretion is a vital process that enables living organisms to eliminate waste products and maintain internal balance. Through the coordinated efforts of various organs, including the skin, liver, large intestine, lungs, and kidneys, the body effectively removes metabolic wastes, toxins, and excess substances, thereby supporting overall health and homeostasis. Understanding the mechanisms of excretion and the roles of excretory organs is essential for appreciating the complexity of physiological regulation and the interconnection of bodily systems. By studying excretory processes, researchers and healthcare professionals can gain insights into disease mechanisms, develop therapeutic interventions, and promote optimal health and well-being.
For students seeking guidance and assistance with their academic assignments, Expert Academic Assignment Help stands out as an invaluable resource. With their unique and top-notch content, they offer solutions to various academic challenges, ranging from essays to research papers ,Clinical case studies and homework. Don’t hesitate to reach out to them for expert assistance and take your academic journey to the next level. For inquiries, contact expertassignment46@gmail.com
10 Diseases of the Heart

Heart disease, a pervasive health concern, encompasses a spectrum of conditions affecting the cardiovascular system, from congenital defects to acquired disorders. According to the Centers for Disease Control and Prevention (CDC), it stands as the leading cause of death in the United States, claiming 1 in 4 lives. Understanding the intricacies of heart disease, including its types, symptoms, causes, treatments, preventive measures, and the overall outlook, is crucial for effective management and mitigation of its impact.
Types of Heart Disease:
1.Coronary Artery Disease (CAD):
Description: Arteries supplying blood to the heart become clogged with plaque.
Risk: Plaque can rupture, leading to a heart attack.
2. Congenital Heart Defects:
Description: Present at birth, affecting heart structure or connections.
Symptoms: May not be noticeable until a routine check.
3. Arrhythmia:
.Description: Irregular heartbeat due to faulty electrical impulses.
Types: Tachycardia (fast), Bradycardia (slow), Premature contractions, Atrial fibrillation.
4.Dilated Cardiomyopathy:
Description: Heart chambers dilate, weakening the heart muscle.
Causes: Past heart attacks, arrhythmias, toxins, and genetics.
5.Myocardial Infarction (Heart Attack)
Description: Blood flow interruption, damaging or destroying part of the heart muscle.
Causes: Plaque, blood clot, or artery spasms.
6.Heart Failure:
Description: Heart works inefficiently; can result from various heart-related conditions.
7.Hypertrophic Cardiomyopathy:
Description: Genetic thickening of heart muscle, affecting pumping ability.
Risk: Common cause of cardiac death in young individuals.
8.Mitral Valve Regurgitation:
Description: Mitral valve doesn’t close tightly, allowing blood back into the heart.
Complications: Enlarged heart, heart failure.
9.Mitral Valve Prolapse:
Description: Valve flaps of mitral valve bulge into the left atrium.
Prevalence: Affects around 2% of the population.
10.Aortic Stenosis:
Description: Narrowing of the aortic valve, hindering blood flow.
Causes: Congenital anomalies, calcium deposits, or scarring.
Symptoms of Heart Disease:
Symptoms vary based on the type but can include:
Angina (chest pain)
Difficulty breathing
Fatigue and lightheadedness
Swelling due to fluid retention
Cyanosis (blue skin) in congenital defects
Symptoms of a heart attack: chest pain, breathlessness, nausea, etc.
Causes and Risk Factors:
Genetic Causes:
Some heart diseases have a genetic basis.
Lifestyle Factors:
High blood pressure, high cholesterol, smoking, excessive alcohol intake, obesity, diabetes.
Other Factors
Age, history of preeclampsia during pregnancy, low activity levels, sleep apnea, stress, leaky heart valves.
Treatments:
Medications:
Anticoagulants, antiplatelet therapies, ACE inhibitors, beta-blockers, diuretics, etc.
Surgery:
Coronary artery bypass surgery, valve replacement or repair, repair surgery, device implantation, laser treatment, maze surgery.
Prevention:
. Lifestyle Measures:
. Balanced diet, regular exercise, maintaining a healthy weight, quitting smoking, limiting alcohol intake.
. Managing Underlying Conditions:
. Treating conditions like high blood pressure, obesity, and diabetes.
Outlook:
Overall Risk:
Common health problem; leading cause of death in the U.S.
Preventive Steps:
Many types are preventable through lifestyle changes and early intervention.
Conclusion:
Heart disease’s multifaceted nature demands a nuanced understanding for effective prevention and management. Regular medical checkups, healthy lifestyle choices, and awareness of symptoms contribute to better heart health. Early intervention and adherence to medical advice play key roles in improving outcomes for individuals with heart disease, reinforcing the importance of comprehensive education and public health initiatives.
For Health Sciences Assignment Help,
Email Us At;
williamsliason@outlook.com
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science

