The Pathophysiology Of Hypertension
The pathophysiology of hypertension

Introduction
Hypertension, or high blood pressure, is a complex medical condition affecting a significant proportion of the global population. Despite its prevalence, there remains uncertainty regarding its pathophysiology, with essential hypertension constituting a substantial portion where no single identifiable cause is found. This comprehensive discussion aims to delve into the physiological mechanisms involved in the development of hypertension, exploring factors such as cardiac output, peripheral resistance, the renin-angiotensin-aldosterone system, the autonomic nervous system, endothelial dysfunction, genetic factors, and intrauterine influences.
Cardiac Output and Peripheral Resistance

Maintaining normal blood pressure relies on the delicate balance between cardiac output and peripheral vascular resistance. Essential hypertension often involves a normal cardiac output but elevated peripheral resistance, primarily determined by small arterioles. The role of smooth muscle cells, calcium concentration, and structural changes in arteriolar vessel walls contribute to the irreversible rise in peripheral resistance.
Renin-Angiotensin System

The renin-angiotensin system plays a crucial role in blood pressure regulation. Renin, released in response to various stimuli, initiates the conversion of angiotensinogen to angiotensin I, which is then converted to the vasoconstrictor angiotensin II. This system also stimulates aldosterone release, promoting sodium and water retention. While the circulating system may not be directly responsible for essential hypertension, local renin-angiotensin systems in organs like the kidney, heart, and arterial tree gain significance in regulating regional blood flow.
Autonomic Nervous System

Sympathetic nervous system stimulation affects arteriolar constriction and dilation, playing a pivotal role in maintaining normal blood pressure. Although the exact role of epinephrine and norepinephrine in hypertension etiology remains unclear, drugs blocking the sympathetic nervous system demonstrate therapeutic efficacy.
Endothelial Dysfunction

Vascular endothelial cells, producing vasoactive agents like nitric oxide and endothelin, play a key role in cardiovascular regulation. Endothelial dysfunction, implicated in essential hypertension, involves impaired production of nitric oxide. This dysfunction, once established, becomes irreversible, highlighting its primary nature in hypertension.
Vasoactive Substances

Various vasoactive substances, such as bradykinin, endothelin, atrial natriuretic peptide, and ouabain, influence sodium transport and vascular tone. These substances contribute to the delicate balance in maintaining normal blood pressure.
Genetic Factors
Genetic predisposition significantly contributes to hypertension, with specific mutations linked to disorders like Liddle’s syndrome, glucocorticoid-remediable aldosteronism, and others. The intricate interplay of multiple genes makes it challenging to pinpoint individual contributions.
Intrauterine Influences
Fetal influences, particularly birth weight, emerge as determinants of adult blood pressure. The Barker hypothesis suggests a link between low birth weight, metabolic abnormalities, and hypertension in later life. However, the role of genetic factors in this relationship requires further exploration.
Diastolic Dysfunction

Hypertensive left ventricular hypertrophy leads to impaired diastolic relaxation, affecting ventricular input during exercise. This dysfunction contributes to increased atrial pressure, pulmonary congestion, atrial fibrillation, and potential complications like pulmonary edema.
Conclusion
In conclusion, understanding the pathophysiology of hypertension involves exploration of various physiological mechanisms. While essential hypertension remains a complex and often multifactorial condition, advancements in research shed light on factors such as cardiac output, peripheral resistance, the renin-angiotensin system, the autonomic nervous system, endothelial dysfunction, genetic influences, and intrauterine factors. A comprehensive understanding of these elements is crucial for developing effective therapeutic strategies and preventive measures against the global burden of hypertension.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for professional assistance.
More Posts from Expertacademicassignmenthelp and Others
Leukemia in Children