The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work

Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader

A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
How to Write Nursing Research Papers The process of nursing research paper writing involves exploring relevant issues within the field and proposing viable solutions. The complexity of nursing necessitates in-depth research, analytical thinking, and critical analysis. Topics may span various areas such as psychiatric nursing, healthcare management, evidence-based medicine, clinic hygiene, home-based healthcare, healthcare practices, and ethics, all of which revolve around the central goal of alleviating patient suffering and addressing their psychological well-being. Before delving into the writing process, it is crucial to determine the type of research paper – analytical or argumentative. Analytical research papers involve a specific analysis of issues or literary texts, employing designs like question/answer, comparison/contrast, problem/solution, cause/effect, hypothesis/proof, or change over time. On the other hand, argumentative research papers focus on presenting diverse viewpoints on a debatable issue, requiring an investigation of different studies to provide compelling arguments while addressing opposing views objectively. Selecting an appropriate topic is a critical aspect of the research paper process. The chosen topic should be specific, relevant to nursing, interesting to the writer, and within the prescribed length and format guidelines. Topics like Nursing Science During the 20th Century, Nurses’ Safety on the Working Place, or The Importance of Neonatal Care Nursing exemplify suitable choices. Once a topic is chosen, the next step involves sourcing information from reliable primary, secondary, and tertiary sources. Primary sources include original materials like academic journals, interviews, surveys, and court records. Secondary sources analyze or describe primary sources, encompassing books, articles, encyclopedias, dictionaries, and textbooks. Tertiary sources aid in organizing or locating both primary and secondary sources and typically involve databases and indexes. Pre-writing activities, such as brainstorming, freewriting, mindmapping, and outlining, play a pivotal role in organizing ideas before the actual writing process. These activities help in collecting and structuring major points and arguments effectively. In terms of formatting styles, the APA style is commonly used in nursing research papers. It dictates a specific structure with a title page, abstract, main body, and reference page. In-text citations follow a specific format with the author's last name and year of publication. The entire paper is typed in twelve-point Times New Roman font. The basic structure of a nursing research paper includes a title page containing the title, running head, author’s name, and institutional affiliation. The abstract, written on a separate page, provides a summary of key points, not less than 250 words, along with keywords. The main body comprises an introduction, body paragraphs addressing each point from the abstract with citations, and a conclusion restating the thesis and supporting arguments. The reference page, placed after the main body, lists all sources alphabetically with one-half inch indentation. Adhering to these guidelines ensures the creation of a well-structured and comprehensive nursing research paper. For further assistance contact us at williamsliason@outloock.com
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
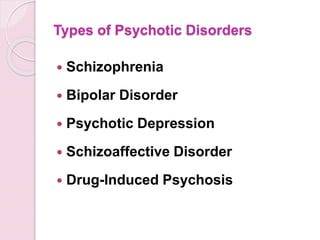
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
H. pylori Infection

Introduction
Helicobacter pylori (H. pylori) infection is a significant global health concern, affecting a substantial portion of the world’s population. The discussion aims to provide an in-depth exploration of various aspects of H. pylori infection, including its prevalence, transmission, symptoms, diagnosis, treatment, complications, prevention strategies, and future research directions.
Prevalence and Transmission

H. pylori infection is widespread, with approximately two-thirds of the world’s population harboring the bacterium in their gastrointestinal tract. Various factors contribute to its prevalence, including socioeconomic status, living conditions, hygiene practices, and geographic location. The discussion indulges into the epidemiological trends of H. pylori infection across different populations and regions, highlighting disparities in prevalence rates and associated risk factors.
Transmission of H. pylori occurs primarily through interpersonal contact and ingestion of contaminated food or water. Saliva, fecal-oral transmission, and oral-oral transmission, including through kissing, are significant modes of spread. Poor sanitation and overcrowded living conditions facilitate the transmission of the bacterium, particularly in resource-limited settings. The discussion explores the mechanisms of H. pylori transmission and the implications for public health interventions aimed at reducing its spread.
Symptoms and Diagnosis

While many individuals with H. pylori infection remain asymptomatic, others experience a range of gastrointestinal symptoms, including stomach pain, bloating, nausea, and weight loss. The discussion elucidates the spectrum of clinical manifestations associated with H. pylori infection, emphasizing the importance of recognizing atypical presentations and considering differential diagnoses.
Diagnosing H. pylori infection presents several challenges due to the variability of symptoms and the limitations of available diagnostic tests. We critically evaluates the utility of different diagnostic modalities, including stool antigen tests, urea breath tests, and upper gastrointestinal endoscopy, in detecting H. pylori infection. It also examines the role of serological tests and molecular techniques in enhancing diagnostic accuracy and guiding clinical management decisions.
Treatment Options

The standard treatment regimens for H. pylori infection typically involve a combination of antibiotics and proton pump inhibitors (PPIs). However, rising rates of antibiotic resistance pose significant challenges to effective eradication therapy. It explores the mechanisms of antibiotic resistance in H. pylori and the implications for treatment outcomes.
Alternative treatment approaches, such as sequential therapy, concomitant therapy, and bismuth-based quadruple therapy, are also examined in the context of their efficacy and tolerability. Highlighting the importance of individualizing treatment regimens based on antibiotic susceptibility testing and patient-specific factors to optimize therapeutic outcomes.
Complications