Introduction
Leukemia in children presents a formidable challenge, demanding meticulous management and treatment. This detailed discussion aims to devolve into various facets of childhood leukemia, encompassing its definition, types, causes, risk factors, symptoms, diagnosis, treatment modalities, potential complications, preventive measures, and strategies for supporting a child living with leukemia.
Understanding Leukemia in Children
1. Definition
Leukemia is a hematological malignancy affecting the blood and bone marrow. Its prominence in childhood stems from the rapid proliferation of abnormal blood cells, disrupting the delicate balance within the body.
2. Types of Blood Cells
Understanding the roles of
Red blood cells (erythrocytes),
2.platelets (thrombocytes), and
3.white blood cells (leukocytes)
Is fundamental. An imbalance in these cells results in a spectrum of symptoms, from anemia to increased infection susceptibility.
3. Types of Leukemia
. Acute Lymphocytic Leukemia (ALL): Predominant in children.
Acute Myelogenous Leukemia (AML): The second most common type.
Hybrid or Mixed Lineage Leukemia: A rare amalgamation of ALL and AML.
Chronic Myelogenous Leukemia (CML): Uncommon in children.
Chronic Lymphocytic Leukemia (CLL): Extremely rare in pediatric cases.
Juvenile Myelomonocytic Leukemia (JMML): A rare type with unique growth characteristics.
Causes and Risk Factors
1. Causes
The exact etiology of childhood leukemia remains elusive. Genetic mutations in bone marrow cell genes may occur sporadically or, in some instances, be inherited.
2. Risk Factors
Exposure to Radiation.
Particularly high levels.
Inherited Syndromes.
Down syndrome.
Li-Fraumeni syndrome.
Immune System Conditions.
Inherited disorders affecting immune function.
Family History.
Having a sibling with leukemia elevates the risk.
Symptoms of Leukemia in Children
A diverse array of symptoms underscores leukemia’s impact on children, including;
.Pale skin
. Fatigue
.Dizziness
.Headaches
.Shortness of breath
.Frequent infections
.Fever
. Easy bruising
.Bleeding
.Bone or Joint pain, and
.Abdominal swelling.
Diagnosis:
1. Procedures:
.Blood Tests (Complete Blood Count — CBC): Essential for initial assessment.
Bone Marrow Aspiration or Biopsy: Crucial in detecting leukemia cells.
Lab Tests: Precisely determine leukemia type.
Diagnostic Imaging: X-rays, ultrasound,
lymph node biopsy, and
Lumbar puncture offer a comprehensive diagnostic perspective.
2. Classification
Unlike other cancers, leukemia is not staged but rather classified into groups, subtypes, or both based on type and specific characteristics, aiding in targeted treatment approaches.
Treatment Options:
1. Primary Treatments:
Blood Transfusions: Address low blood counts, bleeding, or infections.
Chemotherapy: The mainstay, killing or inhibiting cancer cells.
Radiation Therapy: High-energy X-rays to target and eradicate cancer cells.
Stem Cell Transplant: Involves high-dose chemotherapy followed by stem cell replacement.
Targeted Therapy: Specific medications tailored to combat certain types of leukemia.
Immunotherapy: Enhances the body’s immune system to combat cancer cells.
Complications:
1. Short-term:
Serious Infections: Resulting from compromised immune function.
Severe Bleeding: A consequence of low platelet levels.
Thickened Blood: Accumulation of leukemia cells in the bloodstream.
2. Long-term:
Leukemia Recurrence: A persistent concern.
Development of Other Cancers: A potential consequence of treatment.
Heart and Lung Problems: Arising from the impact of leukemia or its treatment.
Learning Issues and Growth Delays: Impacts on cognitive development and physical growth.
Fertility Problems and Bone Issues: Osteoporosis as a potential long-term complication.
Prevention:
Preventing childhood leukemia remains challenging, with a focus on caution regarding unnecessary exposure to radiation, especially in diagnostic procedures involving pregnant women and children.
Supporting a Child with Leukemia:
1. Ongoing Care:
Regular visits to oncologists and healthcare providers are crucial for monitoring and addressing emerging issues.
2. Balanced Lifestyle:
Managing eating difficulties and encouraging appropriate exercise play a vital role in supporting overall health.
3. Emotional Support:
Seeking counseling or participating in support groups helps both the child and their family navigate the emotional challenges associated with leukemia.
4. Follow-up Appointments:
Attending all scheduled appointments ensures continuous monitoring and timely intervention if complications arise.
When to Contact Healthcare Provider:
Prompt communication with healthcare providers is essential if the child experiences fever, worsening symptoms, new symptoms, or side effects from treatment.
Key Points Summary:
Leukemia necessitates a comprehensive approach, involving diagnosis, tailored treatment, and ongoing monitoring.
Varied symptoms demand timely medical attention for an optimal prognosis.
Treatment modalities, including chemotherapy and stem cell transplant, are tailored to the specific leukemia type.
Complications, both short-term and long-term, underscore the importance of ongoing follow-up care.
Prevention is limited, with a focus on minimizing unnecessary radiation exposure.
Comprehensive support, encompassing medical, emotional, and lifestyle aspects, is essential for the child’s well-being.
Next Steps:
1. Follow-up Care:
Continued regular check-ups and imaging tests remain integral to post-treatment monitoring.
2. Communication:
Maintaining open and transparent communication with healthcare providers ensures timely intervention if issues arise.
3. Research:
Inquiring about ongoing clinical trials or new treatments enables families to stay informed about emerging possibilities.
Conclusion:
Childhood leukemia mandates a collaborative effort from medical professionals, caregivers, and support networks to optimize outcomes and enhance the quality of life for affected children. As the landscape of pediatric oncology evolves, the commitment to advancing treatment options and minimizing the impact of complications remains paramount, offering hope for a brighter future for children navigating the complexities of leukemia.
For Health Sciences Assignment Health,
Email us on;
williamsliason@outlook.com
What is The Process Of Sleep?

Introduction
Sleep is a complex physiological process that encompasses more than merely closing one’s eyes and drifting into unconsciousness. It is an active state of unconsciousness in which the brain, while relatively at rest, remains responsive primarily to internal stimuli. Despite extensive research, the precise purpose of sleep remains incompletely understood. Several prominent theories attempt to elaborate the purpose of sleep, including the Inactivity Theory, Energy Conservation Theory, Restoration Theory, and Brain Plasticity Theory.
Inactivity Theory involves that inactivity during nighttime reduces the risk of predation, offering an evolutionary advantage. This theory suggests that creatures that remained inactive during the night were less likely to fall victim to predators, thereby enhancing survival and reproductive success.
Energy Conservation Theory proposes that the primary function of sleep is to decrease energy demand during periods when it is less efficient to procure food, supported by evidence of a 10% reduction in metabolism during sleep. This theory aligns with the observation that many species exhibit lower metabolic rates during sleep, thereby conserving energy.
Restorative Theory asserts that sleep facilitates the repair and replenishment of cellular components, as evidenced by processes such as muscle repair, tissue growth, protein synthesis, and hormone release occurring predominantly during sleep. This theory is supported by findings that various restorative functions are activated during sleep, promoting physical health and well-being.
Brain Plasticity Theory suggests that sleep is essential for neural reorganization and brain development, particularly in infants and children who require extensive sleep. This theory underscores the role of sleep in cognitive functions, learning, and memory consolidation.
These theories collectively indicate that sleep serves multiple functions, and a combination of these concepts likely explains the necessity of sleep.
Function

Sleep follows a cyclical pattern, alternating between two major phases: Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep. NREM sleep is subdivided into stages 1 through 3, each representing different depths of sleep characterized by unique brain wave patterns, muscle tone, and eye movement patterns. NREM sleep comprises approximately 75–80% of total sleep time, while REM sleep accounts for the remaining 20–25%.
The sleep cycle begins with a short NREM stage 1 phase, progresses through NREM stages 2 and 3, and culminates in REM sleep. This cycle repeats throughout the night, with initial cycles lasting 70–100 minutes and subsequent cycles 90–120 minutes. As the night progresses, the duration of REM sleep increases, eventually comprising up to 30% of the sleep cycle later in the night. Typically, an individual undergoes 4 to 5 sleep cycles per night.
NREM Stage 1: A shallow sleep stage lasting 1–7 minutes, characterized by rhythmical alpha waves (8–13 Hz). This stage represents the transition from wakefulness to sleep, during which the individual can be easily awakened.
NREM Stage 2: A deeper sleep state lasting 10–25 minutes initially, progressing to encompass 50% of the total sleep cycle. EEG recordings during this stage show sleep spindles and K-complexes. Memory consolidation is believed to occur primarily in this stage.
NREM Stage 3: Lasting 20–40 minutes initially, characterized by high-voltage, slow-wave frequency on EEG. This stage, also known as slow-wave sleep (SWS), is crucial for restorative processes.
REM Sleep: Responsible for dreaming, characterized by muscle paralysis (except for the extraocular muscles) and sawtooth waveforms on EEG. REM sleep involves increased brain activity and is essential for cognitive functions such as learning, memory consolidation, and emotional regulation.
Mechanism

The regulation of sleep involves a delicate balance between homeostatic processes and circadian rhythms.
a) Homeostatic Processes
These processes reflect the body’s need for sleep, increasing the pressure to sleep the longer one stays awake. Sleep generation is initiated within the ventrolateral preoptic nucleus (VLPO) of the anterior hypothalamus, which inhibits arousal regions in the brain, including the tuberomammillary nucleus, lateral hypothalamus, locus coeruleus, dorsal raphe, laterodorsally segmental nucleus. Hypocretin (orexin) neurons in the lateral hypothalamus facilitate this process synergistically.
b) Circadian Rhythm
The circadian rhythm, or the internal body clock, regulates the sleep-wake cycle and is influenced by light levels detected by the retina. The hypothalamus, particularly the suprachiasmatic nucleus (SCN),initiates this rhythm. Melatonin, produced by the pineal gland, modulates the circadian rhythm, with levels peaking at night and decreasing during the day. The circadian rhythm typically spans approximately 24.2 hours, and variations in body temperature also play a role, with lower temperatures in the morning and higher temperatures in the evening.
NREM sleep involves a functional disconnection between the brain stem, thalamus, and cortex, maintained by hyperpolarizing GABA neurons. During this phase, corticothalamic neurons signal the thalamus, causing hyperpolarization of thalamic reticular neurons, resulting in delta waves from both thalamic reticular and cortical pyramidal sources.
REM sleep is generated by “REM-on neurons” in the mesencephalic and pontine cholinergic neurons. The pedunculopontine tegmental nucleus and lateral dorsal tegmental neurons trigger desynchronized cortical waveforms. The tonic component of REM sleep is parasympathetically mediated, while the phasic component is sympathetically mediated.
Related Testing
Polysomnography is the primary modality used to study sleep. It is a comprehensive test that includes an electrocardiogram (ECG), electroencephalography (EEG), electrooculography (EOG), electromyography (EMG), and oxygen saturation monitoring.
ECG: Measures the electrical activity of the heart to detect cardiac anomalies such as arrhythmias.
EEG: Non-invasively records brain wave activity to determine sleep stages and detect neurological abnormalities.
EOG: Measures eye movements to differentiate between NREM and REM sleep.
EMG: Assesses muscle activity, particularly in the respiratory muscles and peripheral limbs, to detect excessive movement or muscle tension during sleep.
Oxygen Saturation: Monitors respiratory function to ensure adequate oxygenation during sleep.
Clinical Significance

a) .Insomnia
Insomnia is characterized by difficulty falling or staying asleep and is the most common sleep disorder. It is often related to psychological stressors, poor sleep environments, irregular sleep schedules, or excessive mental, physical, or chemical stimulation. Treatment typically involves cognitive-behavioral therapy (CBT), sleep hygiene practices, and, in some cases, pharmacological interventions.
b) .Obstructive Sleep Apnea (OSA)
OSA is marked by repeated pauses in breathing during sleep due to airway obstruction, often caused by obesity or weak pharyngeal muscles. This condition leads to hypoxia and frequent awakenings, preventing restful sleep. OSA is classified into mild, moderate, and severe based on the frequency of apneic episodes per hour. Treatment options include Continuous Positive Airway Pressure (CPAP) therapy, Bilevel Positive Airway Pressure (BiPAP) therapy, mandibular advancement devices, and surgical interventions such as uvulopalatopharyngoplasty, adenotonsillectomy, and maxillomandibular advancement.
c) .Central Sleep Apnea
Central Sleep Apnea (CSA) results from a failure in the central respiratory drive, leading to diminished breathing effort during sleep. Conditions such as congenital central hypoventilation syndrome (Ondine’s curse) or congestive heart failure can cause CSA. Treatment includes CPAP, BiPAP, Adaptive-servo-ventilation, and medications like acetazolamide or theophylline.
d) .Mixed Sleep Apnea
Mixed Sleep Apnea, also known as Complex Sleep Apnea, involves symptoms of both OSA and CSA. This condition typically manifests when patients with OSA develop CSA symptoms upon treatment with CPAP. Treatment often involves low-pressure CPAP therapy.
d) .Ghrelin-Leptin Abnormalities
Sleep duration significantly influences hunger-regulating hormones, with reduced sleep linked to lower levels of leptin and higher levels of ghrelin. Leptin, produced by adipose cells, inhibits hunger, while ghrelin, produced in the gastrointestinal tract, stimulates appetite. Imbalances in these hormones due to inadequate sleep can increase appetite and contribute to higher body mass index (BMI), potentially leading to obesity. This phenomenon is particularly relevant in patients with OSA, where increased BMI is a risk factor.
e) .Narcolepsy
Narcolepsy is characterized by a loss of orexin (hypocretin) neurons, leading to unstable transitions between sleep and wakefulness. Symptoms include excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations. Narcolepsy type 1 involves a significant loss of orexin neurons, while type 2 is less severe. Treatment focuses on managing symptoms with medications such as stimulants, sodium oxybate, and selective serotonin and norepinephrine reuptake inhibitors (SSRIs and SNRIs), along with lifestyle modifications.
f) .Somnambulism (Sleepwalking)
Somnambulism, or sleepwalking, involves performing activities while in a state of combined sleep and wakefulness. Sleepwalking is associated with increased slow-wave sleep and sleep deprivation, and there is evidence of a genetic predisposition. Treatment includes ensuring a safe sleep environment, improving sleep hygiene, and, in some cases, pharmacological interventions such as benzodiazepines.
Conclusion
Sleep is a physiological process essential for various bodily functions, including energy conservation, cellular repair, brain development, and cognitive function. The precise mechanisms and purposes of sleep remain areas of active research. Understanding the complexities of sleep and its disorders is crucial for promoting overall health and addressing various medical conditions. Ongoing research aims to fully understand the mechanisms of sleep and its broad implications for human health..
Navigating the rigorous demands of medical studies requires support and collaboration. Whether you’re a nursing student, medical doctor, clinical student, pharmacist, or any other medical practitioner, don’t hesitate to seek assistance. Utilize available resources and value teamwork and mentorship.
For personalized support, expert advice, and comprehensive resources, contact Expert Academic Assignment Help at expertassignment46@gmail.com With the right support and dedication, you can achieve your goals and make significant contributions to healthcare.
Alopecia Areata