Peptic ulcers are a common complication of H. pylori infection, resulting from the bacterium’s ability to disrupt the gastric mucosal barrier and induce inflammation. The discussion elucidates the pathophysiology of peptic ulcer formation and the factors contributing to ulcer recurrence and complications.
In addition to peptic ulcers, H. pylori infection is associated with an increased risk of more serious complications, such as gastric cancer and mucosa-associated lymphoid tissue (MALT) lymphoma. The discussion explores the molecular mechanisms underlying H. pylori-induced carcinogenesis and the strategies for early detection and management of gastric neoplasms.
Prevention

Preventive measures play a crucial role in reducing the burden of H. pylori infection and its associated complications. The discussion emphasizes the importance of promoting good hygiene practices, including handwashing and sanitation, to minimize the risk of transmission.
Furthermore, dietary factors may influence the risk of H. pylori infection and its clinical outcomes. The discussion evaluates the evidence regarding the impact of dietary habits, such as consumption of fruits, vegetables, and probiotics, on H. pylori colonization and disease progression. It also addresses the potential role of vaccination in preventing H. pylori infection and its complications, highlighting ongoing research efforts in vaccine development.
Research and Future Directions
Ongoing research efforts are focused on advancing our understanding of H. pylori pathogenesis, identifying novel therapeutic targets, and developing effective preventive strategies. The discussion highlights recent advancements in H. pylori research, including insights into bacterial virulence factors, host immune responses, and microbial interactions within the gastric microbiota.
Future directions in H. pylori research encompass a multidisciplinary approach, integrating molecular biology, epidemiology, immunology, and clinical medicine. The discussion outlines key areas for future investigation, such as the development of targeted antimicrobial agents, the role of host genetics in H. pylori susceptibility, and the impact of microbial dysbiosis on disease outcomes.
Conclusion
In conclusion, H. pylori infection remains a significant public health challenge, with implications for gastrointestinal health and disease worldwide. A comprehensive understanding of the epidemiology, pathogenesis, diagnosis, treatment, and prevention of H. pylori infection is essential for guiding clinical practice and informing public health policies. By addressing the complexities of H. pylori infection through interdisciplinary research and collaborative efforts, we can strive towards reducing its global burden and improving patient outcomes.
In managing H. pylori infection, compassion, empathy, and a holistic approach are crucial alongside clinical expertise. Striving for excellence in knowledge and practice enables us to advance gastroenterology and improve patient outcomes.
As we address H. pylori infection and its broader implications on gastrointestinal health, let’s remain dedicated to providing optimal patient care. By working collaboratively and embracing interdisciplinary approaches, we can positively impact lives and contribute to a healthier future.
Email expertassignment46@gmail.com to explore how we can assist you in achieving your academic and professional aspirations. Wishing you continued success in your medical journey.
10 Simple Tips for Caring for Your Heart.

The heart, a tireless worker at the core of our well-being, demands our attention and care. As we navigate through Heart Health Month this February, let’s explore ten simple yet impactful tips to ensure our hearts thrive. These practices, ranging from physical activity to laughter and dental hygiene, collectively contribute to a holistic approach to cardiovascular wellness.
1.Cardiovascular Exercise: A Heart’s Best Friend
Engaging in regular cardiovascular or aerobic activities is fundamental for heart health. Following the American Heart Association’s recommendations of 75 minutes of vigorous exercise or 150 minutes of moderate-intensity exercise weekly can significantly boost cardiorespiratory fitness. Activities such as running, cycling, or brisk walking not only elevate heart rate but also enhance overall cardiovascular function. The rhythmic contraction and relaxation of muscles during exercise contribute to improved blood flow and reduced strain on the heart.
2.Embrace a Smoke-Free Lifestyle
Quitting smoking is a paramount step in safeguarding your heart. Smoking damages both the heart and blood vessels, escalating the risk of cardiovascular diseases. Additionally, avoiding second-hand smoke is crucial, as it has been linked to heart attacks and strokes. The harmful chemicals in tobacco smoke lead to the narrowing of blood vessels, increasing the workload on the heart and elevating the risk of high blood pressure.
3.Prioritize Quality Sleep
Adequate sleep, often underestimated, plays a pivotal role in heart health. With at least seven hours of nightly rest, blood pressure lowers, and the body undergoes essential repair processes. Research underscores the correlation between poor sleep and heightened risks of high blood pressure, subsequently increasing the likelihood of heart diseases. Establishing a consistent sleep routine and creating a conducive sleep environment are crucial steps in promoting optimal cardiovascular health.
4.Regular Checkups: A Heart-Healthy Habit
Consistent visits to the doctor for heart health checkups are essential. Assessing risk factors such as diet, blood pressure, cholesterol, and family history enables early detection and management of potential issues. A proactive approach to heart health empowers individuals to make informed lifestyle choices. Regular checkups also provide an opportunity for healthcare professionals to offer personalized guidance on maintaining heart health through tailored interventions.
5.Laughter: The Heart’s Natural Tonic
Laughing, whether through entertainment or social interactions, yields surprising benefits for the heart. The act of laughter reduces artery inflammation, lowers stress hormones, and increases levels of good cholesterol. Integrating humor into daily life becomes a delightful prescription for heart health. Laughter promotes the release of endorphins, the body’s natural feel-good chemicals, which contribute to overall well-being and stress reduction.
6.Dental Hygiene and Heart Connection
Surprising as it may seem, maintaining good dental hygiene contributes to heart health. Studies reveal a link between poor dental health and the presence of bacteria in the bloodstream, impacting heart valves. Simple practices such as regular brushing can significantly decrease the risk of cardiovascular disease. Furthermore, regular dental checkups not only preserve oral health but also serve as a preventive measure against potential cardiovascular complications.
7.Fuel Your Heart with a Healthy Diet
A heart-healthy diet rich in fruits, whole grains, vegetables, and legumes significantly improves blood pressure and cholesterol levels. Steering clear of salty foods and saturated fats is crucial, as they contribute to elevated blood pressure and increased bad cholesterol. Incorporating omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, further supports heart health by reducing inflammation and promoting optimal functioning of blood vessels.
8.Maintaining a Healthy Weight: A Heart’s Delight
Striving for and maintaining a healthy weight is a powerful defense against heart disease and high blood pressure. A combination of a balanced diet, regular exercise, and mindful calorie intake promotes overall well-being and cardiovascular health. Excess weight puts additional strain on the heart, leading to conditions such as hypertension and diabetes. Adopting sustainable lifestyle changes, including portion control and regular physical activity, contributes to achieving and sustaining a healthy weight.
9.Hydration: The Heart’s Elixir
Staying adequately hydrated is a simple yet often overlooked aspect of heart care. Considering the heart’s continuous effort in pumping around 2,000 gallons of blood daily, increased water intake supports its optimal functioning. Dehydration can lead to thicker blood, making the heart work harder to pump blood through the vessels. Maintaining proper hydration levels ensures the efficient transport of nutrients and oxygen to cells, promoting overall cardiovascular health.
10.Stay Active, Break Inactivity
Combatting sedentary lifestyles is crucial in preserving heart health. Incorporating simple changes like taking the stairs, walking, playing with pets, or engaging in household chores helps keep the heart active, reducing the risk of cardiovascular diseases. Prolonged sitting has been associated with various health risks, including obesity and heart disease. Regular physical activity not only supports cardiovascular health but also contributes to weight management and overall well-being.
In conclusion, adopting these ten heart-healthy habits provides a comprehensive approach to cardiovascular wellness. Whether it’s the joyous act of laughter, the discipline of regular exercise, or the mindfulness of a balanced diet, each step contributes to the harmonious symphony of a healthy heart. As we celebrate Heart Health Month, let’s embrace these practices and gift our hearts the care they deserve. Through consistent efforts and lifestyle modifications, we can ensure that our hearts continue to beat with vitality and resilience.
For health Sciences Assignment Help,
Email us on williamsliason@outlook.com
First Aid Instructions for 10 Medical Emergencies