Introduction
Alopecia areata is a complex autoimmune disease that targets the body’s hair follicles, resulting in patchy hair loss. While medications and therapies offer hope for regrowth, severe cases may pose challenges in responding to treatment. This comprehensive discussion will delve into the various aspects of alopecia areata, from its symptoms and causes to diagnosis, treatment options, prevention, and the psychosocial impact it can have on individuals.
Symptoms and Causes

Alopecia areata manifests as patchy hair loss on various body parts, commonly affecting the scalp. Understanding its classifications, which include total loss (alopecia areata totalis), full-body hair loss (alopecia areata universalis), diffuse thinning (diffuse alopecia areata), and a band of hair loss (ophiasis alopecia areata), provides insights into the diverse ways it can affect individuals.
Certain factors increase the likelihood of developing alopecia areata, such as being a child, having a family history of the condition, or having autoimmune disorders like diabetes, lupus, or thyroid disease. The prevalence of alopecia areata is significant, with nearly 7 million people in the United States affected, and it is the second-most common form of hair loss.
Psychosocial Impact of Alopecia Areata

Beyond its physical effects, alopecia areata can significantly impact an individual’s psychosocial well-being. The emotional toll of experiencing patchy hair loss, potential nail issues, and the uncertainty of its progression can lead to stress, anxiety, and depression. Recognizing these psychological aspects is crucial for holistic management.
Diagnosis and Tests

Diagnosing alopecia areata involves a thorough examination by healthcare providers, considering medical history, the pattern of hair loss, and familial autoimmune conditions. Additional tests, such as scalp examinations, hair analysis, scalp biopsies, and blood tests, may be conducted to confirm the diagnosis.
Management and Treatment

Managing alopecia areata is a nuanced process, and complete cure remains elusive. Treatment options include corticosteroids, administered through injections, oral pills, or topical applications. Minoxidil (Rogaine®), phototherapy, platelet-rich plasma therapy, and topical immunotherapy are among the diverse approaches employed. The unpredictability of alopecia areata necessitates tailored treatment plans, and response times may vary from weeks to months.
Can Alopecia Areata Go Away?
While alopecia areata itself doesn’t vanish, effective treatments can control hair loss. However, severe forms, such as alopecia areata totalis and alopecia areata universalis, pose greater challenges in treatment response.
Prevention and Outlook

Preventing alopecia areata is currently not feasible. The condition tends to have periods of remission and flare-ups throughout an individual’s life. Outlook varies, with mild cases showing remission and more severe forms being less responsive to available treatments.
Living With Alopecia Areata

Coping with alopecia areata involves adopting various cosmetic and protective measures. These include using makeup to conceal hair loss, wearing coverings like wigs or scarves, and protecting the eyes if eyelashes are affected. A balanced diet and vitamin D supplements may contribute to overall health. Avoiding stress, protecting the skin from the elements, and choosing hair products carefully are essential aspects of self-care.
Conclusion
In conclusion, alopecia areata is a multifaceted condition that extends beyond its physical symptoms. Understanding its classifications, causes, and the psychosocial impact on affected individuals is crucial for comprehensive management. While there is no cure, advancements in treatments offer hope for controlling hair loss and stimulating regrowth. A holistic approach, including psychological support and self-care strategies, empowers individuals to navigate life with alopecia areata confidently. As research progresses, further insights into this autoimmune disorder will likely pave the way for more effective interventions, improving the quality of life for those affected by alopecia areata.
We wish you all the best in your studies and knowledge of Alopecia Disease condition.
In case of any challenges during your studies and education journey, don’t hesitate to contact us for a flawless process.
Email us through;
williamsassignmenthelpfredrick@gmail.com
What Makes a PhD Dissertation Different from a Masters Thesis?

Introduction
In the realm of academia, pursuing advanced degrees such as a Master’s or a PhD involves rigorous research and scholarly endeavors. Central to this academic journey are the culminating projects — the Master’s thesis and the PhD dissertation. While often used interchangeably, these two academic works possess distinct characteristics that set them apart. In this comprehensive discussion, we will major into the differences between a PhD dissertation and a Master’s thesis, exploring various aspects including the depth of research, original contribution to knowledge, duration and intensity of study, evaluation and defense process, as well as career implications and academic prestige.
Depth of Research

One of the fundamental disparities between a PhD dissertation and a Master’s thesis lies in the depth of research. A Master’s thesis typically explores a specific topic within a field of study, offering a comprehensive analysis but within a more confined framework. In contrast, a PhD dissertation delves into original research, contributing novel insights or advancing existing knowledge within the chosen discipline. The depth of investigation required for a dissertation is considerably greater, often involving extensive data collection, analysis, and interpretation.
Original Contribution to Knowledge

Building upon the notion of originality, a PhD dissertation is expected to make a significant contribution to the body of knowledge within the respective field. It must demonstrate a unique perspective, innovative methodology, or novel findings that add value to the academic discourse. On the other hand, while a Master’s thesis also involves original research, its contribution may be more incremental or focused on synthesizing existing literature rather than forging new paths of inquiry.
Duration and Intensity of Study