Introduction:
First aid is the immediate care provided to a sick or injured person, often serving as a crucial bridge until professional medical help arrives. While formal first aid training is ideal, there are basic life-saving steps that everyone should be aware of. This article outlines first aid instructions for 10 common medical emergencies, along with practical tips and a comprehensive first aid kit list.
1.Stopped Heart (Cardiac Arrest):
In the event of a stopped heart, immediate action is crucial:
Initiate CPR (cardiopulmonary resuscitation) to maintain blood circulation.
Use an AED (automated external defibrillator) if available to shock the heart.
Call 911 and continue care until professional help arrives.
2. Bleeding:
Effective bleeding control is essential:
Apply direct pressure with a clean cloth or bandage to control bleeding.
Elevate the bleeding body part if possible to reduce blood flow.
Seek immediate medical help for severe bleeding.
3. Choking:
Swift response is vital when someone is choking:
Perform the Heimlich maneuver for a conscious choking victim.
If unconscious, initiate CPR and call for help.
Monitor airway and breathing.
4. Burns:
Proper handling of burns is crucial for minimizing damage:
Stop the burning process by cooling the burn with running water.
For minor burns, use a light gauze bandage and avoid breaking blisters.
Seek medical attention for severe burns.
5. Blisters:
Appropriate care can aid in the healing of blisters:
Leave small, unopened blisters alone to promote healing.
For larger, painful blisters, clean, drain, and apply antibiotic ointment.
Monitor for signs of infection.
6. Broken Bone/Fracture:
Careful management of fractures is essential:
Call 911 for severe fractures and avoid moving the person if a spinal injury is suspected.
Immobilize the injured area with a splint, elevate, and apply a cold pack for pain.
Seek prompt medical attention.
7. Sprains:
Proper first aid can alleviate symptoms of sprains:
Rest the injured limb, apply a cold pack, and elevate if possible.
Seek medical attention for severe pain, inability to bear weight, or signs of infection.
Follow R.I.C.E. (Rest, Ice, Compression, Elevation) principles.
8. Nosebleeds:
Effective nosebleed management is essential:
Lean forward and pinch the nose just below the bridge to control bleeding.
Apply a cold pack and seek medical attention for persistent or frequent nosebleeds.
Address underlying causes such as dry air or trauma.
9. Frostbite:
Timely response is critical to treating frostbite:
Get out of the cold and gradually warm the affected area with warm water.
Avoid rubbing the affected area, and do not use dry heat sources.
Seek medical attention for severe cases.
10. Bee Sting:
Proper care for bee stings is vital, especially for allergic reactions:
Remove the stinger immediately using a straight-edged object.
Monitor for signs of an allergic reaction and call 911 if necessary.
Clean the area, apply a cold pack, and use antihistamines for swelling.
First Aid Kit List:
A well-prepared first aid kit is an essential tool for handling emergencies. The kit should include:
Adhesive bandages in various sizes and shapes
Gauze pads and compress dressings
Adhesive cloth tape, latex gloves, and antiseptic wipes
Antibiotic ointment and hydrocortisone ointment
A breathing barrier for performing CPR
Instant cold compress, tweezers, and an oral thermometer
Emergency blanket for warmth and comfort
Conclusion:
While formal first aid training is highly recommended, understanding the basics of immediate care can make a significant difference in emergencies. The outlined first aid instructions cover a range of medical situations, and having a well-stocked first aid kit further enhances preparedness. Quick and appropriate action can be a crucial factor in saving lives during medical emergencies. Remember, being informed and ready can make you a valuable first responder in times of need.
For Health Sciences Assignment Help;
Email Us At;
williamsliason@outlook.com
The Endocrine System

Introduction
The endocrine system is a complex network containing a symphony of hormonal interactions crucial for maintaining physiological equilibrium. Comprising glands, organs, and tissues dispersed throughout the body, its influence allows various bodily functions, spanning from metabolism to reproduction and beyond. This topic endeavors to provide an in-depth exploration of the endocrine system, encompassing its anatomy, physiological functions, associated conditions, and strategies for proactive care. By indulging into this indispensable regulatory system, we aim to equip readers with a comprehensive understanding to prioritize their hormonal health effectively.
Anatomy of the Endocrine System
The anatomy of the endocrine system is contained by an array of specialized glands, organs, and tissues, each endowed with the capacity to synthesize and dispatch hormones into the bloodstream. Principal among these are:
Endocrine Glands: These specialized tissues, including the pituitary gland, thyroid gland, and adrenal glands, secrete hormones directly into circulation, exerting systemic effects.
Endocrine Organs: Organs such as the hypothalamus, pancreas, and reproductive glands contribute to hormonal regulation, interfacing closely with the nervous system to modulate physiological responses.
Endocrine-Related Tissues: Adjunct to traditional endocrine structures, adipose tissue, kidneys, and even the heart harbor the capability to produce hormones, further augmenting the system’s complexity and regulatory capacity.
Functions of the Endocrine System
The cardinal function of the endocrine system is hormone secretion, holding up varied network of intercellular communication. Hormones, acting as molecular messengers, traverse the bloodstream to target cells, eliciting diverse physiological responses.
Key functions include:
Metabolism Regulation: Hormonal content govern metabolic processes, dictating energy expenditure, glucose homeostasis, and lipid metabolism.
Homeostatic Control: Endocrine signaling regulates internal threshold, modulating blood pressure, fluid balance, and body temperature.
Development and Growth: Hormonal interplay underpins growth trajectories and developmental milestones, steering embryonic stages and pubertal maturation.
Sexual Function and Reproduction: Hormonal modulation governs reproductive physiology, controlling fertility, libido, and secondary sexual characteristics.
Neuroendocrine Integration: The endocrine system reveals intimately with the nervous system, harmonizing behavioral and physiological responses, including mood regulation and sleep-wake cycles.
Conditions and Disorders
A spectrum of endocrine-related ailments afflicts individuals, stemming from hormonal imbalances, glandular dysfunctions, or neoplastic proliferations. Noteworthy conditions encompass:
Diabetes and Metabolic Disorders: Spanning type 1 and type 2 diabetes, metabolic syndrome, and obesity, these conditions disrupt glucose homeostasis and metabolic equilibrium.
Endocrine Cancers and Tumors: Malignancies affecting endocrine tissues, including adrenal tumors, pituitary adenomas, and thyroid malignancies, necessitate specialized oncological management.
Thyroid Dysfunction: Hypo- and hyperthyroidism, thyroid nodules, and autoimmune thyroiditis typify prevalent thyroid disorders, precipitating diverse clinical manifestations.
Reproductive and Sexual Health Disorders: From polycystic ovary syndrome (PCOS) to erectile dysfunction, disruptions in reproductive hormone signaling manifest as infertility, menstrual irregularities, and sexual dysfunction.
Proactive Care and Health Maintenance
In fostering endocrine wellness, a holistic approach integrating lifestyle modifications and environmental awareness is imperative. Strategies for promoting endocrine health encompass:
Lifestyle Optimization: Embracing a balanced diet, regular exercise regimen, and adequate sleep hygiene fosters metabolic resilience and hormonal equilibrium.
Environmental Vigilance: Mitigating exposure to endocrine-disrupting chemicals pervasive in everyday products, such as plastics, pesticides, and personal care items, reduces the risk of hormonal perturbations.
Health Surveillance: Individuals with familial predispositions to endocrine disorders benefit from proactive screening and vigilant symptom monitoring, facilitating early intervention and optimal disease management.
Conclusion
The endocrine entails physiological regulation, producing hormonal interactions essential for vitality and well-being. By looking at anatomy, physiological functions, associated conditions, and avenues for proactive care, this discourse endeavors to foster a comprehensive understanding of the endocrine system Empowered with knowledge, individuals can prioritize their hormonal health, embracing proactive measures to optimize their overall well-being and quality of life.
For medical students navigating the study of endocrinology and seeking guidance and academic support during their study period, Expert Academic Assignment Help offers invaluable assistance. With our expertise and resources, we provide tailored solutions to aid in comprehension, research, and academic success. Don’t hesitate to reach out to us for personalized assistance and elevate your understanding of this vital field. Your academic journey awaits, and we’re here to help you excel.
Contact us at expertassignment46@gmail.com for professional assistance,
Atherosclerosis

Introduction
Atherosclerosis is a chronic and progressive condition characterized by the accumulation of plaque within the walls of arteries, leading to their hardening and narrowing. Despite being often asymptomatic in its early stages, atherosclerosis poses significant risks to cardiovascular health and can result in severe complications such as heart attacks, strokes, and peripheral artery disease (PAD). Therefore, comprehensive knowledge of its symptoms, causes, prevention strategies, diagnosis methods, and treatment options is imperative for effectively managing its impact on individuals’ well-being.
Symptoms of Atherosclerosis

Atherosclerosis typically advances silently, with symptoms only becoming apparent as arteries become significantly obstructed or when a cardiovascular event occurs. The manifestation of symptoms varies depending on the affected arteries, each presenting distinct clinical presentations:
Coronary Arteries: The narrowing of coronary arteries due to atherosclerosis can lead to symptoms such as arrhythmia (irregular heartbeat), angina (chest pain or pressure), and shortness of breath, especially during physical exertion.
Cerebral Arteries: Atherosclerosis affecting cerebral arteries may manifest as numbness or weakness in the limbs, difficulty speaking or understanding speech, drooping facial muscles, paralysis, severe headache, or vision problems, indicating a heightened risk of stroke.
3. Peripheral Arteries: Individuals with atherosclerosis in peripheral arteries may experience symptoms such as leg pain when walking (intermittent claudication), numbness, cold extremities, aching or burning sensations in the feet, and slow-healing wounds or infections, reflecting compromised blood flow to the extremities
4. Renal Arteries: Atherosclerosis affecting renal arteries can result in elevated blood pressure (hypertension) and eventual kidney failure, highlighting the systemic impact of arterial narrowing on vital organ function.
Causes and Stages of Atherosclerosis