Another factor that distinguishes a PhD dissertation from a Master’s thesis is the duration and intensity of study involved. Pursuing a PhD typically entails a more prolonged and immersive engagement with the research topic, spanning several years of dedicated study and inquiry. The process of conducting original research, analyzing data, and drafting a dissertation demands a substantial commitment of time and effort. In contrast, a Master’s thesis can often be completed within a shorter timeframe, typically ranging from one to two years, depending on the program’s requirements.
Evaluation and Defense Process
The evaluation and defense process also differ between a PhD dissertation and a Master’s thesis. For a PhD dissertation, the candidate must present their research findings to a committee of faculty members or experts in the field. This oral defense involves a rigorous examination of the dissertation’s methodology, results, and conclusions, as well as the candidate’s ability to articulate and defend their research. In contrast, while some Master’s programs may require a thesis defense, the level of scrutiny and formality is often less intense compared to a PhD dissertation defense.
Career Implications and Academic Prestige

Furthermore, the completion of a PhD dissertation carries significant career implications and academic prestige. Attaining a PhD is often regarded as the highest level of academic achievement, opening doors to advanced research positions, teaching opportunities, and leadership roles within academia and industry. A PhD dissertation serves as a hallmark of expertise and scholarly rigor, signaling to the academic community and potential employers the candidate’s ability to conduct independent research at a high level. On the other hand, while a Master’s thesis is a commendable accomplishment in its own right, it may not carry the same weight in terms of career advancement or academic recognition as a PhD dissertation.
Conclusion
In conclusion, the comparison between a PhD dissertation and a Master’s thesis reveals the intricate differences that exist between these two academic endeavors. While both represent significant milestones in academic scholarship, they embody distinct attributes that reflect the depth of research, originality of contribution, and level of academic achievement. Whether seeking thesis vs. dissertation writing help or PhD dissertation assistance, students embarking on these scholarly endeavors can benefit from the guidance and support offered by dissertation writing services. With expert assistance, aspiring scholars can navigate the complexities of research, writing, and presentation, ensuring their academic work meets the highest standards of excellence and scholarly rigor
Understanding the differences between a PhD dissertation and a Master’s thesis is crucial for students embarking on academic research. Expert Academic Assignment Help offers personalized support at every stage of the process, ensuring academic excellence. Reach out at expertassignment46@gmail.com to benefit from expertise and guidance in navigating the complexities of research, writing, and presentation.
Pathophysiology of Asthma

Introduction
Asthma has witnessed a surge in prevalence since the early 1990s, with the USA reporting around 8% prevalence. The disease shows mixed trends globally, with variations in childhood cases attributed to factors like atopy and airway size differences between genders. While a genetic component exists, the inheritance pattern is complex, involving multiple genes, locus heterogeneity, and polygenic inheritance. Atopy and Immunoglobulins(Ig) antibodies targeting specific antigens contribute to asthma, with environmental factors such as house dust mites, animal allergens, and pollutants inducing symptoms. The relationship between air pollution, smoking, obesity, and asthma remains less clear, demanding further research for a comprehensive understanding.
Organ Systems Involved
The lungs, a vital organ system, bear the target of asthma’s impact. Comprising lobes and segments, the bronchial structure, specifically, is the focal point. Initiating zone, extending from the nose to bronchioles, and the respiratory zone, facilitating gas exchange from alveolar duct to alveoli, undergo structural changes due to asthma. The bronchial Anatomy, lined with smooth muscle and elastic fibers, reacts to inflammatory mediators, bronchoconstrictors, and bronchodilators, compromising lung vital functions and use. Inflammation-induced changes, notably a decrease in airway circulation, hence triggering the increase rate or activity of lungs oxygen output with law intake collectively increasing of breathing pattern.
Mechanism
Asthma exacerbations unfold in two phases:
the early phase initiated by Ig antibodies, and
2.late phase characterized by a variety of immune cells. Ig antibodies, stimulated by induction hence bind to mast cells and basophils, releasing histamine, prostaglandins, and leukotrienes, inducing bronchoconstriction. Th2 lymphocytes produce interleukins, sustaining inflammation. The late phase involves immune cells causing further bronchoconstriction and inflammation. Airway hyper reaction, marked by exaggerated bronchoconstriction responses, results from various mechanisms, including increased histamine, airway smooth muscle mass, vagal tone, and intracellular free calcium. Airway remodeling, involving myofibroblast-induced collagen production and epithelial cell transition hence contributes to irreversible airflow obstruction. Hence inability to breath amicably.
Related Testing
Diagnosing asthma involves tests to confirm expiratory airflow limitation, reversible obstruction, and rule out alternative diagnoses. Spirometry, helps assess obstruction severity. Methacholine bronchoprovocation testing determines bronchoconstriction severity. Allergy testing aids in identifying triggers. The diagnostic process ensures accurate asthma identification, facilitating targeted treatment.
Clinical Significance
Clinically, asthma presents with symptoms like wheezing, shortness of breath, and cough, triggered by such as cold air, exercise, and pollutants. Severe cases exhibit tachypnea, tachycardia, or tripod positioning. Recognizing asthma stages; intermittent, mild, moderate, severity guides appropriate treatment. Medications like beta-agonists, glucocorticoids, and muscarinic antagonists aim to relieve bronchoconstriction, inflammation, and airway remodeling. Individualized treatment plans based on severity enhance symptom management.
Conclusion
Understanding the pathophysiology of asthma is crucial for effective management. Genetic factors, environmental triggers, and immune responses involves, resulting in a complex disease with varied clinical presentations. Advances in diagnostic tools and targeted therapies enable clinicians to tailor interventions, emphasizing the importance of early detection and personalized treatment. Further research is essential to reveal the genetic and environmental interactions, paving the way for more effective asthma management strategies.
For Health Sciences Assignment Help;
Email us at;
williamsliason@outlook.com
14 Reasons to become a Doctor

Introduction
Embarking on a career as a doctor is a monumental commitment, requiring an extensive education, unwavering dedication, and resilience. This detailed exploration aims to involve deep into the 14 compelling reasons to choose the noble profession of a medical doctor. Each reason represents a reality of the face and nature of the medical field, elucidating the diverse experiences, responsibilities, and its rewards associated with this esteemed profession.
1.To Help Others
At the core of a doctor’s vocation lies the fundamental responsibility to save lives and enhance the health of their patients. Exploring through challenging moments in patients’ lives, doctors have a unique opportunity to contribute significantly to their recovery and overall well-being. This shown aspect forms the very heart of the medical profession, acting as a profound motivator for those who choose this career path
2. To Explore Science