The development and progression of atherosclerosis involve a series of intricate biological processes initiated by damage to the endothelium, the delicate inner lining of arteries. As plaque composed of cholesterol, fat, calcium, and inflammatory substances accumulates within arterial walls, the disease progresses through distinct stages:
Damage to the Endothelium: The initial stage of atherosclerosis is characterized by injury to the endothelial cells lining the arteries, often attributed to risk factors such as high cholesterol, hypertension, inflammation, obesity, diabetes, and smoking.
2. Formation of Fatty Streaks: Following endothelial damage, the infiltration of low-density lipoprotein (LDL) cholesterol into the arterial wall triggers an inflammatory response, leading to the formation of fatty streaks — the earliest visible signs of atherosclerosis.
3 . Development of Fibrous Plaques: Over time, the accumulation of cholesterol-laden foam cells and the proliferation of smooth muscle cells contribute to the formation of fibrous plaques, which protrude into the arterial lumen and impede blood flow.
4 . Formation of Complicated Lesions: Advanced atherosclerosis is characterized by the formation of complicated lesions, where unstable plaques prone to rupture expose thrombogenic components, leading to the formation of blood clots and subsequent cardiovascular events such as myocardial infarction or ischemic stroke.
Risk Factors for Atherosclerosis
Numerous modifiable and non-modifiable risk factors influence the development and progression of atherosclerosis, underscoring the multifactorial nature of the disease. These risk factors include:
High Cholesterol: Elevated levels of LDL cholesterol, commonly referred to as “bad” cholesterol, promote the deposition of cholesterol within arterial walls, contributing to plaque formation and atherosclerosis progression.
2. High Blood Pressure: Hypertension exerts mechanical stress on arterial walls, accelerating endothelial damage and promoting atherosclerosis development
3. Inflammation: Chronic inflammatory conditions, such as rheumatoid arthritis or systemic lupus erythematosus, exacerbate endothelial dysfunction and foster plaque formation within arteries.
4. Obesity: Excess adiposity predisposes individuals to metabolic abnormalities, including dyslipidemia and insulin resistance, which fuel atherosclerosis progression.
5. Diabetes: Both type 1 and type 2 diabetes mellitus increase the risk of atherosclerosis by inducing endothelial dysfunction, promoting inflammation, and accelerating the formation of advanced glycation end-products (AGEs) implicated in vascular
6. Smoking: Tobacco smoke contains toxic compounds that promote endothelial injury, oxidative stress, and inflammation, exacerbating the progression of atherosclerosis and increasing the risk of cardiovascular events.
7.Sedentary Lifestyle: Physical inactivity contributes to metabolic derangements, including obesity, dyslipidemia, and insulin resistance, fostering atherosclerosis development and cardiovascular risk.
8. Family History of Heart Disease: Genetic predisposition plays a significant role in atherosclerosis susceptibility, with familial clustering of cardiovascular risk factors amplifying the likelihood of disease manifestation.
9. Poor Diet: Diets rich in saturated fats, trans fats, refined carbohydrates, and excess sodium promote dyslipidemia, hypertension, and endothelial dysfunction, fueling atherosclerosis progression.
9 .Stress: Chronic stress triggers sympathetic nervous system activation and cortisol release, contributing to hypertension, inflammation, and atherosclerosis development
10. Sleep Apnea: Obstructive sleep apnea, characterized by recurrent episodes of upper airway obstruction during sleep, disrupts normal cardiovascular function and exacerbates atherosclerosis progression.
Identifying and addressing these risk factors through targeted interventions and lifestyle modifications are essential for mitigating the burden of atherosclerosis and reducing the risk of cardiovascular events.
Diagnosis and Treatment of Atherosclerosis

Accurate diagnosis and effective management of atherosclerosis require a multidisciplinary approach involving clinical evaluation, imaging studies, and laboratory testing. Diagnostic modalities utilized in the assessment of atherosclerosis include:
Physical Examination: Healthcare providers perform a comprehensive physical examination, assessing vital signs, auscultating for abnormal heart sounds or bruits, and palpating for peripheral pulses to evaluate cardiovascular health.
Imaging Tests: Various imaging modalities are employed to visualize arterial anatomy, assess plaque burden, and identify areas of stenosis or occlusion. These includes;
Angiography: Intravascular contrast dye is utilized to visualize arterial lumens and detect areas of stenosis or occlusion via X-ray imaging.
Ultrasound: Non-invasive ultrasound techniques, such as carotid ultrasound or abdominal ultrasound, enable the assessment of arterial wall thickness, plaque morphology, and blood flow characteristics.
Computed Tomography (CT) Angiography: CT angiography provides detailed anatomical imaging of arterial structures, facilitating the identification of atherosclerotic lesions and assessing their severity.
Magnetic Resonance Angiography (MRA): MRA employs magnetic resonance imaging (MRI) techniques to generate high-resolution images of blood vessels, aiding in the evaluation of arterial stenosis, plaque composition, and hemodynamic parameters.
3. Laboratory Evaluations: Blood tests are conducted to assess lipid profiles, inflammatory markers, and other biochemical parameters associated with cardiovascular risk. These include
Lipid Profile: Measurement of serum lipid levels, including total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides, provides insight into atherosclerosis risk and treatment efficacy.
Inflammatory Markers: Assessment of inflammatory biomarkers, such as C-reactive protein (CRP) or interleukin-6 (IL-6), aids in risk stratification and monitoring disease activity in individuals with atherosclerosis.
Blood Glucose: Screening for abnormal glucose metabolism, including fasting blood glucose and hemoglobin A1c (HbA1c) levels, helps identify individuals at risk of diabetes-associated atherosclerosis complications
4. Functional Tests: Functional assessments, such as stress testing or ankle-brachial index (ABI) measurement, are performed to evaluate cardiovascular function and assess the impact of atherosclerosis on tissue perfusion.
Once diagnosed, the management of atherosclerosis encompasses various approach targeting risk factor modification, pharmacological intervention, and, when indicated, invasive procedures to alleviate arterial obstruction and prevent cardiovascular events.
Treatment strategies for atherosclerosis include:
Lifestyle Modifications: Lifestyle interventions form the cornerstone of atherosclerosis management, emphasizing dietary modifications, regular physical activity, smoking cessation, stress reduction, and weight management to optimize cardiovascular health and mitigate disease progression.
Medication Management: Pharmacological therapy plays a pivotal role in atherosclerosis treatment, targeting modifiable risk factors such as dyslipidemia, hypertension, and inflammation. Commonly prescribed medications include
Statins: HMG-CoA reductase inhibitors, such as atorvastatin or simvastatin, reduce LDL cholesterol levels and stabilize atherosclerotic plaques, lowering the risk of cardiovascular events.
Antihypertensive Agents: Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, and calcium channel blockers are utilized to control blood pressure and mitigate endothelial dysfunction in individuals with hypertension-associated atherosclerosis.
Antiplatelet Therapy: Aspirin and other antiplatelet agents, such as clopidogrel or ticagrelor, inhibit platelet aggregation and reduce the risk of thrombotic events in individuals with established atherosclerosis or high cardiovascular risk.
Antidiabetic Medications: Oral hypoglycemic agents, insulin, or glucagon-like peptide-1 (GLP-1) receptor agonists are prescribed to achieve glycemic control and minimize the risk of diabetes-related atherosclerosis complications.
3. Invasive Procedures: In cases of severe arterial stenosis or symptomatic atherosclerotic disease refractory to medical therapy, invasive interventions may be warranted to restore arterial patency and alleviate ischemic symptoms. These include:
Percutaneous Coronary Intervention (PCI): Angioplasty with or without stent placement is performed to widen narrowed coronary arteries and improve myocardial perfusion in individuals with coronary artery disease (CAD).
Coronary Artery Bypass Grafting (CABG): Surgical revascularization using autologous or synthetic conduits bypasses obstructed coronary vessels, restoring blood flow to ischemic myocardial territories in patients with multivessel CAD or left main coronary artery disease.
Carotid Endarterectomy: Surgical removal of atherosclerotic plaque from carotid arteries reduces the risk of stroke in individuals with significant carotid stenosis and a history of transient ischemic attacks (TIAs) or cerebrovascular events.
Peripheral Arterial Interventions: Endovascular procedures, such as angioplasty, stenting, or atherectomy, are performed to treat lower extremity arterial disease and alleviate claudication symptoms in patients with peripheral artery disease (PAD).
Secondary Prevention Strategies: Beyond acute management, secondary prevention measures aim to prevent recurrent cardiovascular events and minimize disease progression through comprehensive risk factor modification, medication adherence, and ongoing surveillance of disease activity
Prevention of Atherosclerosis