The steps involving to become a doctor unfolds as a rigorous educational stages across various scientific disciplines. From foundational studies in physics, chemistry, and biology during undergraduate education to the exploration of specialized subjects like pharmacology, anatomy, pathology, and neurology in medical school, doctors engage with an expansive array of scientific knowledge. This profession not only broadens their understanding but also empowers them to apply scientific principles practically in the life of patient care.
3 .To Have Variety in Your Work
A career in medicine is anonymously dynamic, promising a different experience each day. Doctors find themselves at the forefront of a diverse condition of illnesses and injuries, prompting the utilization of various skills and treatments. This extends beyond the medical cases to include interactions with a wide group of people, including patients, families, and colleagues, making the profession continuously admiring and intellectually engaging.
4. To Collaborate
The medical profession thrives on a team-oriented environment, fostering collaboration with nurses, orderlies, administrators, specialists, and pharmacists. This collaborative ethos not only promotes continuous learning as doctors share insights but also serves as a critical for finding collective solutions to complex medical conditions. Effective teamwork emerges as a cornerstone for successful patient care.
5.To Have Purpose in Your Work

Doctors occupy a crucial role in society, profoundly impacting the lives of individuals and their families. By promoting healthier lifestyles and improving patient health, doctors become stewards in contributing to the well-being of their communities. This sense of purpose adds a profound dimension to the daily work of a doctor.
6. To Educate
With their detailed study, doctors become experts of knowledge, which they can share with patients and colleagues as well. Patient education on health management and lifestyle improvements becomes a crucial aspect of a doctor’s responsibilities. Additionally, some doctors have the unique opportunity to contribute to medical education by mentoring and teaching medical students in teaching hospitals to get the best knowledge.
7. To Have Job Security
The universal demand for medical expertise provides doctors with a reassuring sense of job security. Unlike some professions, doctors rarely face concerns about a lack of competition for their skills. This extensive demand allows for greater flexibility when choosing a work location, catering to a broader spectrum of professional opportunities.
8. To Earn a Good Salary
While salaries in the medical field may vary based on factors such as location, experience, and specialization, doctors generally enjoy competitive remuneration coupled with excellent benefits. Specialized fields, particularly surgery, can qualify for even higher incomes. The financial rewards reflect the substantial investment of time and dedication required in pursuing of a medical career.
9. To Be a Leader

A medical career aligns seamlessly with the aspirations of individuals attached towards leadership roles. Physicians and surgeons often find themselves leading large teams of medical personnel, providing vital and main guidance while taking responsibility for patient outcomes. Exceptional leadership skills may present opportunities for doctors to pursue supervisory roles, further enriching their professional journey.
10. To Learn
Medical professionals encounter many challenges facing new medical conditions and dangers regularly. Liaising with experienced physicians and exposure to diverse cases contribute to a continuous learning environment. This commitment to lifelong learning renders a medical career particularly appealing to those with an insatiable passion for acquiring knowledge.
11. To Test Yourself
The study towards being a doctor is worth undertaking, marked by numerous challenges. Overcoming these challenges becomes a crucial for personal and professional growth. Adapting and continuous self-improvement emerge as integrated face of a physician’s journey, contributing to the development of resilient and resourceful medical professionals.
12. To Solve Problems
Critical thinking stands as a cornerstone of medical practice. Physicians accurately analyze symptoms, review patient conditions, and develop precise diagnosis, considering individual’s symptoms and clinical presentation of a disease condition. The expertise skills required in medicine demand cautiousness , structured thinking, and a balanced approach to well being , proofing the analytical competency of doctors.
13. To Contribute to Breakthroughs
Medicine, like many other scientific fields, is in a delicate state of expanding aided by technological advancements. Staying ahead of recent developments is not just a professional necessity but also an opportunity for doctors to contribute actively to breakthroughs in medical science. Those with an admiration towards medical innovation can explore positions in research hospitals, where their contributions may shape the future of healthcare.
14. To Find New Opportunities
Upon completing the rigorous phases of medical school and residency, doctors find themselves at a point of diverse opportunities. The array of choices includes pursuing specialization in a preferred field, opening a private practice, engaging in community work overseas, majoring into scientific research, contributing to public health initiatives, or transitioning into teaching positions, exploiting the versatility of a medical career.
Conclusion:
A career as a doctor is a field attached with diverse experiences, responsibilities, and opportunities. The 14 reasons explored in this discussion shed light on the main rewards and challenges that accompany the study of a medical profession. From the known satisfaction derived from helping others to the demand for knowledge and the potential to actively contribute to important developments, a medical career beckons those with indriven passion, full dedication, and a commitment to the continuous evolution of their professional journey. The resilience, adaptability, and sense of purpose implanted in the medical profession form the foundation of a vocation that extends far beyond the sense of a mere job, defining a passion that motivates those who aspire to make a meaningful impact on the lives of others through the practice of medicine.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
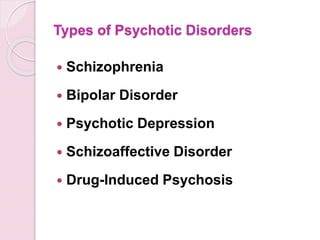
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
10 Tips on How to Study for Medical School

Mastering Time Management
Embarking on the journey of medical school introduces a myriad of challenges, chief among them being the effective management of time. Recognizing the seemingly limited hours in a day, the key lies in adopting a day-by-day approach and establishing a routine that fosters success. Prioritizing tasks, meticulous planning, and incorporating strategic breaks are integral components that enhance both confidence and efficacy in the demanding role of a medical student.
Thorough preparation before the commencement of each class is an impactful strategy. Engaging in pre-class reading enables students to gain a deeper grasp of the lecture’s organization, allowing them to focus on pivotal concepts. This not only facilitates active participation but also positions students to ask informed questions, showcasing a genuine interest and mastery of the subject matter.
2. The Power of Note-Taking
In the intricate landscape of medical school, note-taking emerges as a linchpin for success. Beyond the lecture hall, effective note-taking during readings serves as a powerful tool for managing the deluge of information. Organizing this wealth of material systematically, capturing the essence of each concept, transforms these notes into a potent study guide.
Taking notes not only aids in the recording of information but also serves as an invaluable aid in understanding complex material. The act of transcribing information in one’s own words, essentially explaining concepts to oneself, deepens comprehension and acts as a reinforcing mechanism for challenging subjects.
3. Continuous Learning
Unlike the strategies that sufficed during undergraduate studies, medical school demands a paradigm shift toward continuous learning. The vast curriculum and extensive memorization requirements necessitate a commitment to ongoing, consistent learning. Regular self-testing, routine revisiting of material, and the cultivation of ‘clinical pearls’ — succinct, significant pieces of information — become daily habits that fortify a student’s knowledge base.
The concept of ‘clinical pearls’ transcends the classroom, extending into the professional realm of practicing physicians. As future doctors, adopting these daily learning practices positions students on the trajectory of lifelong learning, a cornerstone of the medical profession.
4. Memory Tricks and Mnemonics
Navigating the labyrinthine landscape of medical knowledge requires innovative memory aids, and mnemonic devices emerge as indispensable allies. Acronyms, memorization phrases, and even the melodic arrangement of information to music serve as effective tools for enhancing memory retention.
Physicians themselves often rely on these mnemonic devices, creating a lexicon of memorable acronyms and phrases that enable them to recall critical information effortlessly. From recalling the signs of a stroke to understanding what passes through the placenta, these memory tricks transform the daunting task of memorization into an engaging and effective learning experience.
5. Know Your Study Sweet Zone
Understanding one’s individual learning strengths is a cornerstone of effective study strategies. Every student possesses a unique learning style, whether through auditory, visual, or other methods. Tailoring study techniques to align with these strengths enhances the overall learning experience and optimizes the absorption of complex medical concepts.
For auditory learners, exploring options such as recording lectures for later review over headphones can be particularly beneficial. On the other hand, visual learners may find sketching and diagramming organ systems to be powerful aids for comprehension. The key to success lies in identifying one’s strengths and leveraging them in the pursuit of medical knowledge.
6. Create Your Study Sanctuary
Amidst the bustling demands of medical school, the creation of a dedicated study space, a ‘study palace,’ becomes imperative. This sanctuary, a space entirely under your control, serves as an oasis of concentration free from distractions. Whether it’s a private room at home or a cubicle in the library, this designated study space becomes the canvas for focused and uninterrupted learning.
Minimizing electronic distractions within this study sanctuary is crucial. In an era of constant connectivity, silencing notifications and carving out dedicated time for focused learning contributes significantly to concentration and overall academic success.
7. Seek Help When Needed
Navigating the complexities of medical school inevitably brings moments of challenge and confusion. During these times, the importance of seeking help cannot be overstated. Whether turning to peers, instructors, or professors, recognizing the need for assistance is a strength, not a weakness.
Approaching professors with questions or seeking clarification on unclear concepts is a proactive step toward academic success. Instructors are not only well-equipped to provide guidance but also appreciate students who show initiative in their learning journey. Additionally, post-exam meetings with professors offer invaluable opportunities for deeper insights, clarification, and personalized study techniques.
8. Form Study Groups
The friendships forged in medical school extend beyond mere camaraderie; they become a cornerstone of academic support. The intensity of studying in medical school is a shared experience among peers. Forming study groups not only provides mutual support but also enhances collaborative learning.
Teaching concepts to fellow students within these study groups serves a dual purpose. Not only does it enhance your own understanding of a concept, but it also creates a dynamic and engaging learning environment. As you collectively navigate the challenges of medical school, the bonds formed in these study groups can last a lifetime.
9. Get Quality Sleep
Pulling an all-nighter to study at the last minute is only going to hurt you in the long run. Your brain needs sleep to retain all the information you’re reviewing. Getting enough sleep each night and keeping a fairly regular schedule is vital to feeling and performing your best.
10. Stay Encouraged
You may be accustomed to school success coming easily, but medical school challenges even the brightest students. No matter how challenging the courses, don’t give up. Remember why you started this journey in the first place!
For Instant Health Science Assignment Help Email: williamsliason@outlook.com
10 Simple Tips for Caring for Your Heart.