Preventive strategies for atherosclerosis focus on addressing modifiable risk factors and promoting cardiovascular health through lifestyle modifications, health education, and targeted interventions. Key components of atherosclerosis prevention include:
Healthy Lifestyle: Encouraging individuals to adopt a healthy lifestyle characterized by balanced nutrition, regular physical activity, adequate sleep, stress management, and avoidance of harmful habits such as smoking or excessive alcohol consumption is paramount for reducing atherosclerosis risk
2. Dietary Modifications: Emphasizing a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and unsaturated fats while limiting intake of saturated fats, trans fats, cholesterol, sodium, and added sugars helps optimize lipid profiles, blood pressure, and overall cardiovascular health.
3. Physical Activity: Promoting regular exercise and physical activity is essential for maintaining cardiovascular fitness, weight management, insulin sensitivity, and endothelial function, thereby reducing the risk of atherosclerosis and its complications.
4. Tobacco Cessation: Implementing tobacco cessation programs and providing support for smoking cessation initiatives are critical for reducing atherosclerosis risk and improving overall cardiovascular outcomes.
5. Stress Management: Teaching stress reduction techniques such as mindfulness meditation, yoga, deep breathing exercises, or cognitive-behavioral therapy empowers individuals to cope with stressors effectively and mitigate their detrimental effects on cardiovascular health.
5 . Health Education: Educating individuals about the risks associated with atherosclerosis, the importance of early detection, and the benefits of preventive measures fosters informed decision-making and empowers individuals to take proactive steps towards cardiovascular wellness.
6. Regular Screening: Encouraging regular medical checkups and health screenings enables early detection of cardiovascular risk factors, facilitating timely intervention and personalized risk stratification for individuals at heightened risk of atherosclerosis.
Conclusion
In conclusion, atherosclerosis represents a significant public health challenge with far-reaching implications for cardiovascular morbidity and mortality. By majoring on the pathophysiology of atherosclerosis, identifying modifiable risk factors, and implementing evidence-based preventive strategies, healthcare providers can effectively mitigate the burden of atherosclerotic disease and promote cardiovascular health across diverse populations. Empowering individuals with knowledge, facilitating lifestyle modifications, and fostering a collaborative approach to atherosclerosis prevention and management are essential steps towards achieving optimal cardiovascular outcomes and enhancing quality of life for individuals affected by this pervasive condition.
As you navigate the complexities of cardiovascular health, remember that support and guidance are always available. Seek assistance from Expert Academic Assignment Help whenever needed.
Your journey in medicine is about more than just acquiring knowledge — it’s about embodying compassion, empathy, and continuous learning. Together, let’s strive for optimal cardiovascular health for all.
Email us at expertassignment46@gmail.com
Wishing you success and fulfillment in your medical journey.