The heart, a tireless worker at the core of our well-being, demands our attention and care. As we navigate through Heart Health Month this February, let’s explore ten simple yet impactful tips to ensure our hearts thrive. These practices, ranging from physical activity to laughter and dental hygiene, collectively contribute to a holistic approach to cardiovascular wellness.
1.Cardiovascular Exercise: A Heart’s Best Friend
Engaging in regular cardiovascular or aerobic activities is fundamental for heart health. Following the American Heart Association’s recommendations of 75 minutes of vigorous exercise or 150 minutes of moderate-intensity exercise weekly can significantly boost cardiorespiratory fitness. Activities such as running, cycling, or brisk walking not only elevate heart rate but also enhance overall cardiovascular function. The rhythmic contraction and relaxation of muscles during exercise contribute to improved blood flow and reduced strain on the heart.
2.Embrace a Smoke-Free Lifestyle
Quitting smoking is a paramount step in safeguarding your heart. Smoking damages both the heart and blood vessels, escalating the risk of cardiovascular diseases. Additionally, avoiding second-hand smoke is crucial, as it has been linked to heart attacks and strokes. The harmful chemicals in tobacco smoke lead to the narrowing of blood vessels, increasing the workload on the heart and elevating the risk of high blood pressure.
3.Prioritize Quality Sleep
Adequate sleep, often underestimated, plays a pivotal role in heart health. With at least seven hours of nightly rest, blood pressure lowers, and the body undergoes essential repair processes. Research underscores the correlation between poor sleep and heightened risks of high blood pressure, subsequently increasing the likelihood of heart diseases. Establishing a consistent sleep routine and creating a conducive sleep environment are crucial steps in promoting optimal cardiovascular health.
4.Regular Checkups: A Heart-Healthy Habit
Consistent visits to the doctor for heart health checkups are essential. Assessing risk factors such as diet, blood pressure, cholesterol, and family history enables early detection and management of potential issues. A proactive approach to heart health empowers individuals to make informed lifestyle choices. Regular checkups also provide an opportunity for healthcare professionals to offer personalized guidance on maintaining heart health through tailored interventions.
5.Laughter: The Heart’s Natural Tonic
Laughing, whether through entertainment or social interactions, yields surprising benefits for the heart. The act of laughter reduces artery inflammation, lowers stress hormones, and increases levels of good cholesterol. Integrating humor into daily life becomes a delightful prescription for heart health. Laughter promotes the release of endorphins, the body’s natural feel-good chemicals, which contribute to overall well-being and stress reduction.
6.Dental Hygiene and Heart Connection
Surprising as it may seem, maintaining good dental hygiene contributes to heart health. Studies reveal a link between poor dental health and the presence of bacteria in the bloodstream, impacting heart valves. Simple practices such as regular brushing can significantly decrease the risk of cardiovascular disease. Furthermore, regular dental checkups not only preserve oral health but also serve as a preventive measure against potential cardiovascular complications.
7.Fuel Your Heart with a Healthy Diet
A heart-healthy diet rich in fruits, whole grains, vegetables, and legumes significantly improves blood pressure and cholesterol levels. Steering clear of salty foods and saturated fats is crucial, as they contribute to elevated blood pressure and increased bad cholesterol. Incorporating omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, further supports heart health by reducing inflammation and promoting optimal functioning of blood vessels.
8.Maintaining a Healthy Weight: A Heart’s Delight
Striving for and maintaining a healthy weight is a powerful defense against heart disease and high blood pressure. A combination of a balanced diet, regular exercise, and mindful calorie intake promotes overall well-being and cardiovascular health. Excess weight puts additional strain on the heart, leading to conditions such as hypertension and diabetes. Adopting sustainable lifestyle changes, including portion control and regular physical activity, contributes to achieving and sustaining a healthy weight.
9.Hydration: The Heart’s Elixir
Staying adequately hydrated is a simple yet often overlooked aspect of heart care. Considering the heart’s continuous effort in pumping around 2,000 gallons of blood daily, increased water intake supports its optimal functioning. Dehydration can lead to thicker blood, making the heart work harder to pump blood through the vessels. Maintaining proper hydration levels ensures the efficient transport of nutrients and oxygen to cells, promoting overall cardiovascular health.
10.Stay Active, Break Inactivity
Combatting sedentary lifestyles is crucial in preserving heart health. Incorporating simple changes like taking the stairs, walking, playing with pets, or engaging in household chores helps keep the heart active, reducing the risk of cardiovascular diseases. Prolonged sitting has been associated with various health risks, including obesity and heart disease. Regular physical activity not only supports cardiovascular health but also contributes to weight management and overall well-being.
In conclusion, adopting these ten heart-healthy habits provides a comprehensive approach to cardiovascular wellness. Whether it’s the joyous act of laughter, the discipline of regular exercise, or the mindfulness of a balanced diet, each step contributes to the harmonious symphony of a healthy heart. As we celebrate Heart Health Month, let’s embrace these practices and gift our hearts the care they deserve. Through consistent efforts and lifestyle modifications, we can ensure that our hearts continue to beat with vitality and resilience.
For health Sciences Assignment Help,
Email us on williamsliason@outlook.com
Why do students look for law assignment help?

Law courses demand significant reading and learning to pass tests and complete assignments successfully. Students face immense pressure while mastering various laws and statutes across different law topics such as criminal law, civil law, property law, and constitutional law, among others. The teaching methods employed by law schools add to the challenge. The Case Method, for instance, requires students to analyze a wide array of case proceedings and appellate level judicial opinions. This involves hours of reading and analysis to grasp the minutest details of each case. Additionally, the Socratic Method, where teachers evaluate students’ understanding by asking specific case-related questions in class, adds further pressure.

At Expert Academic Assignment Help, we provide a comprehensive six-step process to ensure high-quality, well-researched assignments free from plagiarism. Our process begins with the initial contact, where students describe their assignment details and deadlines. Once we understand the requirements, we provide a quotation and assign an academic writing expert who is competent in the subject matter. The expert conducts thorough research and gathers all necessary information before writing the assignment. After completion, the assignment undergoes a quality check to ensure it meets all requirements before being delivered to the student.
Moreover, we prioritize addressing any feedback from professors promptly, ensuring that students receive revised assignments as needed. Our efficient process ensures that assignments are completed within a short timeframe, typically within a day, depending on the assignment’s length and complexity.
Our law assignment help covers various fields, including but not limited to:
Administrative Law: Regulating government administrative bodies’ operations.
Contract Law: Governing legally binding agreements between parties.
Environment and Planning Law: Addressing issues related to environmental regulations and land use planning.
Family Law: Dealing with family dynamics, such as divorce and child custody.
Intellectual Property Law: Protecting innovations, ideas, and ownership rights.
Taxation Law: Enforcing taxation laws and regulations.
Constitutional Law: Governing the fundamental principles of government.
Criminal Law: Addressing criminal offenses and penalties.
Business Law: Managing legal issues related to business operations.
Bankruptcy & Insolvency Law: Handling bankruptcy filings and insolvency proceedings.
Property Law: Resolving property ownership and real estate issues.
Tort Law: Addressing legal blunders that cause harm or injury.
Civil Law: Resolving legal complications involving civilians.
Additionally, we assist students with case studies, which serve as self-learning tools to understand legal proceedings and develop a better understanding of the rules used in court.
In conclusion, law assignment help services play a crucial role in supporting students throughout their legal education journey. By providing expert guidance and assistance with assignments, these services alleviate academic pressure and enable students to focus on learning and achieving their academic goals effectively.
During your journey in the school of law, I wish you all the best in the process.
If you encounter any challenges and require guidance or assistance, do not hesitate to contact us at;
williamsassignmenthelpfredrick@gmail.com
-
 expertacademicassignmenthelp reblogged this · 10 months ago
expertacademicassignmenthelp reblogged this · 10 months ago